Abstract
The purpose of this study is to clinically evaluate and report the effectiveness of radiofrequency microdebrider (Topaz, ArthroCare) treatment in lateral epicondylitis patients. From March to July 2003, 15 patients of 17 elbows were prospectively followed. Candidate for the treatment were lateral epicondylitis patients who had symptom more than 6 month and failed to respond to conservative treatment, including medication (non-steroidal anti-inflammatory drugs), external gel or patch, and steroid injections. All patient who scored greater than grade 3 (fair) on the Self-administered Roles and Maudsley Pain (SRMP) score were selected for the procedure. All procedure was done using local anesthesia and ArthroCare microdebrider by a single surgeon. Postoperative assessments were done on postoperative period 12 month of two previous subjective scores and a simple functional assessment asking better, same, or worst function after the procedure. Mean age of the patients was 45 years old. Mean symptom duration before the procedure was 22.6 months. After the procedure, the mean Pain Visual Analogue Scale improved from 7.3 (range, 5–9; standard deviation [SD], 1.2) preoperatively to 3.7 (range, 0–7; SD, 2.1) postoperatively (p< 0.001). After the procedure, five elbows showed no rating improvement, in seven elbows 1 level improvement, in four elbows 2 level improvement, and in one elbow 3 level improvement. Overall, 71% (12/17) showed improvement after the procedure according to the SRMP score rating. Although 29% (5/17) of the elbow showed no improvement on SRMP score, among them five elbows were still rated decrease in Pain Visual Analogue Scale.
Lateral epicondylitis or tennis elbow is a commonly encountered problem in orthopedic practice. Although the exact etiology still has not been revealed, the most commonly accepted theory has been microscopic rupture with formation of reparative tissue in the extensor carpi radialis brevis (ECRB) origin on the lateral epicondyle1. Most patients respond well to conservative treatment. And yet not a single treatment modality has been effective in curing this common and cumbersome disease. A broad spectrum of conservative treatment includes rest, medication, injections, braces, and extracorporeal shock wave therapy (ESWT). In addition, numerous surgical procedures, open, percutaneous, and arthroscopic, were introduced123456.
The terms epicondylitis and tendinitis are used commonly to describe tennis elbow; however, histopathologic studies have shown that tennis elbow is not an inflammatory condition. Rather, tennis elbow is a fibroblastic and vascular response called angiofibroblastic degeneration now more commonly known as tendinosis78. As hypovascularity has been proposed to be a factor in tendinosis, bipolar plasma-induced radiofrequency (Coblation Technology; ArthroCare, Sunnyvale, CA, USA) has been postulated to induce tissue healing through a controlled inflammatory response. In other words, although the exact mechanism is not known, histological evidence shows neo-vessel formation and an increase in angiogenic markers inducing increased tissue vascularity demonstrated after Coblation therapy.
The aim of this study was to report the early clinical outcome of lateral epicondylitis patients who have been treated with Coblation radiofrequency microdebrider.
From March to July 2003, 15 consecutive patients of 17 elbows were prospectively followed. A proper Institutional Review Board approval (IRB No. 2017-11-130) was granted. Candidates for the treatment were lateral epicondylitis patients who had symptom more than 6 month and failed to respond to conservative treatment, including medication (non-steroidal anti-inflammatory drugs), external gel or patch, and steroid injections. A thorough medical history and clinical evaluation were performed by a single surgeon (JCY) and X-rays were performed to rule out any associated pathologies. We excluded any patients who had combined elbow pathology such as elbow fracture, osteoarthritis, osteochondritis dissecans, and stiffness. Also, any patients who were subject to compensation or litigation were excluded.
Prior to the procedure, all patients were assessed by two subjective scoring systems: Pain Visual Analogue Scale (PVAS) and Self-administered Roles and Maudsley Pain (SRMP)9 score for lateral epicondylitis (Table 1). All patients who scored greater than grade 3 (fair) on the SRMP score were selected for the procedure. Under local anesthesia, the surgical procedure was followed according to the Coblation surgical guideline.
A small incision of approximately of 2 cm was performed over the marked symptomatic areas. The paratenon was incised where indicated to expose the involved tendon. An ArthroCare device (model Topaz) was connected to an ArthroCare system 2000 generator with a voltage setting of 4 (175V RMS) (Fig. 1). A sterile isotonic saline line was connected to the saline port of the device, and flow set to 1 drop per second. After localization of the area to be treated, the device was placed on the tendon, perpendicular to its surface and activated for 0.5 second with a pressure of about 5–8 g (Fig. 2). Treatment was performed at 5-mm distance intervals on and around the symptomatic tendon area, creating a grid-like pattern. All patients received identical surgical treatment by a single surgeon (JCY). Patients were allowed tolerable range of motion exercise immediately after the procedure. We only did stretching of extensor and flexor from the wrist, postoperatively. Two weeks postoperatively, we did no restriction on strengthening. Postoperative assessments were done on postoperative period 12 month of two previous subjective scores and a simple functional assessment asking better, same, or worst function after the procedure.
All statistical analysis was performed with the significance level set at p=0.05 and using the software SPSS ver. 18.0 (SPSS Inc., Chicago, IL, USA). Wilcoxon signed-rank test was performed for comparison of pre- and postoperative PVAS and SRMP score.
There were 14 females and one male. The involved elbows were 17, eight right sides, five left sides and two bilateral. In 16 elbows, dominant arm was involved. Mean age of patient was 45 years (range, 34–61 years; standard deviation [SD], 7.1 years). Mean symptom duration before the procedure was 22.6 months (range, 7–48 months; SD, 14.2 months). Mean number of steroid injection prior to the surgical procedure was 1.3 (range, 0–3; SD, 1.2). Of the 17 elbows, only four patients participated in sports activity, which was badminton, table tennis, and bowling (Table 2).
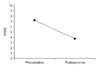
After the procedure, the mean PVAS improved from 7.3 (range, 5–9; SD, 1.2) preoperatively to 3.7 (range, 0–7; SD, 2.1) postoperatively (Fig. 3). Decrease in scale showed statistically significant difference (p<0.001). Prior to procedure, SRMP score rated fair in eight elbows and poor in nine elbows. After the procedure, six elbows showed no rating improvement, in five elbows 1 level improvement in six elbows 2 level improvement, and in one elbow 3 level improvement (Fig. 4). Overall, 71% (12/17) showed improvement after the procedure according to the SRMP score rating. Although 29% of the elbow (5/17) showed no improvement on SRMP score, among them four elbows were still rated decrease in PVAS. The simple function questionnaire that we asked resulted: better function in eight of 17 of the patient (47.1%). No adverse event or complication has been observed to this date.
Coblation technology is thought to be fundamentally different from traditional electrocautery and thermal devices. In appropriate conditions, a small vapor layer forms on the active electrode of the device, in which the electric field breakdown the vapor to produce a plasma. This plasma is itself an electrically conducting gas consisting of free electrons, ions and neutral chemical radicals, and other neutral species. The particles contained in this plasma have sufficient energy to break down most bonds found in soft tissue molecules10. This novel method of tissue removal not only have the effect of volumetric removal of tissue111213 but also seem to have some response in tissue healing and improving the clinical outcomes.
Lateral epicondylitis or tennis elbow is a common disease with relatively good prognosis in most patients. Large number of random study on tennis players revealed that half of the players experienced symptoms of characteristic tennis elbow at one time or another. Of this group, half noted minor symptoms with a duration of less than 6 months, and the rest had had major symptoms with an average duration of 2 and a half years14. To those patients who have had continuous pain and dysfunction seems to have severe impairment even to perform basic daily activities. These patients are candidate for more aggressive and invasive treatment modalities, such as, autologous blood injection, ESWT, Coblation, and surgery.
Injection of autologous blood is thought to provide the necessary cellular and humoral mediators to induce a healing cascade15. This theory was proposed after observing some healing potential after some traumatic insult and bleeding to the affected area516. Some researchers1517 think that healing process occurs either by inflammatory response resulted from local tissue irritation during the metabolism of the blood or from cell-mediated factors within the blood. Merolla et al.18 reported that autologous platelet rich plasma injections are effective in the short and medium term, but patients experienced a significant worsening of pain at 2 years. Unlu et al.19 reported that platelet rich plasma injections in the treatment of chronic tendinopathy resulted a moderate improvement (>50%) in pain symptoms was observed in most of the patients in 6 weeks and 6 months follow-up.
ESWT for treatment of insertion tendinopathies was first introduced in Germany and Austria a decade ago and large numbers of patients have received this treatment. It is proposed to have the anti-nociceptive effect20, but the electrophysiological pathways and molecular mechanisms are obscure. The overall success rates are reported as low as 25% to more than 90%212223. Well organized randomized multicenter study by Haake et al.23 and different study by speed et al.22 showed no relevant difference in the clinical success rate compared with that in a placebo therapy group. Furthermore, they recommended disuse of ESWT for chronic lateral epicondylitis. But, Koksal et al.24 showed ESWT is equally effective in the treatment of acute (<3 months) and chronic (>6 months) lateral epicondylitis.
There have been many attempts to relieve resistant lateral epicondylitis by surgery, open or arthroscopic123456. Historically, surgical release or slide of the extensor aponeurosis, often combined with orbicular ligaments in presumption that the force generators are weakened thereby decreasing stress to the sensitized tissues2. Pierce et al.25 compared outcome after conventional open, percutaneous, and arthroscopic release of the common extensor origin for lateral epicondylitis. They found that all three methods were highly effective for the treatment of tendinosis. Functional outcomes of open and arthroscopic releases may be superior to those of percutaneous release.
Coblation controlled cold ablation or radiofrequency electrosurgical ablation, which was originally developed for cartilage ablation in arthroscopic surgery, is now being utilized in many fields: dermatology for skin resurfacing, otolaryngology for tonsillectomy and others, in cardiology for to improve myocardial perfusion, and so forth11121326. This bipolar, multi-electrode technology has advantages mainly in bipolar cautery, less pain, and cold ablation creation of an ionized vapor or plasma level resulting in cellular disintegration at a lower temperature (100℃) than the Bovie (600℃). Our results showed that it might have some effect on pain relief and SRMP score. Considering the natural course of disease in which half of the chronic tennis elbow patients improve with only conservative treatment. Although our case was small and had short-term follow-up, we feel that the benefit weighs less over the trouble patient has go through.
Recent literature reported about good results of radiofrequency microtenotomy. Meknas et al.27 reported that in prospective, randomized trial with a medium-term (5–7 years) follow-up, the results were similar after surgical release and microtenotomy in patients with recalcitrant lateral epicondylitis. PVAS at the medium-term follow-up in both open and microtenotomy groups significantly decreased compared with the preoperative assessment (p<0.005). The Mayo Elbow Performance Score increased significantly in both groups (p<0.01).
Radiofrequency microtenotomy has advantage of a low complication rate and a short operation time. In our series, the procedure took about 15–20 minutes from skin to skin. And, the tourniquet time took about 10 minutes or less. About complications, there is controversy, but there are some reports that the complications are more likely to occur after open or arthroscopic release in resistant lateral epicondylitis patients. Pierce et al.25 reported that patients who underwent open release technique were more likely to be diagnosed with a superficial wound infection than patients who underwent an arthroscopic ECRB release (0.71% vs. 0%, p=0.04). Pomerantz28 reported overall complication rate in surgical release procedure was 3.3%. For open procedures, it was 4.3%, percutaneous procedures 1.9%, and arthroscopic procedures 1.1%. In higher-level studies directly comparing modalities, the complication rates were 1.3%, 0%, and 1.2%, respectively. However, Tasto et al.29 reported that no complications were reported after radiofrequency-microtenotomy. The results are durable with successful outcomes observed at 9 years after surgery. Meknas30 showed no complications or adverse effects in the radiofrequency microtenotomy group. Compared with the open release procedure, the operation time for radiofrequency microtenotomy is short, simple, and safe.
Several drawbacks of this paper are as follows. First, it is not a large number to draw any concrete conclusions. Second, although the exclusion criteria was strictly selected, other parametric variables or risk factors for tendon overuse7 such as pre- and postoperative work levels, activity levels, and other treatment modalities which was undertaken before and after the procedure, were not accounted in this study. Third, diagnostic tools such as ultrasound or magnetic resonance imaging were not used for all patients to identify other accompanying problems such as posterior interosseous nerve entrapment syndrome, varus instability. However, patients had typical symptoms like a focal tenderness and provocateur pain on resisted wrist extension for a long duration. So, we think it was possible to reduce misdiagnosis due to thorough physical examination, the sufficient medical history taking and symptoms during follow up periods. Fourth, immediate postoperative pain and function follow-up, such as postoperative 3, 6, and 9 month was not performed. Fifth, we did not use objective evaluation parameter such as the grip power. Sixth, no randomization or control was given.
In conclusion, microdebridement procedure on the common extensor tendon for the patients who has retractable lateral epicondylitis showed clinical improvement evaluated with the PVAS score and SMRP score at 1-year follow-up after the procedure.
Figures and Tables
 | Fig. 1(A) ArthroCare timer and (B) Topaz device. This additional equipment is needed with the conventional ArthroCare device. |
 | Fig. 2The pathologic tendon is localized and the Topaz device is inserted perpendicular to the tendon. It is activated 0.5 second with 5-mm distance intervals with grid-like pattern. |
References
1. Nirschl RP, Pettrone FA. Tennis elbo: the surgical treatment of lateral epicondylitis. J Bone Joint Surg Am. 1979; 61:832–839.
2. Goldie I. Epicondylitis lateralis humeri (epicondylalgia or tennis elbow): a pathogenetical study. Acta Chir Scand Suppl. 1964; 57:Suppl 339. 1+.
3. Almquist EE, Necking L, Bach AW. Epicondylar resection with anconeus muscle transfer for chronic lateral epicondylitis. J Hand Surg Am. 1998; 23:723–731.
4. Coonrad RW, Hooper WR. Tennis elbow: its course, natural history, conservative and surgical management. J Bone Joint Surg Am. 1973; 55:1177–1182.
5. Baumgard SH, Schwartz DR. Percutaneous release of the epicondylar muscles for humeral epicondylitis. Am J Sports Med. 1982; 10:233–236.
6. Owens BD, Murphy KP, Kuklo TR. Arthroscopic release for lateral epicondylitis. Arthroscopy. 2001; 17:582–587.
7. Nirschl RP, Ashman ES. Tennis elbow tendinosis (epicondylitis). Instr Course Lect. 2004; 53:587–598.
8. Labelle H, Guibert R, Joncas J, Newman N, Fallaha M, Rivard CH. Lack of scientific evidence for the treatment of lateral epicondylitis of the elbow: an attempted meta-analysis. J Bone Joint Surg Br. 1992; 74:646–651.
9. Roles NC, Maudsley RH. Radial tunnel syndrome: resistant tennis elbow as a nerve entrapment. J Bone Joint Surg Br. 1972; 54:499–508.
10. Stalder KR, Woloszko J, Brown IG, Smith CD. Repetitive plasma discharges in saline solutions. Appl Phys Lett. 2002; 79:4503–4505.
11. Grekin RC, Tope WD, Yarborough JM Jr, et al. Electrosurgical facial resurfacing: a prospective multicenter study of efficacy and safety. Arch Dermatol. 2000; 136:1309–1316.
12. Bortnick DP. Plastic Surgery Educational Foundation DATA Committee. Coblation: an emerging technology and new technique for soft-tissue surgery. Plast Reconstr Surg. 2001; 107:614–615.
13. Hall DJ, Littlefield PD, Birkmire-Peters DP, Holtel MR. Radiofrequency ablation versus electrocautery in tonsillectomy. Otolaryngol Head Neck Surg. 2004; 130:300–305.
14. Nirschl RP. Tennis elbow. Orthop Clin North Am. 1973; 4:787–800.
15. Edwards SG, Calandruccio JH. Autologous blood injections for refractory lateral epicondylitis. J Hand Surg Am. 2003; 28:272–278.
16. Wadsworth TG. Lateral epicondylitis (tennis elbow). Lancet. 1972; 1:959–960.
17. Hildebrand KA, Woo SL, Smith DW, et al. The effects of platelet-derived growth factor-BB on healing of the rabbit medial collateral ligament: an in vivo study. Am J Sports Med. 1998; 26:549–554.
18. Merolla G, Dellabiancia F, Ricci A, et al. Arthroscopic debridement versus platelet-rich plasma injection: a prospective, randomized, comparative study of chronic lateral epicondylitis with a nearly 2-year follow-up. Arthroscopy. 2017; 33:1320–1329.
19. Unlu MC, Kivrak A, Kayaalp ME, Birsel O, Akgun I. Peritendinous injection of platelet-rich plasma to treat tendinopathy: a retrospective review. Acta Orthop Traumatol Turc. 2017; 11. 03. [Epub]. DOI: 10.1016/j.aott.2017.10.003.
20. Haake M, Thon A, Bette M. Absence of spinal response to extracorporeal shock waves on the endogenous opioid systems in the rat. Ultrasound Med Biol. 2001; 27:279–284.
21. Wang CJ, Chen HS. Shock wave therapy for patients with lateral epicondylitis of the elbow: a one- to two-year followup study. Am J Sports Med. 2002; 30:422–425.
22. Speed CA, Nichols D, Richards C, et al. Extracorporeal shock wave therapy for lateral epicondylitis: a double blind randomised controlled trial. J Orthop Res. 2002; 20:895–898.
23. Haake M, Konig IR, Decker T, et al. Extracorporeal shock wave therapy in the treatment of lateral epicondylitis: a randomized multicenter trial. J Bone Joint Surg Am. 2002; 84:1982–1991.
24. Koksal I, Guler O, Mahirogullar M, Mutlu S, Cakmak S, Aksahin E. Comparison of extracorporeal shock wave therapy in acute and chronic lateral epicondylitis. Acta Orthop Traumatol Turc. 2015; 49:465–470.
25. Pierce TP, Issa K, Gilbert BT, et al. A systematic review of tennis elbow surgery: open versus arthroscopic versus percutaneous release of the common extensor origin. Arthroscopy. 2017; 33:1260–1268.e2.
26. Kantor B, McKenna CJ, Caccitolo JA, et al. Transmyocardial and percutaneous myocardial revascularization: current and future role in the treatment of coronary artery disease. Mayo Clin Proc. 1999; 74:585–592.
27. Meknas K, Al Hassoni TN, Odden-Miland A, Castillejo M, Kartus J. Medium-term results after treatment of recalcitrant lateral epicondylitis: a prospective, randomized study comparing open release and radiofrequency microtenotomy. Orthop J Sports Med. 2013; 1:2325967113505433.
28. Pomerantz ML. Complications of lateral epicondylar release. Orthop Clin North Am. 2016; 47:445–469.
29. Tasto JP, Richmond JM, Cummings JR, Hardesty R, Amiel D. Radiofrequency microtenotomy for elbow epicondylitis: midterm results. Am J Orthop (Belle Mead NJ). 2016; 45:29–33.
30. Meknas K. Re: radiofrequency microtenotomy: a promising method for treatment of recalcitrant lateral epicondylitis. Am J Sports Med. 2008; 36:e2–e3.




 PDF
PDF ePub
ePub Citation
Citation Print
Print





 XML Download
XML Download