Abstract
The purpose of remnant preserving technique in anterior cruciate ligament (ACL) reconstruction is to preserve mechanoreceptor and accelerate revascularization. In this study, we compared a group who underwent remnant preserving technique using Achilles tendon allograft with the other group of conventional ACL reconstruction in terms of proprioception, kinematic analysis, knee strength test and dynamic postural stability. Twenty-four patients were followed up for longer than 12 months after ACL reconstruction. They were separated into two groups; remnant preserving group (n=12) and non-remnant group (n=12). Proprioception test was conducted through joint position sense (JPS) and threshold to detection of passive motion. The remnant preserving group showed significantly less difference from the normal side than the non-remnant group. In kinematic analysis, there was statistically significant difference in peak flexion angle during the swing phase. However the 60° JPS, knee strength test, performance capacity test and dynamic postural stability did not showed the significant difference. Remnant preserving technique of ACL reconstruction was meaningful in preserving proprioception and the result showed akin to the unaffected gait.
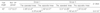
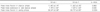
Figures and Tables
Fig. 1
Remnant preserving technique. (A) Femoral tunnel was positioned at the proximal part of bifurcate ridge preserving the remnant of anterior cruciate ligament (ACL). (B) Allograft was passed through beside the remnant of ACL. (C) Postoperative radiographs. *Remnant of ACL; †Achilles thedon allograft.

Fig. 2
The method of measured joint position sense. (A) Put on Lokomat (Hocoma AG). (B) Flow diagram for the measured joint position sense. The subject is placed into the target angle by the Lokomat and is asked to memorize the angle. After being moved away from the target, the subject move the leg back to the target angle.

Fig. 3
Primus-RS, BTE. Physical therapy equipment for multi-joint testing, orthopedic rehab, neuromuscular re-education, and advanced musculoskeletal athletic training of the upper & lower extremities and the core.

Fig. 4
Biodex Stability System (BSS, Biodex Medical Systems Inc.) Consists of a movable balance platform that provides up to 20° of surface tilt in a 360° range of motion. The platform is interfaced with computer software that enables the device to serve as an objective assessment of balance.

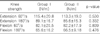
Fig. 5
Knee kinematics at average of each group. Group I was similar to the normal kinematics of the knee joint.
References
1. Bray RC, Dandy DJ. Meniscal lesions and chronic anterior cruciate ligament deficiency. Meniscal tears occurring before and after reconstruction. J Bone Joint Surg Br. 1989. 71:128–130.
2. Georgoulis AD, Pappa L, Moebius U, et al. The presence of proprioceptive mechanoreceptors in the remnants of the ruptured ACL as a possible source of re-innervation of the ACL autograft. Knee Surg Sports Traumatol Arthrosc. 2001. 9:364–368.
3. Shino K, Inoue M, Horibe S, Nakata K, Maeda A, Ono K. Surface blood flow and histology of human anterior cruciate ligament allografts. Arthroscopy. 1991. 7:171–176.
4. Barrett DS. Proprioception and function after anterior cruciate reconstruction. J Bone Joint Surg Br. 1991. 73:833–837.
5. Reider B, Arcand MA, Diehl LH, et al. Proprioception of the knee before and after anterior cruciate ligament reconstruction. Arthroscopy. 2003. 19:2–12.
6. Lee BI, Min KD, Yoon ES, Kim JB, Choi HS, Lee DH. Mechanoreceptors in the remnants of ruptured anterior cruciate ligaments in human knees. J Korean Orthop Assoc. 2006. 41:811–817.
7. Jeong HJ, Shin HK, Lee J, Choi K, Jeon B. Preserving remnant tissue in arthroscopic ACL reconstruction using achilles tendon allograft. J Korean Knee Soc. 2010. 22:215–221.
8. Adachi N, Ochi M, Uchio Y, Iwasa J, Ryoke K, Kuriwaka M. Mechanoreceptors in the anterior cruciate ligament contribute to the joint position sense. Acta Orthop Scand. 2002. 73:330–334.
9. Shelbourne KD, Nitz P. Accelerated rehabilitation after anterior cruciate ligament reconstruction. Am J Sports Med. 1990. 18:292–299.
10. Linn RM, Fischer DA, Smith JP, Burstein DB, Quick DC. Achilles tendon allograft reconstruction of the anterior cruciate ligament-deficient knee. Am J Sports Med. 1993. 21:825–831.
11. Noyes FR, Barber-Westin SD. Reconstruction of the anterior cruciate ligament with human allograft. Comparison of early and later results. J Bone Joint Surg Am. 1996. 78:524–537.
12. Jackson DW, Windler GE, Simon TM. Intraarticular reaction associated with the use of freeze-dried, ethylene oxide-sterilized bone-patella tendon-bone allografts in the reconstruction of the anterior cruciate ligament. Am J Sports Med. 1990. 18:1–10.
13. Roberts TS, Drez D Jr, McCarthy W, Paine R. Anterior cruciate ligament reconstruction using freeze-dried, ethylene oxide-sterilized, bone-patellar tendon-bone allografts. Two year results in thirty-six patients. Am J Sports Med. 1991. 19:35–41.
14. Peterson RK, Shelton WR, Bomboy AL. Allograft versus autograft patellar tendon anterior cruciate ligament reconstruction: A 5-year follow-up. Arthroscopy. 2001. 17:9–13.
15. Chun CH, Han HJ, Lee BC, Kim DC, Yang JH. Histologic findings of anterior cruciate ligament reconstruction with Achilles allograft. Clin Orthop Relat Res. 2004. (421):273–276.
16. Schultz RA, Miller DC, Kerr CS, Micheli L. Mechanoreceptors in human cruciate ligaments. A histological study. J Bone Joint Surg Am. 1984. 66:1072–1076.
17. Miura K, Ishibashi Y, Tsuda E, Okamura Y, Otsuka H, Toh S. The effect of local and general fatigue on knee proprioception. Arthroscopy. 2004. 20:414–418.
18. Tsuda E, Okamura Y, Otsuka H, Komatsu T, Tokuya S. Direct evidence of the anterior cruciate ligament-hamstring reflex arc in humans. Am J Sports Med. 2001. 29:83–87.
19. Ochi M, Iwasa J, Uchio Y, Adachi N, Sumen Y. The regeneration of sensory neurones in the reconstruction of the anterior cruciate ligament. J Bone Joint Surg Br. 1999. 81:902–906.
20. Fremerey RW, Lobenhoffer P, Zeichen J, Skutek M, Bosch U, Tscherne H. Proprioception after rehabilitation and reconstruction in knees with deficiency of the anterior cruciate ligament: a prospective, longitudinal study. J Bone Joint Surg Br. 2000. 82:801–806.
21. Corrigan JP, Cashman WF, Brady MP. Proprioception in the cruciate deficient knee. J Bone Joint Surg Br. 1992. 74:247–250.
22. Oh SJ, Yang SJ, Ha JK, Seo JG, Choi JY, Kim JG. The effectiveness of joint position sense test in evaluating the proprioceptive function after anterior cruciate ligament reconstruction. Korean J Sports Med. 2011. 29:83–88.
23. Refshauge KM, Chan R, Taylor JL, McCloskey DI. Detection of movements imposed on human hip, knee, ankle and toe joints. J Physiol. 1995. 488(Pt 1):231–241.
24. Collins DF, Refshauge KM, Todd G, Gandevia SC. Cutaneous receptors contribute to kinesthesia at the index finger, elbow, and knee. J Neurophysiol. 2005. 94:1699–1706.
25. Domingo A, Marriott E, de Grave RB, Lam T. Quantifying lower limb joint position sense using a robotic exoskeleton: a pilot study. IEEE Int Conf Rehabil Robot. 2011. 2011:5975455.
26. Kim DK, Park WH. Proprioceptive and strength comparison of remnant preserved versus conventional anterior cruciate ligament reconstruction. Korean J Sports Med. 2011. 99–104.
27. Berchuck M, Andriacchi TP, Bach BR, Reider B. Gait adaptations by patients who have a deficient anterior cruciate ligament. J Bone Joint Surg Am. 1990. 72:871–877.
28. Ernst GP, Saliba E, Diduch DR, Hurwitz SR, Ball DW. Lower extremity compensations following anterior cruciate ligament reconstruction. Phys Ther. 2000. 80:251–260.
29. Timoney JM, Inman WS, Quesada PM, et al. Return of normal gait patterns after anterior cruciate ligament reconstruction. Am J Sports Med. 1993. 21:887–889.




 PDF
PDF ePub
ePub Citation
Citation Print
Print







 XML Download
XML Download