Abstract
PURPOSE
The goal of this study was to compare the adhesion of Candida albicans to the surfaces of CAD/CAM and conventionally fabricated complete denture bases.
MATERIALS AND METHODS
Twenty discs of acrylic resin poly (methyl methacrylate) were fabricated with CAD/CAM and conventional procedures (heat-polymerized acrylic resin). The specimens were divided into two groups: 10 discs were fabricated using the CAD/CAM procedure (Wieland Digital Denture Ivoclar Vivadent), and 10 discs were fabricated using a conventional flasking and pressure-pack technique. Candida colonization was performed on all the specimens using four Candida albicans isolates. The difference in Candida albicans adhesion on the discs was evaluated. The number of adherent yeast cells was calculated by the colony-forming units (CFU) and by Fluorescence microscopy.
RESULTS
There was a significant difference in the adhesion of Candida albicans to the complete denture bases created with CAD/CAM and the adhesion to those created with the conventional procedure. The CAD/CAM denture bases exhibited less adhesion of Candida albicans than did the denture bases created with the conventional procedure (P<.05).
CONCLUSION
The CAD/CAM procedure for fabricating complete dentures showed promising potential for reducing the adherence of Candida to the denture base surface. Clinical Implications. Complete dentures made with the CAD/CAM procedure might decrease the incidence of denture stomatitis compared with conventional dentures.
Edentulism is a “debilitating and irreversible condition and is described as the final marker of disease burden for oral health.”12 Among older adults, edentulism is considered one of the most prevalent condition worldwide3 although the percentage of tooth loss has decreased in recent years.4 In the U.S., the prevalence of edentulism is 15% in patients between the ages of 65 and 74 years old and 22% in patients older than 75 years according to the National Health and Nutrition Examination Survey.3 Emami et al.2 reported that the majority of edentulous patients wear one or two complete dentures. The use of removable prostheses has increased due to the increasing number of older patients, who are the primary wearers of dentures, in the general population.4 Being edentulous influences oral health and general well-being.2 The effects on oral health include impaired masticatory efficiency and denture-related oral lesions, such as angular cheilitis, traumatic ulcers and denture stomatitis (DS).56 DS is an inflammation of the mucosa underlying a removable prosthesis.7 Shulman et al.8 conducted a study in the U.S. and found that the prevalence of DS among denture wearers was 28%.8 Another epidemiological study reported that the prevalence of DS was highest among elderly and female denture wearers.9 In addition, that study stated that the prevalence of DS ranged from 15% to over 70%.9 Sadig10 conducted a study in 2010 that reported the incidence of DS to be approximately 62%. Many factors might lead to the development of DS.11 Some of these are related to systemic and immune diseases and impaired salivary flow, and others are related to the dentures themselves, such as poor denture hygiene, denture-induced trauma, roughness and the presence of pores in the acrylic surface.11 Among these factors, Candida colonization is well established as a predisposing factor for the denture wearers experiencing development of denture stomatitis.1213 All the previously mentioned factors contribute to Candida colonization on denture and mucosal surfaces.10 Candida is not harmful by itself, and studies have demonstrated that it is part of the normal flora.11 There are 20 species of Candida among the 300 to 400 species of microorganisms in the oral cavity.14 The presence of Candida ranges from 20% to 50% in healthy dentate individuals.1516 Becoming edentulous and wearing dentures both cause changes in the oral microbial flora, which lead to an increase in Candida colonization as high as 60% to 100%.1117 Candida has the ability to grow on targeted surfaces in several ways.18 One of the ways is the formation of biofilms, which are significant causes of infection.18 The adhesion of Candida to the oral mucosa is an important factor in the resistance to host clearance mechanisms in the oral cavity. Among other Candida species, Candida albicans is the most prevalent isolated species in DS, followed by Candida glabrata.9111219 Other Candida species, such as Candida krusei, Candida Kefyr, Candida parapsilosis, and Candida tropicalis, occur at lower prevalences.91112 In addition to adhesion to the oral mucosa, the adhesion of Candida to acrylic is considered to be a critical factor in the development of DS.2021 This adhesion occurs through the formation of biofilms on the denture surface that act as protective reservoirs that prevent Candida from being washed away by saliva or dislodgment forces.19 Many studies have proven that both Candida albicans and Candida glabrata form these biofilms on denture surfaces.11222324 Several studies have linked the surface characteristics of denture acrylics to the amount of Candida biofilm adhesion.2526 Ramage et al.21 reported that imperfections on the denture surface contribute to an increase in the adhesion of Candida, which becomes imbedded within these imperfections. Other studies have also confirmed that surface roughness and surface crevices facilitate Candida colonization on denture surfaces.27 In a review, Bidra et al.28 reported that decreasing the porosity decreases Candida adhesion. Conventional heat-cured poly(methyl methacrylate) (PMMA) is the most popular material for dentures.29 It has been proven that this curing method increases the number of pores in the denture surface.29
In 1994, the first report in English to discuss the use of computer-aided technology (CAD/CAM) in the fabrication of complete denture with rapid prototyping technology was published.30 Numerous CAD/CAM denture systems appear in the market, the dentures are milled from pre-polymerized pucks of resin.3132 CAD/CAM-fabricated complete dentures have several advantages over conventionally fabricated complete dentures.28 One of these is a decrease in porosity because with CAD/CAM, the denture base is formed from a prepolymerized block of acrylic resin.28 This decrease in porosity might decrease the adhesion of Candida to the dentures.28 Also CAD/CAM fabricated dentures release a small amount of monomer, which may affect microbial adhesion and trigger a mucosal allergy reaction, but this effect is not as statistically significantly as the conventional dentures.32 Usually the internal surface of complete denture is not highly polished which may affect the roughness threshold of microbial adhesion.33 Therefore, the aim of the present study was to compare the adhesion of Candida on the surfaces of CAD/CAM and conventionally fabricated complete denture bases. The null hypothesis was that there would be no difference in Candida adhesion between the CAD/CAM and conventionally fabricated complete denture bases.
Twenty discs of Pink acrylic resin denture bases were fabricated with CAD/CAM and conventional procedures. The specimens were divided into two groups: discs that were fabricated using the CAD/CAM procedure (Wieland Digital Denture Ivoclar Vivadent, Schaan, Liechtenstein) and discs that were fabricated using a conventional flasking and pressure-pack technique.
Ten discs were fabricated from PMMA acrylic resin denture base material (major.base20 heat-processed PMMA, Moncalieri (TO), Italy) using a conventional flasking and pressure-pack technique. A stainless steel disc-shaped mold (3 × 10 mm) was used to make the discs according to the manufacturer's instructions.
The discs were cleaned with a steam jet (Wasi-Steam Classic, Wassermann Dental-Maschinen, Hamburg, Germany) after the deflasking procedure. The excess flash was removed using carbide cutters (Black Hawk Cutter, Horeco, Hopf, Ringleb & Co. GmbH & CIE, Berlin, Germany). The surface was finished with waterproof paper. Next, polishing was performed with a polishing compact unit (Derotor, London, England) consisting of a polishing lathe, a 45-mm polishing brush, and a pleated buff nettle cloth (Renfert GmbH, Industrie-gebiet, Hilzingen, Germany) with pumice (Pumice CL 60, Coarse Grade, Whip Mix Corporation, Louisville, KY, USA). Finally, the discs were cleaned with water and soap using a regular toothbrush followed by a steam jet.
Ten discs of 10 × 3 mm were designed using Zenotec CAD software (Wieland Digital Denture Ivoclar Vivadent, Schaan, Liechtenstein). PMMA blocks were used (opera system, Principauté de Monaco, French). Milling was performed using Zenotec select ion (Wieland Digital Denture Ivoclar Vivadent, Schaan, Liechtenstein). These discs were finished and polished following the same procedures used for the discs made with the conventional method.
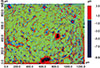
For both CAD/CAM and conventional denture materials, 30 readings were taken from randomly selected spots on the surface of each disc and subjected to surface roughness analysis. The measurements were made using a non-contact optical three-dimensional profilometer (Contour GT-I, Bruker) (Fig. 1, Fig. 2). Roughness is expressed as the surface area roughness (Sa, µm).
Candida isolates were subcultured on Sabouraud dextrose agar (SDA) (Oxoid, Hampshire, UK) for 24 hours at 37℃. The isolates were identified to the species level using the germ tube test and API20C-AUX methods. For the preparation of the yeast suspensions, the cells were inoculated in Sabouraud dextrose broth (SDB) (Oxoid, UK) and incubated for 18 hours at 37℃ with shaking at 150 rpm. The yeast cells were harvested by centrifugation at 3000 g for 10 min and washed twice with phosphate-buffered saline (PBS; pH 7.0). The cell density was adjusted to 1 × 107 cells/mL in SDB.
Biofilm formation by the Candia albicans clinical isolates was investigated with the microtiter plate method, as described previously.34 From the biofilm screening assays, four Candida albicans isolates (CA-1, CA-2, CA-3, and CA-4) were selected for the adherence assay based on their ability to form biofilms.
Biofilm-producing Candida albicans isolates were selected for the adherence assay. The discs were disinfected using 70% alcohol and washed with sterile distilled water before use in the adherence assay. For the adherence assay, yeast cells from a fresh culture were added to the SDB medium to a final concentration of 1 × 107 cells/mL. The discs of dental materials were placed in a 24-well tissue culture plate (Corning, St. Louis, MO, USA), and 1 mL of the yeast cell suspension was added. The plate was incubated for 90 min at 37℃ with shaking at 75 rpm. After incubation, the discs were transferred to new wells and washed three times with PBS to remove the non-adherent cells. The adherent Candida cells were dislodged from the surfaces of the dentures in 2 mL of PBS by scraping and vortexing for 5 minutes. The cell suspension was then gently sonicated for 3 minutes and plated on SDA. The colony-forming unit (CFU) counts were determined after 24 hours of incubation at 37℃. The determinations of the CFU counts were repeated on three different occasions separately for the four Candida albicans isolates with fresh cultures and adherence to the two different denture materials. The number of adherent cells is expressed as CFU/mL.
Candida was applied to the two types of discs (20 discs) and allowed to adhere as described above. After washing, the discs were stained with acridine orange (AO) (Sigma Aldrich, St. Louis, MO, USA) for 5 minutes, and the excess stain was gently rinsed off with PBS. The discs were examined under a fluorescent microscope (SMZ25, Nikon, Tokyo, Japan). Images were captured and analyzed using NIS-Elements imaging and analysis software (Nikon, Tokyo, Japan) (Fig. 3, Fig. 4).
Descriptive statistics were used to describe the Candida albicans isolate adhesion values for the conventional and CAD/CAM complete dentures. Student's t test was used to compare the adhesion of the Candida albicans isolates and the surface roughnesses between the CAD/CAM and conventional complete denture bases. A P value of < 0.5 was considered statistically significant.
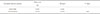
This study assessed the adherence of Candida albicans to the surface of denture bases materials manufactured in two different ways. Table 1 presents the mean Candida albicans isolate adhesion values and their standard deviations for the conventional and CAD/CAM complete dentures. The conventional complete denture surface exhibited a higher adherence of Candida albicans isolates than did the CAD/CAM surface. The percentage of reduction in the adhesion of Candida albicans (CA-1, CA-2 and CA-3) on the CAD/CAM complete dentures was significantly lower than on the conventional dentures (P < .05).
Table 2 presents the surface roughness of the complete denture surface. The conventional complete denture surface exhibited a surface roughness that was significantly greater than that of the CAD/CAM dentures.
The adherence ability was also assessed with acridin orange staining and observation under a fluorescent microscope. The number of yeast cells that adhered to the CAD/CAM discs was lower than the number that adhered to the conventional discs. This microscopic observation is in agreement with and confirms the CFU count. Four different Candida albicans isolates were used in this study to ensure that the outcome of the study was not influenced by biological differences in the Candida strains.
The null hypothesis of this study was rejected because there was a difference in Candida adhesion between the CAD/CAM and the conventionally fabricated complete denture bases. In the present study, the adhesion of Candida albicans to the CAD/CAM and conventionally fabricated complete denture base surfaces was evaluated. The CFU count, which reflects cell adherence to the denture base, was used to assess the difference in adherence. Interestingly, Candida albicans exhibited differing adherence ability to the two different denture bases. Candida albicans adhered to the CAD/CAM base with a lower affinity than it did to the conventional denture base, which had greater surface roughness than CAD/CAM base.
The mechanism by which Candida species cause denture stomatitis can be summarized as follows. Candida can form biofilms on mucosal and denture surfaces that promote plaque deposition on the denture surface.9 This deposition causes the mucosa to be continuously exposed to the microorganisms in the biofilm, which eventually causes DS.9 These biofilms are important contributors to the development of DS.35 Candida albicans is the most frequently isolated species in such biofilms.9111219 The capability of Candida albicans to adhere to and form biofilms on PMMA varies.36 The presence of a denture in the oral cavity facilitates the adherence of Candida albicans and causes infection.37
The reasons for the popularity of PMMA include its ease of handling, low cost, and esthetics.38 However, it has many disadvantages, including its dimensional instability, residual monomer content, weak strength, water absorption, color instability, and porosity. Porosity is considered to be a shortcoming when it exceeds 11% because at this point, the mechanical properties and esthetics are compromised, and the material becomes a reservoir for microorganisms.29 In 1968, the Academy of Denture Prosthetics stated that dentures should be free of pores to ensure adequate cleaning and resistance to stains and the adherence of microorganisms.38 According to the American Dental Association's specifications for the porosity of denture base polymers, “there shall be no bubbles or voids when viewed without magnification”.39 Conventional heat-cured PMMA is the most common curing technique.29 Porosity in heat-cured PMMA denture bases is an unfavorable result. Porosity can be caused by : air trapped during mixing, monomer contraction during polymerization, monomer vaporization associated with the exothermic reaction and the presence of residual monomer, insufficient mixing of monomer and polymer, a processing temperature higher than 74℃, the way the mold is packed, and inadequate compression on the flask.40414243 The surface characteristics of the denture might contribute to an increase in Candida colonization due to hydrophobicity and roughness.2526
Roughness is an important factor; the rougher the surface, the greater the Candida colonization will be.25 There are several methods and devices available to measure the surface roughness, including visual assessments, scanning electron microscopy, profilometry, laser specular reflectance, and atomic force microscopy.44 Profilometry is a common device for measuring surface roughness.45 Profilometry can be performed with either contact or non-contact methods.46 In this study, a non-contact optical three-dimensional profilometer was used. The non-contact method uses a laser or light beam to obtain a surface profile.47 Kukiattrakoon et al.47 claimed that one of the disadvantages of the contact method is that it can damage the surface by producing scratches. However, one study reported that not all irregularities in specimens can be penetrated by the sensor needle of a mechanical profilometer.48 In the present study, an optical laser profilometer that provided a three-dimensional profile was used. According to Joniot et al.,49 this method provides a non-contact, non-destructive, and rapid quantitative measurement of surface roughness.
As mentioned earlier, increased porosity has been proven to increase microorganism colonization.4850 Over the past several years, many attempts have been made to improve both the material properties and the curing and processing techniques.29 The advantage of the CAD/CAM method over the conventional method is that a prepolymerized block of acrylic resin is used to mill the denture base.28 The elimination of mixing used in the conventional procedures will decrease the porosity, which will ultimately decrease Candida adhesion. This study is considered one of the first studies that used microbiological essay comparing CAD/CAM and conventional procedure to fabricate dentures.
Alterations of denture surface characteristics, such as porosity and surface roughness, contribute to a decrease in Candida adhesion, which ultimately decreases the risk of denture stomatitis. The surface characteristics of complete dentures fabricated with the CAD/CAM procedure exhibited promising potential for reducing the adherence of Candida to the denture base surface. Moreover, the adhesion of Candida albicans to the surfaces is significantly affected by the interactions with other microorganisms in the oral cavity. Therefore, further research is needed to fully determine the difference in adhesion to the surface of these denture base materials in complex Candida and bacterial models beside in vivo studies. Also different CAD/CAM systems with different surface roughness can be tested.
Figures and Tables
Table 1
Adhesion of Candida albicans isolates (CA-1 to CA-4) to the conventional and CAD/CAM discs

Notes
References
1. Cunha-Cruz J, Hujoel PP, Nadanovsky P. Secular trends in socio-economic disparities in edentulism: USA, 1972-2001. J Dent Res. 2007; 86:131–136.
2. Emami E, de Souza RF, Kabawat M, Feine JS. The impact of edentulism on oral and general health. Int J Dent. 2013; 2013:498305.
3. Dye BA, Li X, Thorton-Evans G. Oral health disparities as determined by selected healthy people 2020 oral health objectives for the United States, 2009-2010. NCHS Data Brief. 2012; (104):1–8.
4. Douglass CW, Shih A, Ostry L. Will there be a need for complete dentures in the United States in 2020? J Prosthet Dent. 2002; 87:5–8.
5. Gotfredsen K, Walls AW. What dentition assures oral function? Clin Oral Implants Res. 2007; 18:34–45.
6. Martori E, Ayuso-Montero R, Martinez-Gomis J, Viñas M, Peraire M. Risk factors for denture-related oral mucosal lesions in a geriatric population. J Prosthet Dent. 2014; 111:273–279.
7. de Oliveira CE, Gasparoto TH, Dionísio TJ, Porto VC, Vieira NA, Santos CF, Lara VS. Candida albicans and denture stomatitis: evaluation of its presence in the lesion, prosthesis, and blood. Int J Prosthodont. 2010; 23:158–159.
8. Shulman JD, Rivera-Hidalgo F, Beach MM. Risk factors associated with denture stomatitis in the United States. J Oral Pathol Med. 2005; 34:340–346.
9. Gendreau L, Loewy ZG. Epidemiology and etiology of denture stomatitis. J Prosthodont. 2011; 20:251–260.
10. Sadig W. The denture hygiene, denture stomatitis and role of dental hygienist. Int J Dent Hyg. 2010; 8:227–231.
11. Yigit N, Aktas E, Dagistan S, Ayyildiz A. Investigating biofilm production, coagulase and hemolytic activity in Candida species isolated from denture stomatitis patients. Eurasian J Med. 2011; 43:27–32.
12. Coco BJ, Bagg J, Cross LJ, Jose A, Cross J, Ramage G. Mixed Candida albicans and Candida glabrata populations associated with the pathogenesis of denture stomatitis. Oral Microbiol Immunol. 2008; 23:377–383.
13. Ramage G, VandeWalle K, López-Ribot JL, Wickes BL. The filamentation pathway controlled by the Efg1 regulator protein is required for normal biofilm formation and development in Candida albicans. FEMS Microbiol Lett. 2002; 214:95–100.
14. Mizugai H, Isogai E, Hirose K, Chiba I. Effect of denture wearing on occurrence of Candida species in the oral cavity. J Appl Res. 2007; 7:250–254.
15. Samaranayake LP. Oral mycoses in HIV infection. Oral Surg Oral Med Oral Pathol. 1992; 73:171–180.
16. Quirynen M, Marechal M, Busscher HJ, Weerkamp AH, Darius PL, van Steenberghe D. The influence of surface free energy and surface roughness on early plaque formation. An in vivo study in man. J Clin Periodontol. 1990; 17:138–144.
17. Sumi Y, Nagaosa S, Michiwaki Y, Sunakawa M, Miura H. Comparative study of denture and pharyngeal bacterial flora of dependent elderly. Jpn J Gerodont. 2001; 16:171–178.
18. Kumamoto CA, Vinces MD. Alternative Candida albicans lifestyles: growth on surfaces. Annu Rev Microbiol. 2005; 59:113–133.
19. Ramage G, Tomsett K, Wickes BL, López-Ribot JL, Redding SW. Denture stomatitis: a role for Candida biofilms. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2004; 98:53–59.
20. Spratt DA, Pratten J. Biofilms and the oral cavity. Rev Environ Sci Biotechnol. 2003; 2:109–120.
21. Ramage G, Martínez JP, López-Ribot JL. Candida biofilms on implanted biomaterials: a clinically significant problem. FEMS Yeast Res. 2006; 6:979–986.
22. Chandra J, Mukherjee PK, Leidich SD, Faddoul FF, Hoyer LL, Douglas LJ, Ghannoum MA. Antifungal resistance of candidal biofilms formed on denture acrylic in vitro. J Dent Res. 2001; 80:903–908.
23. Kumar CP, Menon T. Biofilm production by clinical isolates of Candida species. Med Mycol. 2006; 44:99–101.
24. Ramage G, Vande Walle K, Wickes BL, López-Ribot JL. Standardized method for in vitro antifungal susceptibility testing of Candida albicans biofilms. Antimicrob Agents Chemother. 2001; 45:2475–2479.
25. Radford DR, Sweet SP, Challacombe SJ, Walter JD. Adherence of Candida albicans to denture-base materials with different surface finishes. J Dent. 1998; 26:577–583.
26. Hazen KC. Participation of yeast cell surface hydrophobicity in adherence of Candida albicans to human epithelial cells. Infect Immun. 1989; 57:1894–1900.
27. von Fraunhofer JA, Loewy ZG. Factors involved in microbial colonization of oral prostheses. Gen Dent. 2009; 57:136–143.
28. Bidra AS, Taylor TD, Agar JR. Computer-aided technology for fabricating complete dentures: systematic review of historical background, current status, and future perspectives. J Prosthet Dent. 2013; 109:361–366.
29. Singh S, Palaskar JN, Mittal S. Comparative evaluation of surface porosities in conventional heat polymerized acrylic resin cured by water bath and microwave energy with microwavable acrylic resin cured by microwave energy. Contemp Clin Dent. 2013; 4:147–151.
30. Maeda Y, Minoura M, Tsutsumi S, Okada M, Nokubi T. A CAD/CAM system for removable denture. Part I: Fabrication of complete dentures. Int J Prosthodont. 1994; 7:17–21.
31. Kattadiyil MT, Goodacre CJ, Baba NZ. CAD/CAM complete dentures: a review of two commercial fabrication systems. J Calif Dent Assoc. 2013; 41:407–416.
32. Steinmassl PA, Wiedemair V, Huck C, Klaunzer F, Steinmassl O, Grunert I, Dumfahrt H. Do CAD/CAM dentures really release less monomer than conventional dentures? Clin Oral Investig. 2017; 21:1697–1705.
33. Bollen CM, Lambrechts P, Quirynen M. Comparison of surface roughness of oral hard materials to the threshold surface roughness for bacterial plaque retention: a review of the literature. Dent Mater. 1997; 13:258–269.
34. Silva S, Henriques M, Martins A, Oliveira R, Williams D, Azeredo J. Biofilms of non-Candida albicans Candida species: quantification, structure and matrix composition. Med Mycol. 2009; 47:681–689.
35. Budtz-Jörgensen E. Etiology, pathogenesis, therapy, and prophylaxis of oral yeast infections. Acta Odontol Scand. 1990; 48:61–69.
36. Chandra J, Kuhn DM, Mukherjee PK, Hoyer LL, McCormick T, Ghannoum MA. Biofilm formation by the fungal pathogen Candida albicans: development, architecture, and drug resistance. J Bacteriol. 2001; 183:5385–5394.
37. Chaffin WL, López-Ribot JL, Casanova M, Gozalbo D, Martínez JP. Cell wall and secreted proteins of Candida albicans: identification, function, and expression. Microbiol Mol Biol Rev. 1998; 62:130–180.
38. Final report. The Academy of Denture Prosthetics. J Prosthet Dent. 1968; 20:101–105.
39. Revised American. 12 for denture base polymers. J Am Dent Assoc. 1975; 90:451–458.
40. Wolfaardt JF, Cleaton-Jones P, Fatti P. The occurrence of porosity in a heat-cured poly (methyl methacrylate) denture base resin. J Prosthet Dent. 1986; 55:393–400.
41. Keller JC, Lautenschlager EP. Porosity reduction and its associated effect on the diametral tensile strength of activated acrylic resins. J Prosthet Dent. 1985; 53:374–379.
42. al Doori D, Huggett R, Bates JF, Brooks SC. A comparison of denture base acrylic resins polymerised by microwave irradiation and by conventional water bath curing systems. Dent Mater. 1988; 4:25–32.
43. Compagnoni MA, Barbosa DB, de Souza RF, Pero AC. The effect of polymerization cycles on porosity of microwaveprocessed denture base resin. J Prosthet Dent. 2004; 91:281–285.
44. Campbell SD. Evaluation of surface roughness and polishing techniques for new ceramic materials. J Prosthet Dent. 1989; 61:563–568.
45. Jung M. Finishing and polishing of a hybrid composite and a heat-pressed glass ceramic. Oper Dent. 2002; 27:175–183.
46. Whitehead SA, Shearer AC, Watts DC, Wilson NH. Comparison of two stylus methods for measuring surface texture. Dent Mater. 1999; 15:79–86.
47. Kukiattrakoon B, Hengtrakool C, Kedjarune-Leggat U. Effect of acidic agents on surface roughness of dental ceramics. Dent Res J (Isfahan). 2011; 8:6–15.
48. Yazici AR, Müftü A, Kugel G. Three-dimensional surface profile analysis of different types of flowable restorative resins following different finishing protocols. J Contemp Dent Pract. 2007; 8:9–17.
49. Joniot SB, Grégoire GL, Auther AM, Roques YM. Threedimensional optical profilometry analysis of surface states obtained after finishing sequences for three composite resins. Oper Dent. 2000; 25:311–315.
50. Kasina SP, Ajaz T, Attili S, Surapaneni H, Cherukuri M, Srinath HP. To evaluate and compare the porosities in the acrylic mandibular denture bases processed by two different polymerization techniques, using two different brands of commercially available denture base resins - an in vitro study. J Int Oral Health. 2014; 6:72–77.




 PDF
PDF ePub
ePub Citation
Citation Print
Print






 XML Download
XML Download