Abstract
PURPOSE
The purpose of this study was to evaluate the influence of different coping thicknesses and veneer ceramic cooling rates on the failure load of zirconia-ceramic crowns.
MATERIALS AND METHODS
Zirconia copings of two different thicknesses (0.5 mm or 1.5 mm; n=20 each) were fabricated from scanning 40 identical abutment models using a dental computer-aided design and computer-aided manufacturing system. Zirconia-ceramic crowns were completed by veneering feldspathic ceramics under different cooling rates (conventional or slow, n=20 each), resulting in 4 different groups (CONV05, SLOW05, CONV15, SLOW15; n=10 per group). Each crown was cemented on the abutment. 300,000 cycles of a 50-N load and thermocycling were applied on the crown, and then, a monotonic load was applied on each crown until failure. The mean failure loads were evaluated with two-way analysis of variance (P=.05).
RESULTS
No cohesive or adhesive failure was observed after fatigue loading with thermocycling. Among the 4 groups, SLOW15 group (slow cooling and 1.5 mm chipping thickness) resulted in a significantly greater mean failure load than the other groups (P<.001). Coping fractures were only observed in SLOW15 group.
CONCLUSION
The failure load of zirconia-ceramic crowns was significantly influenced by cooling rate as well as coping thickness. Under conventional cooling conditions, the mean failure load was not influenced by the coping thickness; however, under slow cooling conditions, the mean failure load was significantly influenced by the coping thickness.
Due to its high strength, zirconia has been successfully used as a framework material for long span posterior fixed dental prostheses as well as anterior single tooth restorations. Previous studies reported no fractures in the zirconia framework within 3 - 4 years of clinical service.123 In addition to its excellent strength, zirconia, compared to titanium, shows a favorable peri-implant soft tissue color match.4 Therefore, dental zirconia is also preferred as an abutment material for anterior implant restorations.
Despite these advantages, zirconia-ceramic crowns have a major drawback. Clinical studies show that the chipping rate of the veneering ceramic is much higher in zirconia-ceramics than in metal-ceramics.567 Monolithic zirconia restorations, which are fabricated from more translucent zirconia blocks, have been clinically used recently to overcome chipping problems.8,9 Monolithic zirconia can be characterized by special coloring liquids before the sintering process to get esthetic results. However, there are limitations in obtaining excellent anterior esthetics with the coloring technique, and therefore, layering ceramics on a zirconia framework remains a preferred method to fabricate esthetic anterior restorations.
Experimental studies have suggested the following causes for higher chipping rate: (1) damage to the ceramic surface after occlusal adjustments10; (2) mismatched coefficient of thermal expansion between the veneer ceramic and the zirconia coping11; (3) relationship between the coping thickness and the coefficient of thermal expansion12; (4) inadequate zirconia framework design13,14; and (5) poor adhesion between the ceramic and the zirconia coping.15,16
Accumulated residual stresses during the cooling process of the veneering ceramics have recently been focused as a major cause of veneer chipping.17181920 In contrast to metal-ceramics, slow cooling is recommended for zirconia-ceramics because fast cooling after the final firing introduces greater residual tensile stress in the veneering ceramic layer,21,22 and increased residual tensile stress is vulnerable to crack propagation. A previous research showed that the amount and type of residual stresses (i.e., compressive or tensile stress) were also influenced by the thickness of the zirconia coping.23,24 Therefore, the cooling rate and the zirconia coping thickness should be considered in order to minimize chipping. To date, little information is available concerning the interaction between the cooling ratio and the zirconia coping thickness on the failure load of zirconia-ceramic restorations.
The purpose of the current study was to evaluate the impact of different zirconia coping thicknesses and cooling rates on the failure loads of zirconia-ceramic crowns in the fatigue test. The null hypothesis tested was that neither the zirconia coping thickness nor the cooling rate influences the failure load of zirconia-ceramic crowns.
A simplified configuration of an abutment was designed (Fig. 1). Forty abutments were fabricated from polymethylmethacrylate (Arystal 100, Plavex Ltd., Geumwang, Korea) using a dental computer-aided design and computer-aided manufacturing (CAD/CAM) system (Chameleon, Neobiotech, Seoul, Korea).
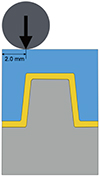
The abutment models were randomly divided into two groups (N = 20 teeth per group). Each abutment was digitally scanned using a dental desktop scanner (D700, 3Shape, Copenhagen, Denmark). Using CAD software (Model Builder, 3Shape), two different coping configurations were designed: 0.5-mm thick zirconia coping and 1.5-mm-thick zirconia coping (Fig. 2). A total of forty zirconia copings were milled from presintered zirconia blocks (NaturZ, D-max, Seoul, Korea) using a 5-axis milling machine (Zmatch, DentAim, Seoul, Korea). They were then sintered at 1450℃ for 7 hours in a special furnace (Zmatch sintering furnace, DentAim). The zirconia coping was randomly chosen and veneered with feldspathic ceramic (e.max Ceram, A2 shade; Ivoclar Vivadent, Schaan, Liechtenstein), and then sintered to form a simple shape of zirconia-ceramic crown. A mold was fabricated by indexing the restoration with a heavy viscosity silicone impression material (Aquasil Heavy Putty, Dentsply International, York, PA, USA), for the veneering ceramic build up. The remaining 39 zirconia ceramic crowns were fabricated using the mold. To check the dimension of the veneering porcelain, the final dimension of each crown was measured using a digital caliper (Series 500, Mitutoyo America Corporation, Plymouth, MI, USA).
Two different firing cycles were used. For the conventionally cooling cycle, the zirconia-ceramic crowns were tempered from 900℃ to room temperature by opening the furnace door. The crowns were then removed from the honeycomb tray as soon as the muffle of the furnace had completely descended. For the slow cooling cycle, the furnace temperature was cooled from 900℃ to 500℃ at a cooling rate of 2℃ per minute. The furnace door was then opened. Each group was divided into two subgroups, based on the cooling rate (i.e., the slow cooling and conventional cooling groups; N = 10 crowns per subgroup) Therefore, the resulting subgroups were: 1) CONV05, conventional cooling and 0.5 mm coping thickness; 2) SLOW05, slow cooling and 0.5 mm coping thickness; 3) CONV15, conventional cooling and 1.5 mm coping thickness; and 4) SLOW15, slow cooling and 1.5 mm coping thickness. Each zirconia-ceramic crown was cemented onto its abutment using a self-polymerizing resin cement (Multilink Automix, Ivoclar Vivadent). The crowns were then stored in distilled water before undergoing artificial aging.
The crown-abutment specimens were embedded in a self-polymerzing acrylic resin (Jet Tooth Shade, Lang Dental Manufacturing Co., Wheeling, IL, USA) at 1 mm apical from the crown margin. Each zirconia-ceramic crown was submitted to a fatigue load of 300,000 cycles using a chewing simulator with sliding movement (CS-4.8, SD Mechatronik, Feldkirchen-Westerham, Germany), which simulated 1 year of clinical function. The chewing simulator applied mechanical loading (50 N, 1.6 Hz) and thermal aging between 5℃ and 55℃ for 1263 times. After the completion of the chewing simulation, the zirconia-ceramics were carefully inspected using binocular magnifying (4×) glasses (Eye Mag Pro, Zeiss, Jena, Germany) to determine whether any chipping or fracture of the veneering ceramics or copings had occurred.
Each specimen that did not show any fracture or chipping after artificial aging was subjected to a fracture test by a universal loading device (Z 250/SN 5S, Zwick GmbH and Co., Ulm, Germany). Each test was performed at a crosshead speed of 0.5 mm/min. The load was applied 2 mm from the center of the occlusal surface, parallel to the long axis of the crown-abutment (Fig. 3). The loading stylus had a 4-mm diameter stainless steel ball. The maximum failure load was recorded in Newtons (N).
A statistical analysis was performed using a software package (IBM SPSS Statistics 20, IBM, Chicago, IL, USA). The Kolmogorov–Smirnov test was performed to check the normality of the data of each group. Based on the results of the normality test, two-way ANOVA was performed to analyze the significance of the failure load between the groups (α = 5%).
After undergoing chewing simulation, none of the zirconia-ceramic crown had cohesive or adhesive failure of the ceramic veneer. Therefore, all 40 specimens received a monotonic load until failure. One specimen from SLOW15 group did not fail until it was exposed to 8,000 N, which was the maximum force of the loading device. The degree of failure load was therefore regarded as 8,000 N for the specimen. Table 1 lists the mean and standard deviation of each group. Table 2 presents the results of two-way ANOVA, which was used to check the effect of different cooling rates, coping thicknesses, and the interaction between the different cooling rates and coping thicknesses.
The failure load is significantly influenced by the cooling rate (P = .003) and by the coping thickness (P < .001). The interaction between the cooling rate and the coping thickness also significantly influences the failure load (P = .001).
Under conventional cooling conditions, the difference in the coping thickness did not influence the mean failure load of the zirconia-ceramic crowns (P = .525). However, under slow cooling conditions, the coping thickness significantly influenced the mean failure load (P < .001).
With the thin coping, the difference in the cooling rate did not influence the mean failure load of the zirconia-ceramic crowns (P = .686). However, with the thick coping, the cooling rate significantly influenced the mean failure load of the zirconia-ceramic crowns (P < .001).
Figure 4 showed the typical failure aspects of 4 subgroups. CONV05 group showed small edge chipping without exposure of the zirconia coping, except for the margin area. Extended fracture of the veneer ceramic was present with a small area of exposed zirconia coping at the occlusal side in SLOW05 group.
In the current study, the mean failure loads were evaluated in zirconia-ceramic crowns with different cooling rates and coping thicknesses. The results of this study showed that a thicker zirconia coping and a slow cooling rate resulted in greater mean failure loads, compared to a thinner coping with a thicker veneer ceramic and conventional cooling. Therefore, the null hypothesis was rejected.
It was only possible to design nonanatomic copings with a uniform thickness in the early stages of dental CAD/CAM services. Nonanatomic copings resulted in areas of unsupported veneering ceramics, which is considered the main cause of the high chipping rate.25 Laboratory studies showed that greater failure loads or a fewer number of chippings occurred in zirconia-ceramic crowns with anatomic or thicker coping designs.262728 Mathematical analyses also showed that modifying the coping design with a lingual and proximal collar significantly increased the reliability of zirconia-ceramic crowns.29 However, compared to thin coping or uniform thickness zirconia coping designs, thick or anatomic coping designs have another issue, which is the thermal gradient problem. Tholey and his coworkers compared the temperature difference between the inner and outer surfaces of zirconia-ceramic crowns with two different coping designs.12 They reported that the anatomic coping resulted in a greater temperature difference between the inner and outer surfaces of the zirconia-ceramic crowns, compared to crowns with an even coping thickness, and that a greater temperature difference resulted in high residual tempering stresses. Furthermore, clinical studies reported a higher chipping rate and extended veneer fractures of zirconia-ceramic compared to metal-ceramics, even with anatomic coping designs.7,30,31 Therefore, the anatomic coping design is presumably insufficient to prevent veneer ceramic chipping in clinical practice. In addition to the coping designs, recent studies emphasize the influence of the cooling rate until attaining the glass transition temperature of veneer ceramics after the final firing. Swain17 reported that the residual stress in veneer ceramic was closely associated with chipping failure and that slow cooling decreased the amount of residual tensile stress in veneer ceramics.22,32 During the cooling process of metal-ceramics or aluminaceramics, the surrounding temperature is quickly transmitted through the coping material because of the higher thermal diffusivity of an alloy or alumina. Therefore, the type and amount of residual stresses were determined by the thickness of the veneer ceramics, not by the thickness of the coping or the total thickness of the coping and veneer ceramics. In contrast to alloys or alumina, zirconia has a very low thermal diffusivity. It retains heat for a certain amount of time rather than transmitting the surrounding temperature to the veneering ceramics. The amount and type of residual stress are governed by the sum of the veneer ceramic and the coping thickness of the zirconia-ceramic crowns,17 and slow cooling is important in zirconia-ceramics to compensate for the slow temperature transition through zirconia.
The most important finding of this study was that the mean failure load increased remarkably when zirconia-ceramic crowns with the thick coping had been slowly cooled after the final firing cycles, compared to the failure load of zirconia-ceramic crowns with a thick coping / conventional cooling or crowns with thin coping / slow cooling. In the zirconia-ceramic crowns that had the thick coping design, the mean failure load was not significantly increased when the crowns were conventionally cooled after the final firing. However, the mean failure load of the crowns with the thick coping was significantly increased when the crowns were slowly cooled until attaining the glass transition temperature of the veneer ceramic (Table 3; P < .001). These results are in agreement with the findings of the study by Tholey et al.12 As mentioned previously, the thicker coping produced higher residual tempering stress because of the greater temperature difference between the inner and outer surfaces of the zirconia-ceramic crowns. However, a smaller temperature difference occurred when the crowns were cooled slowly, which could decrease the residual stress.12
Statistical analysis showed that slow cooling did not significantly increase the mean failure loads when the zirconia-ceramic crowns had the thin coping (Table 4; P <.686), whereas slow cooling significantly increased the mean failure load when the coping was thick (P < .001). The thick coping likewise only effectively increased the mean failure load when the crowns were slowly cooled after the final firing. This result was clinically confirmed by the study of Rinke and colleagues,33 who reported comparable chipping rates of zirconia-ceramic crowns to those of metal-ceramics in 3 years of clinical service when the anatomic zirconia coping design and extra-cooling time were applied.
Each group presented different fracture patterns. The thinner coping (i.e., 0.5 mm) with the conventional cooling group showed a small edge chipping of the veneer ceramic. Extensive fracture of veneer ceramic or coping exposure was not observed in this group. The thin coping with the slow cooling group showed extensive fractures in the veneer ceramic. Most specimens showed zirconia coping exposure, but the exposed areas were limited. The thick coping (i.e., 1.5 mm) with the conventional cooling group showed extensive veneer fractures with a large area of zirconia coping exposure. One specimen in this group had a small amount of zirconia coping fracture at the cervical area (Fig. 4D). Six of 10 specimens in the thick coping and slow cooling rate group showed catastrophic zirconia coping fracture. The crowns were cut into two or three pieces and separated from the abutment.
The current study has some limitations. No chipping was introduced after 300,000 chewing cycles with 1263 thermal stimulations. Because of the lack of chipping after the chewing simulations, a monotonic load was applied to each crown until failure. In most clinical situations, a subcritical crack is propagated by small and repeated occlusal forces, not by a single catastrophic force such as a monotonic load. A chewing simulator is a very useful device for wear studies because it provides sliding movements. However, it has limitations in fatigue studies. Instead of a chewing simulator, a cyclic loading device with varying force would be appropriate to reproduce the intraoral fatigue condition.
The result of current study showed that coping thickness and cooling rate significantly influence the mean failure load of zirconia-ceramic crowns. There is an interaction between the coping thickness and cooling rate on the mean failure load of zirconia-ceramic crowns. Moreover, there is a significantly greater mean failure load when the zirconia-ceramic crowns have a thicker coping and are slowly cooled after the final firing.
Figures and Tables
 | Fig. 2A zirconia-ceramic crown with 1.5 mm coping thickness (A) and 0.5 mm coping thickness (B). Yellow color represents zirconia coping and blue color represents veneering ceramic. |
 | Fig. 3A monotonic load was applied 2 mm off center (2 mm from line-angle) of occlusal surface of each zirconia-ceramic crown. |
 | Fig. 4The fracture pattern of zirconia-ceramic crowns from each group. (A) 0.5-mm coping under the conventional cooling rate. (B) 0.5-mm coping under slow cooling. (C) 1.5-mm coping under conventional cooling, (D) 1.5-mm coping under slow cooling. |
Table 1
The means and standard deviations of the failure loads for 4 study groups

| Cooling rate | Coping thickness (mm) | Mean (Newtons) | Standard deviation (Newtons) | Number of specimens |
|---|---|---|---|---|
| Conventional | 0.5 | 2336.5 | 1378.0 | 10 |
| 1.5 | 2724.9 | 1411.2 | 10 | |
| Slow | 0.5 | 2089.7 | 663.4 | 10 |
| 1.5 | 5737.4 | 1733.1 | 10 |
Table 2
Two-way analysis of variance for the failure loads

Table 3
The effect of coping thickness under the different cooling rates

Table 4
The effect of the cooling rate under different coping thicknesses

References
1. Tinschert J, Schulze KA, Natt G, Latzke P, Heussen N, Spiekermann H. Clinical behavior of zirconia-based fixed partial dentures made of DC-Zirkon: 3-year results. Int J Prosthodont. 2008; 21:217–222.
2. Schmitt J, Holst S, Wichmann M, Reich S, Gollner M, Hamel J. Zirconia posterior fixed partial dentures: a prospective clinical 3-year follow-up. Int J Prosthodont. 2009; 22:597–603.
3. Pelaez J, Cogolludo PG, Serrano B, Serrano JF, Suarez MJ. A four-year prospective clinical evaluation of zirconia and metal-ceramic posterior fixed dental prostheses. Int J Prosthodont. 2012; 25:451–458.
4. Cosgarea R, Gasparik C, Dudea D, Culic B, Dannewitz B, Sculean A. Peri-implant soft tissue colour around titanium and zirconia abutments: a prospective randomized controlled clinical study. Clin Oral Implants Res. 2015; 26:537–544.
5. Sax C, Hämmerle CH, Sailer I. 10-year clinical outcomes of fixed dental prostheses with zirconia frameworks. Int J Comput Dent. 2011; 14:183–202.
6. Burke FJ, Crisp RJ, Cowan AJ, Lamb J, Thompson O, Tulloch N. Five-year clinical evaluation of zirconia-based bridges in patients in UK general dental practices. J Dent. 2013; 41:992–999.
7. Rinke S, Gersdorff N, Lange K, Roediger M. Prospective evaluation of zirconia posterior fixed partial dentures: 7-year clinical results. Int J Prosthodont. 2013; 26:164–171.
8. Rojas-Vizcaya F. Full zirconia fixed detachable implant-retained restorations manufactured from monolithic zirconia: clinical report after two years in service. J Prosthodont. 2011; 20:570–576.
9. Limmer B, Sanders AE, Reside G, Cooper LF. Complications and patient-centered outcomes with an implant-supported monolithic zirconia fixed dental prosthesis: 1 year results. J Prosthodont. 2014; 23:267–275.
10. Aboushelib MN, Feilzer AJ, Kleverlaan CJ. Bridging the gap between clinical failure and laboratory fracture strength tests using a fractographic approach. Dent Mater. 2009; 25:383–391.
11. Saito A, Komine F, Blatz MB, Matsumura H. A comparison of bond strength of layered veneering porcelains to zirconia and metal. J Prosthet Dent. 2010; 104:247–257.
12. Tholey MJ, Swain MV, Thiel N. Thermal gradients and residual stresses in veneered Y-TZP frameworks. Dent Mater. 2011; 27:1102–1110.
13. Bonfante EA, Rafferty B, Zavanelli RA, Silva NR, Rekow ED, Thompson VP, Coelho PG. Thermal/mechanical simulation and laboratory fatigue testing of an alternative yttria tetragonal zirconia polycrystal core-veneer all-ceramic layered crown design. Eur J Oral Sci. 2010; 118:202–209.
14. Silva NR, Bonfante EA, Rafferty BT, Zavanelli RA, Rekow ED, Thompson VP, Coelho PG. Modified Y-TZP core design improves all-ceramic crown reliability. J Dent Res. 2011; 90:104–108.
15. Aboushelib MN, Kleverlaan CJ, Feilzer AJ. Microtensile bond strength of different components of core veneered all-ceramic restorations. Part II: Zirconia veneering ceramics. Dent Mater. 2006; 22:857–863.
16. Aboushelib MN, Mirmohamadi H, Matinlinna JP, Kukk E, Ounsi HF, Salameh Z. Innovations in bonding to zirconiabased materials. Part II: Focusing on chemical interactions. Dent Mater. 2009; 25:989–993.
17. Swain MV. Unstable cracking (chipping) of veneering porcelain on all-ceramic dental crowns and fixed partial dentures. Acta Biomater. 2009; 5:1668–1677.
18. Guazzato M, Walton TR, Franklin W, Davis G, Bohl C, Klineberg I. Influence of thickness and cooling rate on development of spontaneous cracks in porcelain/zirconia structures. Aust Dent J. 2010; 55:306–310.
19. Mainjot AK, Schajer GS, Vanheusden AJ, Sadoun MJ. Influence of cooling rate on residual stress profile in veneering ceramic: measurement by hole-drilling. Dent Mater. 2011; 27:906–914.
20. Belli R, Frankenberger R, Appelt A, Schmitt J, Baratieri LN, Greil P, Lohbauer U. Thermal-induced residual stresses affect the lifetime of zirconia-veneer crowns. Dent Mater. 2013; 29:181–190.
21. Belli R, Monteiro S Jr, Baratieri LN, Katte H, Petschelt A, Lohbauer U. A photoelastic assessment of residual stresses in zirconia-veneer crowns. J Dent Res. 2012; 91:316–320.
22. Meira JB, Reis BR, Tanaka CB, Ballester RY, Cesar PF, Versluis A, Swain MV. Residual stresses in Y-TZP crowns due to changes in the thermal contraction coefficient of veneers. Dent Mater. 2013; 29:594–601.
23. Mainjot AK, Schajer GS, Vanheusden AJ, Sadoun MJ. Influence of zirconia framework thickness on residual stress profile in veneering ceramic: measurement by hole-drilling. Dent Mater. 2012; 28:378–384.
24. Mainjot AK, Schajer GS, Vanheusden AJ, Sadoun MJ. Influence of veneer thickness on residual stress profile in veneering ceramic: measurement by hole-drilling. Dent Mater. 2012; 28:160–167.
25. Rosentritt M, Behr M, Thaller C, Rudolph H, Feilzer A. Fracture performance of computer-aided manufactured zirconia and alloy crowns. Quintessence Int. 2009; 40:655–662.
26. Alhasanyah A, Vaidyanathan TK, Flinton RJ. Effect of core thickness differences on post-fatigue indentation fracture resistance of veneered zirconia crowns. J Prosthodont. 2013; 22:383–390.
27. Larsson C, El Madhoun S, Wennerberg A, Vult von Steyern P. Fracture strength of yttria-stabilized tetragonal zirconia polycrystals crowns with different design: an in vitro study. Clin Oral Implants Res. 2012; 23:820–826.
28. Rosentritt M, Steiger D, Behr M, Handel G, Kolbeck C. Influence of substructure design and spacer settings on the in vitro performance of molar zirconia crowns. J Dent. 2009; 37:978–983.
29. Guess PC, Bonfante EA, Silva NR, Coelho PG, Thompson VP. Effect of core design and veneering technique on damage and reliability of Y-TZP-supported crowns. Dent Mater. 2013; 29:307–316.
30. Sailer I, Gottnerb J, Kanelb S, Hammerle CH. Randomized controlled clinical trial of zirconia-ceramic and metal-ceramic posterior fixed dental prostheses: a 3-year follow-up. Int J Prosthodont. 2009; 22:553–560.
31. Schwarz S, Schröder C, Hassel A, Bömicke W, Rammelsberg P. Survival and chipping of zirconia-based and metal-ceramic implant-supported single crowns. Clin Implant Dent Relat Res. 2012; 14:e119–e125.
32. Rues S, Kröger E, Müller D, Schmitter M. Effect of firing protocols on cohesive failure of all-ceramic crowns. J Dent. 2010; 38:987–994.
33. Rinke S, Schäfer S, Lange K, Gersdorff N, Roediger M. Practice-based clinical evaluation of metal-ceramic and zirconia molar crowns: 3-year results. J Oral Rehabil. 2013; 40:228–237.




 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download