Abstract
PURPOSE
MATERIALS AND METHODS
RESULTS
Figures and Tables
 | Fig. 1Location of the strain gauge on implant. (A) Buccal surface of #43 implant, lingual surface of #33 implant, (B) Mesial surface of #43 implant, distal surface of #33 implant. |
 | Fig. 2Three types of vertical load were transferred to the experimental models. (A) Load was applied on the right mandibular first molar area, (B) Load was applied on the right posterior area, (C) Load was applied on the mandibular entire edentulous area. |
 | Fig. 3Extension of denture base was divided into three groups. (A) Group 1, (B) Group 2, (C) Group 3. |
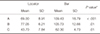
Table 1
Mean strain values (µm/m) and SD of Group 1 (n = 10)

43iB: Strain gauge on the buccal side of #43 implant, 43iM: Strain gauge on the mesial side of #43 implant, 33iL: Strain gauge on the lingual side of #33 implant, 33iD: Strain gauge on the distal side of #33 implant.
A: Vertical loading on the mandibular right first molar, B: Vertical loading on the mandibular right premolars and molars, C: Vertical loading on both mandibular posterior areas.
Table 2
Mean strain values (µm/m) and SD of Group 2 (n = 10)

43iB: Strain gauge on the buccal side of #43 implant, 43iM: Strain gauge on the mesial side of #43 implant, 33iL: Strain gauge on the lingual side of #33 implant, 33iD: Strain gauge on the distal side of #33 implant.
A: Vertical loading on the mandibular right first molar, B: Vertical loading on the mandibular right premolars and molars, C: Vertical loading on both mandibular posterior areas.
Table 3
Mean strain values (µm/m) and SD of Group 3 (n = 10)

43iB: Strain gauge on the buccal side of #43 implant, 43iM: Strain gauge on the mesial side of #43 implant, 33iL: Strain gauge on the lingual side of #33 implant, 33iD: Strain gauge on the distal side of #33 implant.
A: Vertical loading on the mandibular right first molar, B: Vertical loading on the mandibular right premolars and molars, C: Vertical loading on both mandibular posterior area.
Table 4
Comparison of P values between locator and bar/clip attachment
| Locator | Bar | P value* | |||
|---|---|---|---|---|---|
| Mean | SD | Mean | SD | ||
| A | 69.00 | 8.91 | 109.43 | 18.79 | < .001 |
| B | 77.05 | 6.21 | 105.73 | 12.66 | .01 |
| C | 43.70 | 7.84 | 62.30 | 4.73 | .01 |
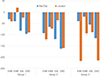
Table 5
Comparison of P values for locator attachment by differences in the denture base (P < .05)

| Group 1 | Group 2 | Group 3 | P value* | ||||
|---|---|---|---|---|---|---|---|
| Mean | SD | Mean | SD | Mean | SD | ||
| A | 69.00 | 8.91 | 84.43 | 8.19 | 112.58 | 8.32 | 0.03 |
| B | 77.05 | 6.21 | 86.63 | 8.47 | 116.80 | 11.56 | 0.03 |
| C | 43.70 | 7.84 | 97.50 | 6.09 | 153.88 | 8.57 | 0.01 |
*Significant difference at the 0.05 level.
Group 1: Full denture base, Group 2: Denture base reduction to level of distal area of second molar, Group 3: Denture base reduction to level of distal area of first molar.
A: Vertical loading on the mandibular right first molar, B: Vertical loading on the mandibular right premolars and molars, C: Vertical loading on both mandibular posterior areas.
Table 6
Comparison of the P values for bar/clip attachment by difference in the denture base (P < .05)

| Group 1 | Group 2 | Group 3 | P value* | ||||
|---|---|---|---|---|---|---|---|
| Mean | SD | Mean | SD | Mean | SD | ||
| A | 109.43 | 18.79 | 148.45 | 6.08 | 0173.38 | 10.63 | 0.001 |
| B | 105.73 | 12.66 | 144.78 | 8.79 | 170.55 | 6.57 | 0.02 |
| C | 62.30 | 4.73 | 110.28 | 5.60 | 57.60 | 3.73 | 0.02 |
*Significant difference at the 0.05 level.
Group 1: Full denture base, Group 2: Denture base reduction to level of distal area of second molar, Group 3: Denture base reduction to level of distal area of first molar A: Vertical loading on the mandibular right first molar, B: Vertical loading on the mandibular right premolars and molars, C: Vertical loading on both mandibular posterior areas.




 PDF
PDF ePub
ePub Citation
Citation Print
Print





 XML Download
XML Download