Abstract
Objective
We studied the efficacy and safety of solifenacin for urinary difficulty in brain lesion from multicenter prospective study.
Method
Eighty patients with brain lesion who visited from 5 multicenter department of rehabilitation medicine from May 2009 to June 2010 were included. Patients were treated with solifenacin 5 mg to 10 mg for 12 weeks. The outcome measure was mean change in daily micturation frequency, daily frequency of incontinence, urgency episodes, and nocturia episodes from baseline to week 12. Patient's attitude to drug was assessed using the BSW Questionnaire (Benefit, Satisfaction and Willingness to Continue Questions).
Results
Sixty-one of 80 were evaluated for effect. All voiding parameters showed significant improvement after 12 weeks of treatment (p<0.05). There was no significant difference in efficacy of solifenacin between ischemic and hemorrhagic stroke. A twenty-two patients experienced 27 adverse events (AE). The most frequent AE were dry mouth (12.5%) and constipation (6.3%). Treatment related adverse events with solifenacin were mainly mild in severity, and only led to discontinuation in 6.3% of patients.
Figures and Tables
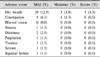
Table 2
Changes of Urination after Solifenacin

Values are mean ± standard deviation. *p<0.01 for the comparison of the value at the follow up time with the baseline value by post Hoc test of Bonferroni F. †p<0.01 for the comparison of the value at the follow up time with the week 4 value by post Hoc test of Bonferroni F. ‡p<0.01 for the comparison of the value at the follow up time with the week 8 value by post Hoc test of Bonferroni F.
References
1. Marinkovic S, Badlani G. Voiding and sexual dysfunction after cerebrovascular accidents. J Urol. 2001. 165:359–370.
2. Gladman JR, Harwood DM, Barer DH. Predicting the outcome of acute stroke. prospective evaluation of five multivariate models and comparison with simple methods. J Neurol Neurosurg Psychiatry. 1992. 55:347–351.
3. Nakayama H, Jørgensen HS, Pedersen PM, Raaschou HO, Olsen TS. Prevalence and risk factors of incontinence after stroke. The Copenhagen Stroke Study. Stroke. 1997. 28:58–62.
4. Patel M, Coshall C, Rudd AG, Wolfe CD. Natural history and effects on 2-year outcomes of urinary incontinence after stroke. Stroke. 2001. 32:122–127.
5. Taub NA, Wolfe CD, Richardson E, Burney PG. Predicting the disability of first-time stroke sufferers at 1 year. 12-month follow-up of a population-based cohort in southeast England. Stroke. 1994. 25:352–357.
6. Brittain KR, Perry SI, Peet SM, Shaw C, Dallosso H, Assassa RP, Williams K, Jagger C, Potter JF, Castleden CM. Prevalence and impact of urinary symptoms among community dwelling stroke survivors. Stroke. 2000. 31:886–891.
7. Chua K, Chuo A, Kong KH. Urinary incontinence after traumatic brain injury. Brain Inj. 2003. 17:469–478.
8. Sakakibara R, Hattori T, Yasuda K, Yamanish T. Micturitional disturbance after acute hemispheric stroke: analysis of the lesion site by CT and MRI. J Neurol Sci. 1996. 137:47–56.
9. Han JY, Choo MS. Drug treatment for lower urinary tract symptoms. J Korean Med Assoc. 2011. 54:637–645.
10. Chapple CR, Martinez-Garcia R, Selvaggi L, Toozs-Hobson P, Warnack W, Drogendijk T, Wright DM, Bolodeoku J. STAR study group. A comparison of the efficacy and tolerability of solifenacin succinate and extended release tolterodine at treating overactive bladder syndrome: results of the STAR trial. Eur Urol. 2005. 48:464–470.
11. Haab F, Cardozo L, Chapple C, Ridder AM. Solifenacin Study Group. Long-term open-label solifenacin treatment associated with persistence with therapy in patients with overactive bladder syndrome. Eur Urol. 2005. 47:376–384.
12. Michel MC, de la Rosette JJMCH. Role of muscarinic receptor antagonists in urgency and nocturia. BJU Int. 2005. 96:37–42.
13. Pleil AM, Coyne KS, Reese PR, Jumadilova Z, Rovner ES, Kelleher CJ. The validation of patient-rated global assessments of treatment benefit, satisfaction, and willingness to continue--the BSW. Value Health. 2005. 8:Suppl 1. S25–S34.
14. Cardozo L, Hessdorfer E, Milani R, Arano P, Dewilde L, Slack M, Drogendijk T, Wright M, Bolodeoku J. Solifenacin in the treatment of urgency and other symptoms of overactive bladder: results from a randomized, double-blind, placebo-controlled, rising-dose trial. BJU Int. 2008. 102:1120–1127.
15. Choo MS, Lee JZ, Lee JB, Jung HC, Lee KS, Kim JC, Seo JT, Paick JS, Kim HJ, Na YG, Lee JG. Efficacy and safety of solifenacin succinate in Korean patients with overactive bladder: a randomised, prospective, double-blind, multicentre study. Int J Clin Pract. 2008. 62:1675–1683.
16. de Groat WC. A neurologic basis for the overactive bladder. Urology. 1997. 50:36–52.
17. Sibley GN. The physiological response of the detrusor muscle to experimental bladder outflow obstruction in the pig. Br J Urol. 1987. 60:332–336.




 PDF
PDF ePub
ePub Citation
Citation Print
Print






 XML Download
XML Download