Abstract
PURPOSE
This in vitro study aimed to evaluate the effect of implant connection design (external vs. internal) on the fit discrepancy and torque loss of zirconia and titanium abutments.
MATERIALS AND METHODS
Two regular platform dental implants, one with external connection (Brånemark, Nobel Biocare AB) and the other with internal connection (Noble Replace, Nobel Biocare AB), were selected. Seven titanium and seven customized zirconia abutments were used for each connection design. Measurements of geometry, marginal discrepancy, and rotational freedom were done using video measuring machine. To measure the torque loss, each abutment was torqued to 35 Ncm and then opened by means of a digital torque wrench. Data were analyzed with two-way ANOVA and t-test at α=0.05 of significance.
RESULTS
There were significant differences in the geometrical measurements and rotational freedom between abutments of two connection groups (P<.001). Also, the results showed significant differences between titanium abutments of internal and external connection implants in terms of rotational freedom (P<.001). Not only customized internal abutments but also customized external abutments did not have the exact geometry of prefabricated abutments (P<.001). However, neither connection type (P=.15) nor abutment material (P=.38) affected torque loss.
CONCLUSION
Abutments with internal connection showed less rotational freedom. However, better marginal fit was observed in externally connected abutments. Also, customized abutments with either connection could not duplicate the exact geometry of their corresponding prefabricated abutment. However, neither abutment connection nor material affected torque loss values.
Replacing teeth with dental implants is a common practice in dental treatments.1 Recently ceramic implant abutments have been used regularly in implant dentistry because of their esthetic benefits such as a better translucency and the elimination of the gray color associated with metal components that is transmitted through the peri-implant tissues.23
However, all-ceramic abutments may have mechanical limitations due to their brittleness, which makes them less resistant to tensile forces compared to metal abutments.4 Hence, the capability of all-ceramic implant restorations to tolerate the functional forces in the oral cavity remains a concern.5 To overcome such disadvantages, ceramic abutments using aluminum oxide have been developed and used in clinic. Although aluminum oxide abutments presented the advantage of optical translucency and proper fit with the implant, they may not be strong enough to withstand heavy masticatory forces.67 With high fracture strength, abrasion resistance, and biocompatibility of zirconia abutments, mechanical disadvantages of ceramic materials have been diminished.38 Consequently, zirconia abutments are the most appropriate ceramic substitute for conventional titanium abutments and are available in many different implant systems.
The implant-abutment connection design can be either internal or external.8 Several articles have compared biomechanical stability of these two implant connection designs.9101112131415 External connections have been demonstrated to orient the abutment in single tooth prostheses and benefit by working as an anti-rotational mechanism. On the other hand, there are also some biomechanical difficulties that are associated with this type of connection such as loosening or a fracture of the abutment and prostheses screws.16 A number of studies have revealed that internal implant-abutment connections are superior to external connections regarding the long-term stability of the implant-abutment complex.81718 Moreover, an internal conical connection has been demonstrated to display excessively higher in vitro strength than an external hexagonal connection because of its higher resistance to bending; In addition, the incidence of abutment screw fracture is lower with the internal connections.8171819
Fabricating methods of all-ceramic abutments are different as well. They could be either prefabricated or customized. Although prefabricated zirconia abutments are standardized and easy to use, they are often not able to afford morphologic demands of dental implant esthetics such as desired tooth dimensions and soft tissue contours.20 CAD/CAM (computer aided designed/computer aided manufactured) technology has proven its capability to fabricate prosthetic restorations in comparison with conventional techniques.2122 Accordingly, for their advantageous characteristics such as customizable design, accurate fit, and higher resistance,2324 customized ceramic abutments that are fabricated using either CAD/CAM, MAD/CAM (manually aided designed/computer aided manufactured) or MAD/MAM (manually aided designed/manually aided manufactured) systems have been suggested to be used as substitutes for prefabricated titanium and ceramic abutments in esthetic regions.2526
Beside physical properties and biocompatibility, an accurate fit of any dental restoration is vital to its long-term success.27282930 Lack of precise fit at the implant-abutment interface may lead to biological and biomechanical problems.31 Vertical and horizontal misfits apply loads to different restorative components such as implants and bones232 and could cause screw loosening, screw fracture, possible microfracture of bone, partial ischemia, crestal bone loss, and even loss of osseointegration.1 Lack of fit between components may contribute to loss of preload in the screws. Since screw-joint integrity is reliant on the preservation of preload, this change may result in screw loosening or fracture.33
Several studies have found a direct connection between rotational freedom and screw loosening at the implant-abutment interface.273435363738394041 Binon34 reported that when the rotational misfit increased from 2 degrees to 3 degrees, the average number of cycles before a screw loosening decreased from 6.7 million cycles to 4.9 million cycles (26%). Therefore, clinical complications may occur in case of higher degree rotational misfit.
Moreover, torque loss is thought to be in association with “preload” and “settling,” the variables of the joint stability. Preload is the tension generated in the screw after tightening which is necessary to keep the components together. However, settling is the flattening of micro-roughness of the metal contacting surfaces after tightening the screw and reduces the clamping force that keeps the components together.42 It is suggested that the screw loosening originates from the separation between the screw and abutment surfaces, as well as the high stress levels generated over the screws.43 Investigations evaluating the misfit effect between the external hex of the implant and the abutment screws verify a direct correlation between rotational freedom and abutment screw loosening at the abutment-implant interface.3435
A number of studies have concentrated on abutments made using CAD/CAM technique and have presented reproducible outcomes.128444546 Nonetheless this system may need computer knowledge and is not always user friendly.27 On the other hand, MAD/MAM (copy milling) system offers benefits such as a simple technique and low cost.27 Therefore, this study was determined to evaluate the precision fit, rotational freedom, and torque loss of customized zirconia and prefabricated titanium abutments in both internal and external implant systems. The null hypothesis was that there was no difference between precision fit and torque loss of titanium and customized zirconia abutments of internal and external implants.
Two regular platform dental implants were used in this investigation. One of these implants had the standard external hexagon of 0.7 mm (Brånemark, Nobel Biocare AB, Göteborg, Sweden), and the other one had an internal connection (Noble Replace, Nobel Biocare AB, Göteborg, Sweden). Two acrylic models were fabricated in which the implants were embedded perpendicular to the horizontal surface. Fourteen abutments of 3.75 mm diameter were used in each implant group, consisting of 7 customized zirconia abutments and 7 prefabricated titanium ones.
For the fabrication of zirconia abutments, two prefabricated titanium abutments of each connection were implemented as three dimensional models in the copy milling machine. Each three dimensional model was fixed in the copy milling unit (Zirkograph 025 ECO, Zirkonzahn GmbH, Gais, Italy) and milled in partially yttrium stabilized zirconia (Y2O3) green stage blocks (ICE Zirkon, Zirkonzahn GmbH) according to the directions provided by the manufacturer. All abutments were made by an expert in the respective field. Copy-milled zirconia abutments were sintered afterwards in a sintering oven (Zirkonofen 600/V2, Zirkonzahn GmbH) at 1500℃. During the sintering process the temperature rose uniformly from 20℃ to 1500℃ in approximately 3 hours and was maintained at 1500℃ for an additional 2 hours, according to the manufacturer's instructions. After the sintering process, any bulges, voids, or discrepancies were removed, and abutments were visually tested (under magnification) to assure the absence of any structural defects.
The primary part of the study involved direct measurement of the abutment connection area as well as concentricity measurement (Fig. 1). A video measuring machine (VMM) (Galileo video measuring machine, Starrett Precision Optical Limited, Jedburgh, Scotland) was employed to measure the three-dimensional lateral walls of each connection area. Data obtained from the aforementioned procedure were used to juxtapose the measures of internal and external zirconia abutments with those of titanium abutments.27
Secondarily, measurement of the marginal discrepancy of each abutment within implant was conducted. Fit accuracy was assessed by means of VMM. Embedding each group of implants in a holder, zirconia and titanium abutments were fixed to the implants by subjecting the abutment screws to a 35 Ncm torque. The vertical discrepancy was measured by placing the sample holder in the VMM in a manner that implant-abutment interface was positioned-horizontally. To determine the vertical discrepancy, the distance between two parallel lines representing the platform surface and the bottom surface of the abutment was measured. Afterwards, the horizontal misfit of each specimen was measured by placing the sample holder in the VMM in a way that the implant-abutment interface was positioned-vertically. The distance between two vertical lines traced parallel to the outer surface of the implant platform and the outer surface of the abutment designated the horizontal distance between these two surfaces and was described as the horizontal misfit. The acquired data were then analyzed by utilizing the appropriate software (QC5000, Starrett Precision Optical Limited). For each abutment, the measurements were made at four predetermined reference locations around the abutment, and the mean values were reported as horizontal and vertical misfit of each specimen.27
The third section of the investigation was meant to determine the rotational misfit between the implant and abutment. In order to achieve this objective, abutments with a flag attached to their top were located on each implant that was immobilized in a holder. Subsequently, each abutment was subjected to a counter clockwise torque and rotated until contact between the implant and abutment hexagon restricted any further rotation; VMM (Starrett Precision Optical Limited) was utilized to capture the positions. The rotational freedom was measured by calculating the angle between the flags in the two positions. All measurements were completed by a single qualified operator.27
In the final part of the study, to assess the torque loss value, implants were fixed in a holding device. Then, as instructed by the manufacturer, zirconia and titanium abutments were installed by applying 35 Ncm torque with a digital torque wrench (TQ-8800, Lutron, Taipei, Taiwan). After five minutes, the torque required to remove the abutment screw was measured. Each specimen was subjected to this procedure three times. The amount of torque lost during the specified period was reported as a percentile fraction of the applied torque. All torque loss assessments were executed by a trained operator.27 The normal distribution of the data was tested using the Kolmogorov-Smirnov test. Comparison of the values between two groups of variables (torque loss and horizontal gap) was performed using two-way ANOVA. Besides, comparison of the values between the two groups of different variable of concentricity (geometry) was tested using Independent sample t-tests. Also, given the non-normality of data on rotational freedom and vertical gap, the comparison of the study groups in terms of these variables was performed with a non-paramertic test of Mann-Whitney U test. Statistical significance was set at α = 0.05.
The concentricity, marginal discrepancies, rotational freedom, and torque loss values of zirconia and titanium abutments of both external and internal connections are presented in Table 1.
Two-way ANOVA analysis indicated that horizontal gap was significantly different between the abutments with different connections (P < .001), and the abutments with external connection showed less discrepancy. However, the abutment material did not have any significant impact on the horizontal gap (P = .14). Also, according to Mann-Whitney analysis, abutment connection and material did not have a significant effect on the vertical gap (P > .05). However, according to Mann-Whitney test, abutment connection and material significantly affected the rotational freedom (P < .001. Moreover, Two-way ANOVA analysis revealed that neither connection type (P = .15) nor abutment material (P = .38) could affect the torque loss.
There was no significant difference in the vertical gap parameter between the customized zirconia abutments with internal and external connections (P > .05). Results also showed that the customized zirconia abutments with internal and external connections had significant differences in terms of rotational freedom (P < .001). According to the t-test analysis, the customized abutments with either external or internal connection did not show the exact geometry (concentricity) of their corresponding prefabricated abutments (P < .001).
In prefabricated groups, evaluating the vertical gap showed that there was a significant difference between the internal and external abutments (P < .001). In prefabricated groups, evaluating rotational freedom showed a significant difference between internal and external abutments (P < .001), and prefabricated abutments delivered better results in both groups.
The purpose of the present study was to evaluate the effect of implant connection types on the precision of fit, rotational freedom, and torque loss of customized zirconia and prefabricated titanium abutments. According to the findings, except for the torque loss values, both precision of fit and rotational freedom parameters were affected by the implant connection in both groups of abutments. In a study by Alikhasi et al.27 precision fit, rotational freedom and torque loss parameters of customized zirconia abutments and prefabricated titanium abutments were compared. However, the effect of implant connection on the fit and rotational freedom of customized and prefabricated abutments has not been addressed in previous studies. Almost all of the related studies have investigated the effect of implant connection on the joint stability and stress distribution in this area.3435363738394041
According to Asvanund,15 implant-abutment geometry configuration could influence the interfacial stress/strain, and internal connection geometry created a lower level of stress as compared to the external one. This is probably due to the ability of this type of implant-abutment connection to distribute stresses more efficiently.17 Also, according to a review article by Gracis et al.,14 the most common complication in internal and external connections (with either zirconia or metal-based abutments) is screw loosening, which happens more frequently in externally connected ones. The reason is related to the short and narrow configuration of an external hexagon connection which limits the engagement of the external part and also creates a short fulcrum point.32
The screw joint stability of the implant-abutment connection is influenced by the rotational freedom of the abutment on the implant,3738394041 which itself is influenced by the dimensions of connection hexagon.23435 According to Binon,3940 optimal joint stability necessitates rotational freedom of less than 5 degrees. According to the finding of the present study, a mean rotational freedom of 0.970 degrees was observed in the external prefabricated titanium abutments, while the internal prefabricated ones showed no rotational misfit. According to Binon,34 rotational misfit of less than 2 degrees (as in external and internal prefabricated titanium abutments in the present study) resulted in the most stable screw joint. Similar findings for external configuration could also be found in the study of Kano and his colleagues who stated the mean rotational freedom of 1.21 ± 0.57 degrees for the machined titanium abutments.37 However, Carrilho and his colleagues reported a higher rotational freedom in the internal group compared to external configuration group.41 On the other hand, zirconia abutments with an external connection showed a mean rotational freedom of 7.911 degrees which was almost as twice as greater than the ones with internal connections (4.645 degrees). This property of zirconia abutments may lead to clinical complications such as fracture of the restoration or loosening of abutment and prosthesis screws.
Also, in a comparison between rotational fit of zirconia and titanium abutments with either external or internal connection, less fit was observed for customized abutments. Therefore, it could be concluded that not only implant connection design, but also the material and the method which has been used for the fabrication of the abutment are the important factors for this quality. However, Vigolo et al. demonstrated that if the laboratory stages are observed carefully in the fabrication of zirconia and gold-machined UCLA abutments, changes in implant-abutment interface and rotational misfit will not happen.238 In another study by Vigolo et al.,1 the rotational freedom of three types of Procera CAD/CAM abutments (titanium, zirconia and alumina) was consistently verified to be not greater than 3 degrees. Similarly, Garine et al.46 measured the rotational freedom of five ceramic abutments (two of them fabricated using CAD/CAM) and described rotational freedom of less than 5 degrees for all of them. However, the values reported for customized zirconia abutments in the present study are higher than the values in these studies.
The present study also revealed that there was a significant difference in horizontal misfit between two groups of internal and external abutment designs, regardless of their composition. Externally connected abutments showed less horizontal gap. Additionally, less marginal discrepancy was observed in the prefabricated abutments with an external connection design. The reason might be the easier accessibility to the external geometry to be read and duplicated by the scanner of milling machine. Also, missing of details during fabrication process of the customized abutments or dimensional changes of zirconia material might be responsible for their less fit as compared to the prefabricated titanium abutments. Furthermore, Abrahamsson et al.30 observed a greater microbial contamination for all-ceramic abutments due to a larger microgap as compared to the titanium abutments.
The geometric measurement of customized abutments with either connection showed less accuracy as compared to the prefabricated abutments. Butz et al.5 also stated that allceramic abutments could not be machined as accurately as metal abutments. The precision of zirconia abutments is dependent on several factors including the abutment-implant connection type, the characteristics of the raw stock zirconia, and the fabrication technique.3 The poor fit of the customized abutments in the present study could also be associated with the fabrication processes and laboratorial stages such as the scanning process, compensatory software design, milling and 20% sintering shrinkage.2122 Although designing a larger abutment could partially compensate the sintering shrinkage, the sintering procedure could cause discrepancy in the abutment hexagon dimensions and affect the precision of fit of a customized zirconia abutment. According to Park et al.,3 marginal misfit of the customized zirconia abutments were significantly higher than the prefabricated zirconia abutments. However, the vertical gap at the horizontal ledge showed no difference between the prefabricated zirconia and customized zirconia abutment groups which are in agreement with the findings of this investigation for the internal group. Also, it should be mentioned that different reports on the microgap values at the abutment-implant interface may be the result of using various implant systems with different machining tolerance and also different measuring techniques in the studies.24
In determining the torque loss values, in spite of significant differences in the fit accuracy of zirconia and titanium abutments of both connections, torque maintenance was not affected by the connection type or abutment material. This finding is in accordance with the results reported by Barbosa et al.43 While vertical misfit is thought to be a possible cause of screw loosening and torque loss, Barbosa demonstrated that there was no evidence for relating the misfit at the implant-abutment interface to torque loss.43 Additionally, according to Kano et al.42 torque loss value of all tested abutments was lower than the initial tightening torque regardless of abutment material.
Using video measuring machine with high accuracy is one of the advantages of the present study. However, a limitation of this study was that the torque loss values of customized zirconia abutments with internal or external connections were not measured and compared with prefabricated titanium abutments after cyclic loading. Also, comparing the studied qualities in other implant systems with different abutment materials could be the subject of the future investigations.
Within the limitations of this study, it could be concluded that customized zirconia abutments regardless of the connection type did not have an accurate rotational fit as prefabricated titanium abutments. Also, abutments with external connection showed superior marginal fit as compared to internal ones. Furthermore, internally connected abutments (as compared to external ones) and prefabricated abutments (as compared to customized ones) showed less rotational freedom which is an important factor in the joint stability. However, losing or maintenance of the applied torque was not related to the abutment material or connection. Also, none of the customized abutments (with internal or external connection) were an exact geometric duplicate of their prefabricated abutment models.
Figures and Tables
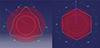 | Fig. 1Schematic depiction of geometrical (L1 - L6) and concentricity (C) measurements of both internal (left) and external (right) connection configurations. |
Table 1
The absolute mean values (± SD) of concentricity measurements, marginal discrepancy, rotational freedom, and torque loss measurements of the prefabricated and customized abutments with different connections

References
1. Vigolo P, Fonzi F, Majzoub Z, Cordioli G. An in vitro evaluation of titanium, zirconia, and alumina procera abutments with hexagonal connection. Int J Oral Maxillofac Implants. 2006; 21:575–580.
2. Vigolo P, Fonzi F, Majzoub Z, Cordioli G. An in vitro evaluation of ZiReal abutments with hexagonal connection: in original state and following abutment preparation. Int J Oral Maxillofac Implants. 2005; 20:108–114.
3. Park JI, Lee Y, Lee JH, Kim YL, Bae JM, Cho HW. Comparison of fracture resistance and fit accuracy of customized zirconia abutments with prefabricated zirconia abutments in internal hexagonal implants. Clin Implant Dent Relat Res. 2013; 15:769–778.
4. Quinn JB, Quinn GD. A practical and systematic review of Weibull statistics for reporting strengths of dental materials. Dent Mater. 2010; 26:135–147.
5. Butz F, Heydecke G, Okutan M, Strub JR. Survival rate, fracture strength and failure mode of ceramic implant abutments after chewing simulation. J Oral Rehabil. 2005; 32:838–843.
6. Andersson B, Glauser R, Maglione M, Taylor A. Ceramic implant abutments for short-span FPDs: a prospective 5-year multicenter study. Int J Prosthodont. 2003; 16:640–646.
7. Andersson B, Taylor A, Lang BR, Scheller H, Schärer P, Sorensen JA, Tarnow D. Alumina ceramic implant abutments used for single-tooth replacement: a prospective 1- to 3-year multicenter study. Int J Prosthodont. 2001; 14:432–438.
8. Leutert CR, Stawarczyk B, Truninger TC, Hämmerle CH, Sailer I. Bending moments and types of failure of zirconia and titanium abutments with internal implant-abutment connections: a laboratory study. Int J Oral Maxillofac Implants. 2012; 27:505–512.
9. Almeida EO, Freitas AC Jr, Bonfante EA, Marotta L, Silva NR, Coelho PG. Mechanical testing of implant-supported anterior crowns with different implant/abutment connections. Int J Oral Maxillofac Implants. 2013; 28:103–108.
10. Gehrke SA, Souza Dos Santos Vianna M, Dedavid BA. Influence of bone insertion level of the implant on the fracture strength of different connection designs: an in vitro study. Clin Oral Investig. 2014; 18:715–720.
11. Lin MI, Shen YW, Huang HL, Hsu JT, Fuh LJ. A retrospective study of implant-abutment connections on crestal bone level. J Dent Res. 2013; 92:202S–207S.
12. Peñarrocha-Diago MA, Flichy-Fernández AJ, Alonso-González R, Peñarrocha-Oltra D, Balaguer-Martínez J, Peñarrocha-Diago M. Influence of implant neck design and implant-abutment connection type on peri-implant health. Radiological study. Clin Oral Implants Res. 2013; 24:1192–1200.
13. Asvanund P, Morgano SM. Photoelastic stress analysis of external versus internal implant-abutment connections. J Prosthet Dent. 2011; 106:266–271.
14. Gracis S, Michalakis K, Vigolo P, Vult von Steyern P, Zwahlen M, Sailer I. Internal vs. external connections for abutments/reconstructions: a systematic review. Clin Oral Implants Res. 2012; 23:202–216.
15. Asvanund P. A strain gauge analysis comparing external and internal implant-abutment connections. Implant Dent. 2014; 23:206–211.
16. Davi LR, Golin AL, Bernardes SR, Araújo CA, Neves FD. In vitro integrity of implant external hexagon after application of surgical placement torque simulating implant locking. Braz Oral Res. 2008; 22:125–131.
17. Khraisat A, Stegaroiu R, Nomura S, Miyakawa O. Fatigue resistance of two implant/abutment joint designs. J Prosthet Dent. 2002; 88:604–610.
18. Norton MR. An in vitro evaluation of the strength of an internal conical interface compared to a butt joint interface in implant design. Clin Oral Implants Res. 1997; 8:290–298.
19. Möllersten L, Lockowandt P, Lindén LA. Comparison of strength and failure mode of seven implant systems: an in vitro test. J Prosthet Dent. 1997; 78:582–591.
20. Adatia ND, Bayne SC, Cooper LF, Thompson JY. Fracture resistance of yttria-stabilized zirconia dental implant abutments. J Prosthodont. 2009; 18:17–22.
21. Kelly JR. Developing meaningful systematic review of CAD/CAM reconstructions and fiber-reinforced composites. Clin Oral Implants Res. 2007; 18:205–217.
22. Strub JR, Rekow ED, Witkowski S. Computer-aided design and fabrication of dental restorations: current systems and future possibilities. J Am Dent Assoc. 2006; 137:1289–1296.
23. Fuster-Torres MA, Albalat-Estela S, Alcañiz-Raya M, Peñarrocha-Diago M. CAD/CAM dental systems in implant dentistry: update. Med Oral Patol Oral Cir Bucal. 2009; 14:E141–E145.
24. Beuer F, Naumann M, Gernet W, Sorensen JA. Precision of fit: zirconia three-unit fixed dental prostheses. Clin Oral Investig. 2009; 13:343–349.
25. Kapos T, Ashy LM, Gallucci GO, Weber HP, Wismeijer D. Computer-aided design and computer-assisted manufacturing in prosthetic implant dentistry. Int J Oral Maxillofac Implants. 2009; 24:Suppl. 110–117.
26. Karataşli O, Kursoğlu P, Capa N, Kazazoğlu E. Comparison of the marginal fit of different coping materials and designs produced by computer aided manufacturing systems. Dent Mater J. 2011; 30:97–102.
27. Alikhasi M, Monzavi A, Bassir SH, Naini RB, Khosronedjad N, Keshavarz S. A comparison of precision of fit, rotational freedom, and torque loss with copy-milled zirconia and prefabricated titanium abutments. Int J Oral Maxillofac Implants. 2013; 28:996–1002.
28. Lang LA, Wang RF, May KB. The influence of abutment screw tightening on screw joint configuration. J Prosthet Dent. 2002; 87:74–79.
29. Att W, Hoischen T, Gerds T, Strub JR. Marginal adaptation of all-ceramic crowns on implant abutments. Clin Implant Dent Relat Res. 2008; 10:218–225.
30. Abrahamsson I, Berglundh T, Glantz PO, Lindhe J. The mucosal attachment at different abutments. An experimental study in dogs. J Clin Periodontol. 1998; 25:721–727.
31. Baixe S, Fauxpoint G, Arntz Y, Etienne O. Microgap between zirconia abutments and titanium implants. Int J Oral Maxillofac Implants. 2010; 25:455–460.
32. Weinberg LA, Kruger B. A comparison of implant/prosthesis loading with four clinical variables. Int J Prosthodont. 1995; 8:421–433.
33. Hecker DM, Eckert SE, Choi YG. Cyclic loading of implant-supported prostheses: comparison of gaps at the prosthetic-abutment interface when cycled abutments are replaced with as-manufactured abutments. J Prosthet Dent. 2006; 95:26–32.
34. Binon PP. The effect of implant/abutment hexagonal misfit on screw joint stability. Int J Prosthodont. 1996; 9:149–160.
35. Binon PP, McHugh MJ. The effect of eliminating implant/abutment rotational misfit on screw joint stability. Int J Prosthodont. 1996; 9:511–519.
36. Jörnéus L, Jemt T, Carlsson L. Loads and designs of screw joints for single crowns supported by osseointegrated implants. Int J Oral Maxillofac Implants. 1992; 7:353–359.
37. Kano SC, Binon PP, Bonfante G, Curtis DA. The effect of casting procedures on rotational misfit in castable abutments. Int J Oral Maxillofac Implants. 2007; 22:575–579.
38. Vigolo P, Majzoub Z, Cordioli G. Measurement of the dimensions and abutment rotational freedom of gold-machined 3i UCLA-type abutments in the as-received condition, after casting with a noble metal alloy and porcelain firing. J Prosthet Dent. 2000; 84:548–553.
39. Binon PP. Evaluation of machining accuracy and consistency of selected implants, standard abutments, and laboratory analogs. Int J Prosthodont. 1995; 8:162–178.
40. Binon PP. Evaluation of three slip fit hexagonal implants. Implant Dent. 1996; 5:235–248.
41. de Barros Carrilho GP, Dias RP, Elias CN. Comparison of external and internal hex implants' rotational freedom: a pilot study. Int J Prosthodont. 2005; 18:165–166.
42. Kano SC, Binon P, Bonfante G, Curtis DA. Effect of casting procedures on screw loosening in UCLA-type abutments. J Prosthodont. 2006; 15:77–81.
43. Barbosa GA, Bernardes SR, das Neves FD, Fernandes Neto AJ, de Mattos Mda G, Ribeiro RF. Relation between implant/abutment vertical misfit and torque loss of abutment screws. Braz Dent J. 2008; 19:358–363.
44. Yüzügüllü B, Avci M. The implant-abutment interface of alumina and zirconia abutments. Clin Implant Dent Relat Res. 2008; 10:113–121.
45. Kerstein RB, Radke J. A comparison of fabrication precision and mechanical reliability of 2 zirconia implant abutments. Int J Oral Maxillofac Implants. 2008; 23:1029–1036.
46. Garine WN, Funkenbusch PD, Ercoli C, Wodenscheck J, Murphy WC. Measurement of the rotational misfit and implant-abutment gap of all-ceramic abutments. Int J Oral Maxillofac Implants. 2007; 22:928–938.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download