Abstract
PURPOSE
This study investigated the effects of silver nanoparticle (SN) loading into hydraulic calcium silicate-based Portland cement on its mechanical, antibacterial behavior and biocompatibility as a novel dental bone substitute.
MATERIALS AND METHODS
Chemically reduced colloidal SN were combined with Portland cement (PC) by the concentrations of 0 (control), 1.0, 3.0, and 5.0 wt%. The physico-mechanical properties of silver-Portland cement nanocomposites (SPNC) were investigated through X-ray diffraction (XRD), setting time, compressive strength, solubility, and silver ion elution. Antimicrobial properties of SPNC were tested by agar diffusion against Streptococcus mutans and Streptococcus sobrinus. Cytotoxic evaluation for human gingival fibroblast (HGF) was performed by MTS assay.
RESULTS
XRD certified that SN was successfully impregnated in PC. SPNC at above 3.0 wt% significantly reduced both initial and final setting times compared to control PC. No statistical differences of the compressive strength values were detected after SN loadings, and solubility rates of SPNC were below 3.0%, which are acceptable by ADA guidelines. Ag ion elutions from SPNC were confirmed with dose-dependence on the concentrations of SN added. SPNC of 5.0 wt% inhibited the growth of Streptococci, whereas no antimicrobial activity was shown in control PC. SPNC revealed no cytotoxic effects to HGF following ISO 10993 (cell viability > 70%).
CONCLUSION
Addition of SN promoted the antibacterial activity and favored the bio-mechanical properties of PC; thus, SPNC could be a candidate for the futuristic dental biomaterial. For clinical warrant, further studies including the inhibitory mechanism, in vivo and long-term researches are still required.
The demands for bone substitutes have markedly increased to compensate for bone loss or to reinforce prosthodontic dental implants. While the gold standard osseous graft is autogenous bone graft with its excellent osteoconduction/induction, limitations including financial cost, extra surgical time, and additional donor site morbidity have motivated efforts to find alternatives.12 Inorganic bone cements have been used biomedically to compensate for bone defects or as the substitutes that do not migrate from the recipient as can occur in the granule type. Portland cement (PC) is an inorganic, hydraulic, calcium silicate-based material. PC is characterized by stable biocompatibility, high compressive strength, rapid set-up, and low solubility to blood. This allows PC to be useful in providing initial graft stability in medical orthopedic applications.34 Concerning dental applications, PC is a main component of mineral trioxide aggregate (MTA), which is already widely used in endodontic surgery including root end filling, root repair, and pulp capping due to its biological and physicochemical properties.56 PC stimulates mineralized tissue formation.7 It can also be economically appropriate for use in dental bone cement for small osseous defects.8 A pig model revealed that new bone formation occurred adjacent to bony sockets containing PC.9 Other results from a rabbit model suggested that PC can provide early implant stability and good mechanical properties while maintaining intimate bone-implant interfaces without soft tissue intervention.10 Despite these biological merits, PC-based materials have limited or controversial antimicrobial effects against some microorganisms.1112 Bacterial infection could remain a significant complication following chemo-mechanical instrumentation in the graft procedure and could lead to the development of antibiotic-resistant microorganisms. Antimicrobial bone cement would be a welcomed way of reducing the incidence of infection while maintaining the performance benefits. The incorporation of antimicrobial agents into bone cement is a practical approach because PC is a powder/liquid system and antibacterial elements could easily be combined in the powder or liquid during the mixing procedure.
Silver nanoparticles (SN) are widely-used nano-additives for preventing bacterial colonization of surfaces on catheters, 13 dental materials,1415 and PMMA (polymethylmetacrylate) bone cement.16 It is widely accepted that the main antibacterial effect of SN-based materials is due to the release of silver ion (Ag+) via interaction with a medium.17 The ion interacts with disulfide or sulfhydryl groups of enzymes, disrupting metabolic processes followed by cell death18 or free radicals derived from their surface that lead the cell membrane damage.19 Furthermore, nano-engineered PC with nanoparticles showed the reinforced concrete material behavior as well as accelerated wound healing.2021 Various dental polymers infiltrated by SN have been investigated for their antimicrobial activity and characterized.1415 However, until now, the antimicrobial efficacy of SN in calcium silicate cement has not been addressed. SN could act as heterogeneous nuclei or impurities, which could influence the cement hydration process and jeopardize PC matrix because of their high reactivity as well as toxicity. The aim of this study was to assess the effect of SN on biomechanical properties and antibacterial activity of PC to develop a novel hydraulic bone cement.
The materials for fabrication of silver-Portland cement nanocomposites (SPNC) samples are shown in Table 1. Calcium sulfate (type VI stone, Die-Keen, Heraeus Kulzer Inc., South Bend, IN, USA) and hydroxyethyl cellulose (HEC, Sigma-Aldrich, St. Louis, MO, USA) were added to control the setting time and workability of PC (type I, Hanil Cement Co., Seoul, Korea). Collectively, PC and calcium sulfate were powder components. Pure PC powders were passed through a sieve (250-mesh) and homogenized in a ball mill for 5 min to minimize the presence of agglomerates. Calcium sulfate was homogenously blended into pure PC by 9.0 weight percent (wt%) through the mortar and pestle method. SN and HEC were separately added to powder components as the colloidal components. Colloidal SN was prepared by reduction of silver nitrate (AgNO3, Aldrich, St. Louis, MO, USA) with sodium borohydride (NaBH4, Aldrich, St. Louis, MO, USA). This process can be described by the reaction, AgNO3 + NaBH4 → Ag + ½ H2 +½ B2H6 +NaNO3, and 2.0% PVP (polyvinyl pyrrolidon) was used as a stabilizer. Transmission electron microscopy (TEM) revealed the morphology of prepared SN, with particle size ranging from 50 to 80 nm (Fig. 1). HEC granules were dispersed homogeneously in warm water to produce a 1.5% HEC solution. The incorporating dose of SN to PC was 0 (control), 1.0, 3.0, and 5.0 wt%. Each colloidal SN and HEC solution was simultaneously added to the powder components at a liquid/powder ratio of 0.3 mL/g, and the solutions were then vacuum mixed for 15 seconds to produce cement slurries. Each mixture was packed into custom molds to produce a uniform shape that met each experimental protocol. The samples were kept in 100% relative humidity at 37℃ until used. Crystalline phase analysis for SPNC was carried out using X-ray diffraction (XRD) in an automated XRD-7000 powder diffractometer (Shimadzu, Kyoto, Japan). The physico-mechanical properties of SPNC were tested through setting time, compressive strength, solubility, and Ag+ elution. Setting times were measured by a 400 g Gillmore needle with a 1 mm diameter, in accordance with international standard ISO 9917-1 for water-based cements.22 Mixed slurries were poured into a disc mold (10 mm × 3 mm). A sample (n = 10) was considered to be initially set when light needle (190 g in weight) could not mark its surface with a complete circular indentation on the sample surface for the first time. The final setting time was then recorded when the needle failed to penetrate the specimen with a heavy needle (455 g in weight).
For compressive strength, mixed slurries were placed into a silicone mold producing cylindrical (10 mm × 5 mm) samples (n = 10) and were incubated at 37℃ with 100% humidity. Compressive strength was measured using a model GB/4302 universal testing machine (Instron Corp., Canton, MA, USA) at a crosshead speed of 1 mm/min at 24 h and 168 h, respectively. Values were calculated using the equation C = 4P/πD2, where P is the applied load and D is the diameter of the tested specimen. For solubility test, disc samples (10 mm × 3.0 mm, n = 10) were prepared and stored for 24 h at 100% relative humidity. In the next stage, each sample was separately placed in glass bottles containing 100 mL of distilled water (DW) at 37℃ for 1 h. The drying and weighing steps of the samples were conducted at 24 and 168 h intervals. The percentage of solubility was calculated using the following formula: (weight loss × 100)/initial weight and a weight loss in 0.1 mg was interpreted as solubility. The solubility below 3.0% was determined acceptable based on ISO 6876 and ADA protocol.23 Ag+ detection was done using a model 240FS AA atomic absorption spectrophotometer (Agilent Technologies, Santa Clara, CA, USA) and model SI-600R shaking incubator (JEIO TECH, Seoul, Korea). After the final set, each disc specimen (10 mm × 3.0 mm, n = 10) was put into 100 mL of sterile DW and then stored at 37℃ under agitation. The concentration of eluted Ag+ was measured at 24 and 168 h, with daily replacement of distilled water. The quantity (in mg/L) of ion was expressed as the amounts of ion in the solution per unit of surface area of the disc (in cm2).
Antibacterial activity of SPNC was evaluated by an agar diffusion test (ADT) against two oral bacteria, Streptococcus mutans (S. mutans, ATCC 25175) and Streptococcus sobrinus, (S. sobrinus, ATCC 27607). Bacteria were suspended in brain heart infusion (BHI) broth and turbidity was adjusted to 0.5 McFarland standard, corresponding to approximately 1.0 × 107 colony forming units (CFU)/mL after serial dilution. Cement discs (10 mm × 3.0 mm, n = 9) were sterilized with ethylene oxide gas for 24 h prior to experiment. Each bacterial suspension was streaked evenly in two planes onto the surface of the medium with a cotton swab. After the inoculum had been dried, the disc specimens were placed onto an agar plate and incubated overnight at 37℃ in an aerobic environment. Diameters of inhibition halo produced around disc were optically measured by a sliding caliper with 0.1 mm accuracy at three different points. Sizes of the inhibition halo were calculated by subtracting the diameter of the specimen (10 mm) from the average of the three measurements of the halo. For biocompatibility test, a disc sample (10 mm × 3.0 mm, n = 5) was sterilized and immersed in phosphate buffered saline (PBS) overnight at 37℃. Human gingival fibroblasts (HGF, ATCC 2014) were cultured at a concentration of 4 × 104 cells/mL and dispensed in 24-well plates. The extracts from cement samples (20 µL) were added to the respective well and incubated for 24 h. After collection of cell supernatants, 10% MTS (2,5-diphenyltetrazolium bromide) solution (Sigma-Aldrich, St. Louis, MO, USA) was added to each well and kept in a dark environment for 4 h at 37°C. 100 µL of Dimethyl sulfoxide (DMSO) was added to each well followed by aspiration of MTS. Optical density for each group was measured using an ELISA reader at 570 nm. The relative cell viability (%) related to control wells containing cell culture medium without sample was calculated. The reduction of cell viability by more than 30% are regarded as cytotoxic according to ISO 10993-5.24
The results were evaluated by one-way ANOVA, followed by Student's t-test for post-Hoc test. A significance level of 0.05 was used for statistical tests.
The XRD analysis of powder particles from SPNC confirmed that SN was successfully embedded in PC (Fig. 2). The characteristic peak assigned with pure Ag (2θ = 38°) was not identified by the detection limit of the diffractometer used in this study. The spikes ranged from 33° to 36°, indicating the isomorphous clusters of silver-oxygen-silicate (Ag6-O7-Si2), which implied the presence of silver in PC (Fig. 2). The results of mechanical tests are shown in Table 2.
After mixing with water, setting times of 1.0 wt% SPNC were not significantly different to those of the PC-control (P > .05). However, SPNC above 3.0 wt% decreased significantly in both the initial and final setting times as compared with the PC-control with dose dependent manner (P < .05).
All samples possessed significantly higher compressive strength values after 168 h than after 24 h (P < .05). However, the addition SN to PC did not significantly improved the compressive strength compared to PC-control at both periods (P > .05).
The percentages of weight loss were significantly increased at 168 h than 24 h (P < .05) and SPNC above 3.0 wt% revealed significant loss of weight at both intervals as compared to PC-control (P < .05) and 1.0 wt% SPNC. The highest weight loss was seen in 5.0 wt% SPNC with value of 2.81 ± 0.07% at 168 h and there was no significant weight loss between 3.0 wt% and 5.0 wt% SPNC (P > .05).
Ag+ release was detected from all SPNCs, except the control. Eluted quantities were dose-dependent on SN incorporated amounts and SNPC 1.0 wt% released a small, negligible amount of Ag, which was statistically equivalent to that of control. There was no significant difference for eluted amount between two intervals (P > .05).
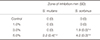
The bacterial inhibitory actions of SPNC on S. mutans and S. sorbinus after 24 h incubation are presented in Table 3 and Fig. 3. Control and 1.0 wt% SPNC did not show a clear antibiotic effect against two bacteria. 3.0 wt% SPNC inhibited S. sorbinus by 1.9 ± 0.5 mm, while no inhibition halos were shown for S. mutans at the same dose. SNPC of 5.0 wt% significant inhibited S. sorbinus (halo diameter 4.2 ± 0.3 mm) and S. mutans (halo diameter 2.2 ± 0.4 mm). S. sorbinus showed the statistically higher sensitivity to SPNC than S. mutans (P < .05). Control and 1.0 wt% group revealed statistically similar values as negative control (medium-only). 3.0 and 5.0 wt% SPNC showed statistically lower cell viability from negative control by 83.5% and 79.6%, respectively, without a significant difference between two groups (Fig. 4).
A lot of commercialized bone substitutes contain typical carriers that are easily manipulated in clinics; these include hyaluronic acid, glycerol, calcium sulfate, and gelatin.25 In this study, calcium sulfate and HEC were added to SPNC for setting time control as well as moldability.10 The setting time of pure PC is 3 - 4 h at a typical liquid/powder ratio of 0.3 mL/g.26 A long setting time may be a clinical handicap due to the lack of cement stability during initial healing. Calcium sulfate presently acted as an accelerant to the PC to decrease curing time to around 1 h. HEC can provide cohesion to SPNC, producing a more thixotropic material to resist washout from liquid flow, such as bleeding.2728 All of the samples at 168 h showed higher compressive strength values than at 24 h. SN incorporation did not interfere the hydration phase of PC, which provides more hardness to the cement material after final setting. It was anticipated that SN within PC matrix could reinforce the material similar to fillers in resin composites.29 Wang et al.30 reported PC added by carbon fiber was improved in the compressive strength because carbon fibers blocked the initiation and propagation of microcracks. Machado et al.29 reported that PC infiltrated by amalgam particles enhances the compressive strength as well as setting time. Guerreiro-Tanomaru et al.21 adversely reported that the combination of PC with nanozinc oxide significantly decreased the compressive strength due to flaws or porosity in its microstructure. In the present test, the compressive strength of PC was not improved regardless of increasing SN dose. The absence of a stable chemical union between PC matrix and nanoparticles might have limited the increase in strength.
Results of SPNC setting times revealed that an increase in the weight fraction of SN at above 3.0 wt% caused a significant decrease in both the initial and final setting times of PC. It is assumed that SN incorporation accelerated the hydration reaction of cement than control PC. Nanoparticles are characterized by extremely small particle size, high surface energy, and unique surface effects.31 These characteristics hastened the hydration of silicates, which resulted in a faster reaction speed. The maximum solubility rate was 2.81% in SPNC 5.0 wt% at 168 h, which was acceptable in vitro. However, in vivo the solubility rates of SPNC might be higher under clinical conditions. Bone cement inevitably interacts with surrounding vital environment when in contact with biologic tissues and fluids. The solubility test in the present study was conducted in DW only followed by final set under testing standard protocol; this does not reflect the clinical situation because bone cement immediately contacts fluid, such as blood.32
The antimicrobial activity of SPNC was assessed in vitro by ADT. Despite some limitations, this test can provide a direct comparison and a reproducible result of antimicrobial effects against the tested strains if variables are properly controlled.33 ADT relies on the material's diffusibility across the medium as well as antimicrobial material itself, and a material that easily diffuses could probably generate the larger inhibition halo. The solubility of nanocomposites might also influence the metal ion availability for inhibitory action at the medium interface and low solubility of SPNC after the hydration reaction might affect the antimicrobial activity. Hotta et al.34 reported that higher silver amounts were not needed to produce an antibacterial effect, given the dose-dependent release of silver from matrix. On the contrary, Yoshida et al.35 suggested the inhibitory effect of composite resin with SN could be due to direct contact with S. mutans regardless of silver ion release. Unlike the inorganic cement, ion releasing from solid PMMA is more handicapped owing to hydrophobic polymer network whose water uptake may be insufficient to release ions.3637 Some studies revealed that PC (MTA) may not produce adequate free radicals and PC has the limited antimicrobial effect to some microorganisms.3839 The present finding similarly suggests that control PC had no antibacterial effect, similar to previous reports.5111239 SNPC of 5.0 wt% exhibited significant inhibitory effects to both tested bacteria, which could be attributed to the elution of Ag+ out of SPNC into the media, as shown by other studies of nanosilver-MTA composites. 2340 Furthermore, prolonged and persistent antimicrobial effect would be expected because silver-oxygen-silicate clusters detected by XRD might play a role in a reservoir of Ag+ to elute. S. mutans and S. sobrinus were selected as the representative oral bacteria that primarily cause dental caries. S. sorbinus was more sensitive to lower Ag+ concentration from SPNC, which can be explained by the different thickness and complexity of bacterial cell walls.40 Nevertheless, regarding the limitations of ADT, further studies are required to clarify the antimicrobial mechanism of SPNC including physicochemical factors such as electrostatic charge, hydrophobicity, or surface free energy.
In this study, the maximum SN incorporating dose to PC was controlled under 5.0 wt% to consider possible silver toxicity as well as to secure mechanical aspects of SPNC. According to Zand et al.,41 addition of 1.0 wt% of SN to MTA did not alter its biocompatibility in an animal study. Gomes-Filho et al.42 concluded that dispersion of embedded SN from fibrin sponge was non-toxic response to tissue, especially under low concentration. All of the tested SPNC revealed no cytotoxic effect to HGF at 24 h incubation according to the ISO standard24 (cell viability by more than 70%), although the inherent toxicity of SN must be considered. Silver could produce free radicals, which might explain a potential toxicity to oral tissue and an antibacterial activity simultaneously.43 For practical applications of SPNC, controlled silver release and long-term exposure to SN compounds are also needed for biocompatible dental bone cement due to its sustained antimicrobial activity.
Within the limitation of this preliminary study, the addition of silver nanoparticles to PC can be a possible antimicrobial dental bone substitute with acceptable mechanical strength, degradability, and biocompatibility. Further investigations for SPNC are needed, including in vivo and long-term data, and the clarification of the inhibitory mechanism to be used clinically.
Figures and Tables
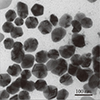 | Fig. 1TEM of the prepared silver nanoparticle used in this study. The particle diameters ranged from 50 to 80 nm. |
 | Fig. 2XRD pattern of SPNC. Asterisk (*) peaks denote silver-doped precipitates formed as silver-oxygen-silicate (Ag6-O7-Si2) clusters indicating the presence of silver. (a) calcium sulfate (CaSO4), (b) Ettringite (calcium aluminium sulfate mineral), (c) tricalcium silicate + CaCO3 isomorphous AgO. |
 | Fig. 3Representative photos of disc diffusion test. (A) control (0 w%), (B) 5.0 w% SPNC against S. mutans, (C) 5.0 w% SPNC against S. sorbinus. |
 | Fig. 4Cytotoxic effects of SPNC extracts on HGF at 24 hour-incubation. 100% cell viability was considered for the control negative (medium-only group). Statistically significant differences are indicated by (*) when P < .05. |
Table 1
Composition of SPNC

Table 2
Mean values and standard deviation (SD) of physico-mechanical tests

References
1. Berberi A, Samarani A, Nader N, Noujeim Z, Dagher M, Kanj W, Mearawi R, Salemeh Z, Badran B. Physicochemical characteristics of bone substitutes used in oral surgery in comparison to autogenous bone. Biomed Res Int. 2014; 2014:320790.
2. Kim YK, Yun PY, Um IW, Lee HJ, Yi YJ, Bae JH, Lee J. Alveolar ridge preservation of an extraction socket using autogenous tooth bone graft material for implant site development: prospective case series. J Adv Prosthodont. 2014; 6:521–527.
3. Wynn-Jones G, Shelton RM, Hofmann MP. Development of Portland cement for orthopedic applications, establishing injectability and decreasing setting times. J Biomed Mater Res B Appl Biomater. 2012; 100:2213–2221.
4. Peh WC, Munk PL, Rashid F, Gilula LA. Percutaneous vertebral augmentation: vertebroplasty, kyphoplasty and skyphoplasty. Radiol Clin North Am. 2008; 46:611–635.
5. Torabinejad M, Watson TF, Pitt Ford TR. Sealing ability of a mineral trioxide aggregate when used as a root end filling material. J Endod. 1993; 19:591–595.
6. Camilleri J, Montesin FE, Di Silvio L, Pitt Ford TR. The chemical constitution and biocompatibility of accelerated Portland cement for endodontic use. Int Endod J. 2005; 38:834–842.
7. Saidon J, He J, Zhu Q, Safavi K, Spångberg LS. Cell and tissue reactions to mineral trioxide aggregate and Portland cement. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2003; 95:483–489.
8. Abdullah D, Ford TR, Papaioannou S, Nicholson J, McDonald F. An evaluation of accelerated Portland cement as a restorative material. Biomaterials. 2002; 23:4001–4010.
9. Dokami S, Raoofi S, Ashraf MJ, Khorshidi H. Histological analysis of the effect of accelerated portland cement as a bone graft substitute on experimentally-created three-walled intrabony defects in dogs. J Dent Res Dent Clin Dent Prospects. 2007; 1:131–135.
10. Seong WJ, Kim HC, Jeong S, DeVeau DL, Aparicio C, Li Y, Hodges JS. Ex vivo mechanical properties of dental implant bone cement used to rescue initially unstable dental implants: a rabbit study. Int J Oral Maxillofac Implants. 2011; 26:826–836.
11. Estrela C, Bammann LL, Estrela CR, Silva RS, Pécora JD. Antimicrobial and chemical study of MTA, Portland cement, calcium hydroxide paste, Sealapex and Dycal. Braz Dent J. 2000; 11:3–9.
12. Miyagak DC, de Carvalho EM, Robazza CR, Chavasco JK, Levorato GL. In vitro evaluation of the antimicrobial activity of endodontic sealers. Braz Oral Res. 2006; 20:303–306.
13. Samuel U, Guggenbichler JP. Prevention of catheter-related infections: the potential of a new nano-silver impregnated catheter. Int J Antimicrob Agents. 2004; 23:S75–S78.
14. Nam KY. In vitro antimicrobial effect of the tissue conditioner containing silver nanoparticles. J Adv Prosthodont. 2011; 3:20–24.
15. Jonaidi-Jafari N, Izadi M, Javidi P. The effects of silver nanoparticles on antimicrobial activity of ProRoot mineral trioxide aggregate (MTA) and calcium enriched mixture (CEM). J Clin Exp Dent. 2016; 8:e22–e26.
16. Alt V, Bechert T, Steinrücke P, Wagener M, Seidel P, Dingeldein E, Domann E, Schnettler R. An in vitro assessment of the antibacterial properties and cytotoxicity of nanoparticulate silver bone cement. Biomaterials. 2004; 25:4383–4391.
17. Kumar R, Howdle S, Münstedt H. Polyamide/silver antimicrobials: effect of filler types on the silver ion release. J Biomed Mater Res B Appl Biomater. 2005; 75:311–319.
18. Feng QL, Wu J, Chen GQ, Cui FZ, Kim TN, Kim JO. A mechanistic study of the antibacterial effect of silver ions on Escherichia coli and Staphylococcus aureus. J Biomed Mater Res. 2000; 52:662–668.
19. Durán N, Durán M, de Jesus MB, Seabra AB, Fávaro WJ, Nakazato G. Silver nanoparticles: A new view on mechanistic aspects on antimicrobial activity. Nanomedicine. 2016; 12:789–799.
20. Jafari H, Afshar S. Improved photodegradation of organic contaminants using Nano-TiO2 and TiO2-SiO2 deposited on portland cement concrete blocks. Photochem Photobiol. 2016; 92:87–101.
21. Guerreiro-Tanomaru JM, Trindade-Junior A, Costa BC, da Silva GF, Drullis Cifali L, Basso Bernardi MI, Tanomaru-Filho M. Effect of zirconium oxide and zinc oxide nanoparticles on physicochemical properties and antibiofilm activity of a calcium silicate-based material. ScientificWorldJournal. 2014; 2014:975213.
22. International Organization for Standardization. ISO 9917-1, Dentistry-water-based cements part 1: powder/liquid acid-base cements. Geneva, Switzerland: International Standard Organization;2003.
23. Samiei M, Shahi S, Aslaminabadi N, Valizadeh H, Aghazadeh Z, Pakdel SM. A new simulated plasma for assessing the solubility of mineral trioxide aggregate. Iran Endod J. 2015; 10:30–34.
24. International Organization for Standardization. ISO 10993-5. In: Biological evaluation of medical devices-Part 5: Tests for in vitro cytotoxicity. Geneva, Switzerland: International Standard Organization;2009.
25. Kim YK, Lee JY, Kim SG, Lim SC. Guided bone regeneration using demineralized allogenic bone matrix with calcium sulfate: case series. J Adv Prosthodont. 2013; 5:167–171.
26. Ber BS, Hatton JF, Stewart GP. Chemical modification of proroot mta to improve handling characteristics and decrease setting time. J Endod. 2007; 33:1231–1234.
27. Alves HL, Dos Santos LA, Bergmann CP. Injectability evaluation of tricalcium phosphate bone cement. J Mater Sci Mater Med. 2008; 19:2241–2246.
28. Wang X, Chen L, Xiang H, Ye J. Influence of anti-washout agents on the rheological properties and injectability of a calcium phosphate cement. J Biomed Mater Res B Appl Biomater. 2007; 81:410–418.
29. Machado DF, Bertassoni LE, Souza EM, Almeida JB, Rached RN. Effect of additives on the compressive strength and setting time of a Portland cement. Braz Oral Res. 2010; 24:158–164.
30. Wang C, Li KZ, Li HJ, Jiao GS, Lua J, Houa DS. Effect of carbon fiber dispersion on the mechanical properties of carbon fiber-reinforced cement-based composites. Mater Sci Eng. 2008; 487:52–57.
31. Ye Q. The study and development of the nano-composite cement structure materials. New Build Mater. 2001; 1:4–6.
32. Bortoluzzi EA, Broon NJ, Bramante CM, Felippe WT, Tanomaru Filho M, Esberard RM. The influence of calcium chloride on the setting time, solubility, disintegration, and pH of mineral trioxide aggregate and white Portland cement with a radiopacifier. J Endod. 2009; 35:550–554.
33. Tobias RS. Antibacterial properties of dental restorative materials: a review. Int Endod J. 1988; 21:155–160.
34. Hotta M, Nakajima H, Yamamoto K, Aono M. Antibacterial temporary filling materials: the effect of adding various ratios of Ag-Zn-Zeolite. J Oral Rehabil. 1998; 25:485–489.
35. Yoshida K, Tanagawa M, Atsuta M. Characterization and inhibitory effect of antibacterial dental resin composites incorporating silver-supported materials. J Biomed Mater Res. 1999; 47:516–522.
36. Imazato S, Ebi N, Takahashi Y, Kaneko T, Ebisu S, Russell RR. Antibacterial activity of bactericide-immobilized filler for resin-based restoratives. Biomaterials. 2003; 24:3605–3609.
37. Monteiro DR, Gorup LF, Takamiya AS, de Camargo ER, Filho AC, Barbosa DB. Silver distribution and release from an antimicrobial denture base resin containing silver colloidal nanoparticles. J Prosthodont. 2012; 21:7–15.
38. Ribeiro CS, Scelza MF, Hirata Júnior R, Buarque de. The antimicrobial activity of gray-colored mineral trioxide aggregate (GMTA) and white-colored MTA (WMTA) under aerobic and anaerobic conditions. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2010; 109:e109–e112.
39. Estrela C, Bammann LL, Estrela CR, Silva RS, Pécora JD. Antimicrobial and chemical study of MTA, Portland cement, calcium hydroxide paste, Sealapex and Dycal. Braz Dent J. 2000; 11:3–9.
40. Bahador A, Pourakbari B, Bolhari B, Hashemi FB. In vitro evaluation of the antimicrobial activity of nanosilver-mineral trioxide aggregate against frequent anaerobic oral pathogens by a membrane-enclosed immersion test. Biomed J. 2015; 38:77–83.
41. Zand V, Lotfi M, Aghbali A, Mesgariabbasi M, Janani M, Mokhtari H, Tehranchi P, Pakdel SM. Tissue reaction and biocompatibility of implanted mineral trioxide aggregate with silver nanoparticles in a rat model. Iran Endod J. 2016; 11:13–16.
42. Gomes-Filho JE, Silva FO, Watanabe S, Cintra LT, Tendoro KV, Dalto LG, Pacanaro SV, Lodi CS, de Melo FF. Tissue reaction to silver nanoparticles dispersion as an alternative irrigating solution. J Endod. 2010; 36:1698–1702.
43. Chaloupka K, Malam Y, Seifalian AM. Nanosilver as a new generation of nanoproduct in biomedical applications. Trends Biotechnol. 2010; 28:580–588.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download