Abstract
PURPOSE
Although magnetic attachment is used frequently for overdenture, it is reported that attractive force can be decreased by abrasion and corrosion. The purpose of this study was to establish the clinical basis about considerations and long term prognosis of overdenture using magnetic attachments by investigating the change in attractive force of magnetic attachment applied to the patients.
MATERIALS AND METHODS
Among the patients treated with overdenture using magnetic attachments in Dankook University Dental Hospital, attractive force records of 61 magnetic attachments of 20 subjects who re-visited from July 2013 to June 2014 were analyzed. Dental magnet tester (Aichi Micro Intelligent Co., Aichi, Japan) was used for measurement. The magnetic attachments used in this study were Magfit IP-B Flat, Magfit DX400, Magfit DX600 and Magfit DX800 (Aichi Steel Co., Aichi, Japan) filled with Neodymium (NdFeB), a rare-earth magnet.
RESULTS
Reduction ratio of attractive force had no significant correlation with conditional variables to which attachments were applied, and was higher when the maintenance period was longer (P<.05, r=.361). Reduction ratio of attractive force was significantly higher in the subject group in which attachments were used over 9 years than within 9 years (P<.05). Furthermore, 16.39% of total magnetic attachments showed detachment of keeper or assembly.
CONCLUSION
Attractive force of magnetic attachment is maintained regardless of conditional variables and reduction ratio increased as the maintenance period became longer. Further study on adhesive material, attachment method and design improvement to prevent detachment of magnetic attachment is needed.
Recently, due to improvement in medicine, population is aging rapidly with increasing number of partial or complete edentulous patients. Complications of tooth loss such as resorption of residual alveolar ridge, collapsed appearance, deterioration of oral function and lowered self-esteem may occur, thus increasing the demand for prosthetic treatment. Treatments with dentures to solve these complications are considered to contribute to the quality of life in edentulous patients. This treatment acquired its scientific, theoretical background over long period of time and attained esthetic goals by sophisticated techniques. However, functional properties such as efficiency and force of mastication are not considered successful.12 Previous studies reported that most of the denture patients were not satisfied with their dentures34 due to loose dentures, problems with pronunciation, and decreased mastication efficiency.
In 1958, Miller5 systemized the concept of overdentures - distributing the stress to abutment teeth and supporting tissues - and this was applied not only to complete dentures but also partial dentures. This concept has been clinically utilized as an alternative to conventional dentures because overdentures increase retention and stability as well as mastication efficiency by using residual natural teeth or implants as abutments, prevent alveolar bone resorption and preserve vertical dimension.6789101112131415
Since then, continuous attempts to achieve increased retention and stability were made and attachments to mechanically fix, retain, and stabilize dentures were invented and developed.161718
Removable overdentures which increase support and retention by attaching various attachments to natural teeth and implants are preferred and are widely used because of easy maintenance of oral hygiene and more esthetic results.
Among various attachments, magnetic attachments have advantages that they can maintain a constant initial attractive force during maintenance period, are small in size, are easy to install into prostheses and the patient has no difficulty in inserting and removing the denture.1920 In addition, patients are more satisfied because metal components are not exposed. Also, they can be applied to the patients who are considered to have bad prognosis when other attachments are used, because magnetic attachments prevent the abutment from traumatic injury by lateral force of upper prosthesis. Moreover, when dentures are slightly displaced, magnetic attachments return them back to their original position.2122
However, there are reports that abrasion and corrosion due to the direct load to the magnetic attachments or dislodgement of sealing because of inadequate welding procedure may lead to the decreased attractive force of magnetic attachment, thus lowering the retentive force of attachments.232425 Therefore, the clinical study concerning the effectiveness and long-term prognosis of magnetic attachments are needed.
Considering that the oral cavity remains moist due to saliva, and that the tongue and the muscles around the oral cavity make it mechanically unstable and mobile, the environment of oral cavity differs enormously from that of extraoral. Additionally, implants and teeth have different mastication capacity because they perceive occlusal contact by different proprioception. Occlusal status is different according to the type of residual dentition and restoration, and occlusal force differs between genders. These variations influence the prognosis of attachments in dentures and the longer the attachments remain in the denture, the more possible that they might be exposed to the environment which may deteriorate attractive force.
In these circumstances, this study focuses on determining the difference of variation in attractive force based on the measurements in clinical magnetic attachments and its correlation with gender, its location and the type of abutment teeth, the type of overdenture, the type of magnetic attachment, relationship with the abutment teeth and applied period. Thus, the object of this study was to determine the considerations when treating with overdentures using magnetic attachments and clinical basis of its long-term prognosis.
The magnetic attachments for overdenture used in this study were Magfit IP-B Flat, Magfit DX400, Magfit DX600 and Magfit DX800 (Aichi Steel Co., Aichi, Japan) which were filled with Neodymium (NdFeB), a rare-earth magnet. Table 1 indicates the types and sizes of magnetic attachments.
Dental magnet tester (Aichi Micro Intelligent Co., Aichi, Japan) was used to measure attractive force at the assemblies of magnetic attachments.
Among the patients treated with overdentures using magnetic attachments at Dankook University Dental Hospital, patients with dental records including attractive force measurement were selected. In this study, records of 20 patients who re-visited the Department of Prosthodontics from July, 2013 to June, 2014 for follow-up treatment were used. 61 magnetic attachments were used in total (IRB NO. H-1406/008/001).
Dental magnet tester was held firmly with device clip holder (Szstella Co., Seoul, Korea) and the tip of the tester was positioned to contact the four types of new magnetic attachment assemblies (Aichi Steel Co., Aichi, Japan) used in this study. Initial attractive force was measured 10 times for each 10 types of magnetic attachments and the mean value was calculated.
The attractive force of magnetic attachment assemblies applied in overdenture was measured again when the patients re-visited. During the measuring procedure, dental magnet tester was held firmly as it was held at the initial measurement to keep the surrounding magnetic field. The tester was turned on and attractive force was measured. The measuring procedure was repeated 10 times and performed by one researcher to minimize the error.
The difference between initial and final attractive force was obtained in percentages and reduction ratio of attractive force was calculated, except for one data in which the magnetic attachment assembly was detached and lost at the time of re-visit. The difference of reduction ratio of attractive force was analyzed according to the patients' gender, the type of abutment, the distribution and location of attachments, the type of overdenture, the type of magnetic attachment, the type of opposite dentition and applied period (Table 2).
SPSS 21.0 (IBM Corp., New York, NY, USA) was used for statistical analysis. Results according to the patients' gender, the type of abutment teeth, the distribution and position of attachments, and the type of overdenture were compared by Independent t-test. Significance of the difference caused by the type of magnetic attachment, and the type of opposite dentition was determined with Kruskal-Wallis test. Also, results by the applied period were analyzed with One-way ANOVA and Correlation analysis to determine the correlation. Post hoc testing for statistical significance was done with Tukey HSD test under 95% confidence interval.
Initial attractive force was measured 10 times for each of 10 magnetic attachments of all four types of new magnetic attachments and the results are shown in Table 3 and Table 4. The mean initial attractive force (± SD) of four types of magnetic attachment assemblies are as follow; 848.40 (± 11.31) gf in Magfit IP, 424.00 (± 11.52) gf in Magfit DX400, 688.00 (± 16.35) gf in Magfit DX600 and 838.00 (± 11.07) gf in Magfit DX800.
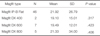
One patient whose magnetic attachment assembly was detached and lost at the time of re-visit was excluded and the total number of male and female patients were 12 and 7 respectively. Male and female patients had 36 and 24 magnetic attachments in their dentures respectively. The reduction ratio of attractive force was 20.41 (± 24.51)% in male and 23.12 (± 27.12)% in female. Attractive force decreased more in female patients, but the difference was not statistically significant (Table 3).
Abutments with magnetic attachment were 12 natural teeth and 48 implants. The mean values of reduction ratio of attractive force were 22.31 (± 21.82)% in natural teeth and 21.29 (± 26.42)% in implants. The reduction ratio of attractive force in natural teeth was more than that in implants' but the difference was not statistically significant (Table 4).
Twenty eight magnetic attachments for overdentures were installed at maxilla and 32 in mandible. The mean values of reduction ratio of attractive force were 20.70 (± 28.34)% in maxilla and 22.18 (± 22.96)% in mandible. Attractive force decreased more in mandible than in maxilla but the difference was not statistically significant (Table 5).
Overdentures using magnetic attachment were as follow; 16 complete overdentures, 3 partial overdentures. The number of magnetic attachments beneath the complete dentures and partial dentures was 50 and 10, respectively. The mean values of reduction ratio of attractive force of magnetic attachments in complete dentures was 21.21 (± 25.04)% and 22.90 (± 28.48)% in partial dentures. The reduction ratio of partial dentures was more than that of complete dentures, but the difference was not statistically significant (Table 6).
Four types of magnetic attachments, Magfit IP, Magfit DX400, Magfit DX600, Magfit DX800 were used and 46, 2, 7, 5 were applied , respectively. The mean reduction ratio was 21.92 (± 26.79)% in Magfit IP, 19.10 (± 15.01)% in Magfit DX400, 19.49 (± 12.01)% in Magfit DX600 and 21.33 (± 34.00)% in Magfit DX800 in the order of Magfit IP, Magfit DX800, Magfit DX600 and Magfit DX400 according to higher value. However, the differences were not statistically significant (Table 7).
The types of opposite dentitions to overdentures with magnetic attachments were complete denture, partial denture, and full dentition, the numbers being 35, 9, and 16, respectively. The mean reduction ratio was 21.35 (± 26.16)% with complete denture, 25.05 (± 25.35)% with partial denture and 19.80 (± 25.15)% with full dentition, in order of partial denture, complete denture and full dentition according to higher value. However, the differences were not statistically significant (Table 8).
Applied period was calculated from the timing when the magnetic attachments were installed into patients' overdentures. 7 magnetic attachments were applied for less than 3 years, 26 for 3 - 6 years, 17 for 6 - 9 years and 10 for more than 9 years. The mean values (± SD) of reduction rate were 6.46 (± 4.14) for less than 3 years, 16.80 (± 24.74)% for 3 - 6 years, 20.19 (± 16.73)% for 6 - 9 years and 46.42 (± 32.96)% for more than 9 years. Reduction ratios had positive correlation with applied period (r=0.361, P < .05) and reduction ratio of the group with more than 9 years of applied period was significantly more than that of other groups (P < .05) (Table 9).
Overdentures that were invented to overcome the disadvantages found in complete dentures and partial dentures not only enhance retention and stability compared to conventional dentures, but reduce further resorption of alveolar bone and maintain vertical dimension. Numerous studies about overdentures were reported and the concept of available abutments for increased retention and stability were expanded from only residual teeth or implants to various types of attachments, such as Bar, Ball & Socket, ERA, Locator, magnetic attachments.
Overdentures with magnetic attachments used in this study were frequently applied from early 1980s but utilizing magnets in denture treatment was reported earlier. Behrman and Egan26 increased stability and retention of dentures by placing different poles of magnets at the jaw and the denture. Freedman27 in 1953 and Winkler and Pearson28 in 1967 suggested placing the same magnetic pole at both maxillary and mandibular dentures to gain retention and stability by the repulsive force of magnet. Also, connecting intraoral prosthesis or maxillofacial prosthesis with magnets to restore maxillofacial defects had been introduced.2930
Because of its small size, magnetic attachments can be used even when the vertical dimension is deficient. Magnetic attachments are easy to install and can prevent abutment teeth from being damaged by lateral forces. Also, magnetic attachments are readily applied in short implants or poor bone quality area and the denture with magnetic attachments can be easily worn on and off.
However, Contradicting results concerning the retention force of attachments, which is, the most important factor, have been reported. Naert et al.31 and Burns et al.32 reported that the retention force of magnetic attachments is smaller than that of other attachments but it is maintained the longest and the magnetic attachments were able to function sufficiently with more than 400 gf of attractive force. In addition, Setz et al.33 reported that theoretically, attractive force of magnetic attachment remains constant and that the main cause of decrease in retention force is the gap between assembly and keeper. Riley et al.24 insisted that magnetic attachments are not preferred in the West because of decreased attractive force and corrosion due to the sealing failure, but Thean et al.34 reported that corrosion in magnet attachments was not observed for 3 years since the development of sealing system using laser welding.
Therefore, this study focused on observing the change in attractive force of magnetic attachments by numerous variables present in oral cavity and determining the considerations in fabricating overdentures with magnetic attachments and the clinical basis of long-term prognosis.
The four types of magnetic attachments used in this study showed the average initial attractive force over 400 gf as the manufacturer implied, and it was confirmed that the attractive force was stronger than the minimum retention force needed to be used as attachments. However, the magnetic attachments were fabricated by compressing rare-earth magnet powder which has stronger attractive force than the manufacturer implied in stainless steel and sealing by laser welding. For this reason it is challenging to fabricate to have the same attractive force as manufacturer implied. As a result, the standard attractive force and the measured value did not correspond. Also, this study is not a prospective study which would measure the attractive force of new magnetic attachment and re-measure the attractive force of the same magnetic attachment after a certain period of time. This study is rather a retrospective one which establishes initial attractive force through measuring attractive force in new products and calculates reduction ratio by measuring the attractive force of used magnetic attachments. Strictly speaking, the reduction ratio cannot be defined to be that of the same magnetic attachments; as a result, there were cases where the reduction ratio had negative values.
The mean reduction ratio of attractive force of total magnetic attachments was 21.49% and a patient's magnetic attachment of which attractive force could not be measured due to the detachment of assembly of magnetic attachment during the visit was excluded from statistics. However, two attachments of two patients which were located in the denture but completely lost attractive force were included in statistics.
As previously mentioned, intraoral condition in which attachments and dentures are located is greatly different from extraoral condition due to high humidity and fluid dynamic relation. This seems to influence the long term prognosis of dental prostheses.
This study was designed based on the ideas that if the load on denture is strong due to gender, types of overdentures, difference in proprioception between natural teeth and implants, difference in masticatory force due to difference in opposing dentition, abrasion and failure in sealing can occur and application of attachment on mandible can cause more reduction of attractive force than maxilla from corrosion because of more exposure to saliva. Furthermore, comparison of attractive force by maintenance period was added because it was thought as the maintenance period gets longer, the attachment is more exposed to conditions which can reduce the attractive force.
The problem which occurred during the study was irregular measurement values and high errors when the attractive force of attachments was measured repeatedly. This was error from measurement method and it seemed that measurement was not consistent because of the change in surrounding magnetic field when there was movement of device after turning on the magnet tester. Therefore, stable attractive force measurement values were attained by using a device which can fixate the magnet tester. This can be utilized in further studies on attractive force measurement of magnetic attachments.
Reduction ratio of attractive force of magnetic attachments as a result of this study did not correlate with variables such as gender of subjects, types of abutments to which attachments were applied, location of attachments, types of overdentures to which attachments were applied, types of magnetic attachments and types of opposing dentition (P > .05). These results can be interpreted that attractive force of magnetic attachments are maintained regardless of condition to which magnetic attachments are applied. This may be due to the development of corrosionresistant metal which protects magnetic attachments and the dramatic decrease in sealing failure due to development of micro laser welding technique.
Significant increase in reduction ratio of attractive force when the maintenance period was longer(r = .361, P < .05) seems to be caused by increased possibility of exposure to conditions which can reduce attractive force of magnetic attachments. Therefore, consideration of factors which can possibly reduce the attractive force other than many conditional variables introduced previously in this study and further study are needed. Furthermore, when the subject groups were divided by the maintenance period, magnetic attachments of the group whose maintenance period was over 9 years showed significantly higher reduction ratio of attractive force than those within 9 years (P < .05). This result, in consideration of mean reduction ratio of attractive force of total magnetic attachment in this study which is 21.49%, attractive force of magnetic attachments is consistent during maintenance period within 9 years. This clinically supports the previous literature that reported attractive force of magnetic attachment was maintained stably.2526
Among the subjects in this study, the total number of magnetic attachments which experienced detachment of keeper or assembly was 10, reaching 16.39%. It was found that these subjects had repair by re-visit except one subject. This detachment of assembly of magnetic attachment has been reported in previous studies. Therefore, studies on various adhesive materials for adhesion of attachment assembly to denture for prevention of detachment of magnetic attachment assembly and prevention method of detachment by modification of assembly design were reported. Detachment possibility of attachment can be changed by the technique and experience of dentist and development of adhesive method which is not influenced by the technique of dentist and additional adhesive materials and designs are needed.
Moreover, subjects in this study were patients treated with overdenture using magnetic attachments among the ones who visited the department of dental prosthodontics of Dankook University Dental Hospital regularly and were treated and managed. This made it possible to investigate subjects who had long maintenance period. However, the data did not follow a normal distribution because the number of subjects and specimens were insufficient, resulting in high standard deviation. Further study with more subjects and specimens is needed.
From this study, the conclusions are as follow;
Attractive force of magnetic attachments was maintained regardless of conditional variables such as gender of subjects, types of abutments to which attachments were applied, location of attachments, types of overdentures to which attachments were applied, types of magnetic attachments and types of opposing dentition.
Reduction ratio of attractive force was higher when the maintenance period was longer (r = .361, P < .05), and magnetic attachments showed stable maintenance of attractive force within 9 years compared to other groups by maintenance period (P < .05).
Initial attractive force of magnetic attachment was higher than the standard attractive force indicated by the manufacturer. Mean reduction ratio of attractive force was 21.49% and detachment ratio of attachment was 16.39%.
Figures and Tables
Table 1
Magnetic attachments used in this study

Table 2
Measurement of magnetic force of each attachment of the patients

Table 3
Statistical analysis of reduction ratio of magnetic force by gender using independent t-test (unit : %)

| Gender | N | Mean | SD | P value |
|---|---|---|---|---|
| Male | 36 | 20.41 | 24.51 | .663 |
| Female | 24 | 23.12 | 27.12 |
Table 4
Statistical analysis of reduction ratio of magnetic force by abutment type using independent t-test (unit : %)

| Abutment type | N | Mean | SD | P value |
|---|---|---|---|---|
| Natural teeth | 12 | 22.31 | 21.82 | .384 |
| Implant | 48 | 21.29 | 26.42 |
Table 5
Statistical analysis of reduction ratio of magnetic force by location using independent t-test (unit : %)

| Location | N | Mean | SD | P value |
|---|---|---|---|---|
| Maxilla | 28 | 20.70 | 28.34 | .812 |
| Mandible | 32 | 22.18 | 22.96 |
Table 6
Statistical analysis of reduction ratio of magnetic force by denture type using independent t-test (unit : %)

| Denture type | N | Mean | SD | P value |
|---|---|---|---|---|
| CD | 50 | 21.21 | 25.04 | .642 |
| RPD | 10 | 22.90 | 28.48 |
Table 7
Statistical analysis of reduction ratio of magnetic force by Magfit type using Kruskal-Wallis test (unit : %)
| Magfit type | N | Mean | SD | P value |
|---|---|---|---|---|
| Magfit IP-B Flat | 46 | 21.92 | 26.79 | |
| Magfit DX 400 | 2 | 19.10 | 15.01 | .317 |
| Magfit DX 600 | 7 | 19.49 | 12.01 | .423 |
| Magfit DX 800 | 5 | 21.33 | 34.00 | .406 |
Table 8
Statistical analysis of reduction ratio of magnetic force by opposite dentition using Kruskal-Wallis test (unit : %)

| Opposite dentition | N | Mean | SD | P value |
|---|---|---|---|---|
| CD | 35 | 21.35 | 26.16 | |
| RPD | 9 | 25.05 | 25.35 | .433 |
| Full dentition | 16 | 19.80 | 25.15 | .451 |
References
1. Haraldson T, Karlsson U, Carlsson GE. Bite force and oral function in complete denture wearers. J Oral Rehabil. 1979; 6:41–48.
2. Osterberg T, Carlsson GE. Symptoms and signs of mandibular dysfunction in 70-year-old men and women in Gothenburg, Sweden. Community Dent Oral Epidemiol. 1979; 7:315–321.
3. Ellis JS, Pelekis ND, Thomason JM. Conventional rehabilitation of edentulous patients: the impact on oral health-related quality of life and patient satisfaction. J Prosthodont. 2007; 16:37–42.
4. Turkyilmaz I, Company AM, McGlumphy EA. Should edentulous patients be constrained to removable complete dentures? The use of dental implants to improve the quality of life for edentulous patients. Gerodontology. 2010; 27:3–10.
5. Miller PA. Complete dentures supported by natural teeth. J Prosthet Dent. 1958; 8:924–928.
6. Morrow RM, Feldmann EE, Rudd KD, Trovillion HM. Tooth-supported complete dentures: an approach to preventive prosthodontics. J Prosthet Dent. 1969; 21:513–522.
7. Lord JL, Teel S. The overdenture: patient selection, use of copings, and follow-up evaluation. J Prosthet Dent. 1974; 32:41–51.
8. Morrow RM, Powell JM, Jameson WS, Jewson LG, Rudd KD. Tooth-supported complete dentures: description and clinical evaluation of a simplified technique. J Prosthet Dent. 1969; 22:415–424.
9. Dodge CA. Prevention of complete denture problems by use of "overdentures". J Prosthet Dent. 1973; 30:403–411.
10. Ettinger RL, Taylor TD, Scandrett FR. Treatment needs of overdenture patients in a longitudinal study: five-year results. J Prosthet Dent. 1984; 52:532–537.
11. Parel SM. Implants and overdentures: the osseointegrated approach with conventional and compromised applications. Int J Oral Maxillofac Implants. 1986; 1:93–99.
12. Crum RJ, Rooney GE Jr. Alveolar bone loss in overdentures: a 5-year study. J Prosthet Dent. 1978; 40:610–613.
13. Rissin L, House JE, Manly RS, Kapur KK. Clinical comparison of masticatory performance and electromyographic activity of patients with complete dentures, overdentures, and natural teeth. J Prosthet Dent. 1978; 39:508–511.
14. Reitz PV, Weiner MG, Levin B. An overdenture survey: preliminary report. J Prosthet Dent. 1977; 37:246–258.
15. Fenton AH, Hahn N. Tissue response to overdenture therapy. J Prosthet Dent. 1978; 40:492–498.
16. Thayer HH, Caputo AA. Photoelastic stess analysis of overdenture attachments. J Prosthet Dent. 1980; 43:611–617.
17. Stansbury BE. A retentive attachment for overdentures. J Prosthet Dent. 1976; 35:228–230.
18. Quinlivan JT. An attachment for overlay dentures. J Prosthet Dent. 1974; 32:256–261.
19. Khoo HD, Chai J, Chow TW. Prosthetic outcome, patient complaints, and nutritional effects on elderly patients with magnet-retained, implant-supported overdentures-a 1-year report. Int J Oral Maxillofac Implants. 2013; 28:1278–1285.
20. Gillings BR. Magnetic retention for complete and partial overdentures. Part I. J Prosthet Dent. 1981; 45:484–491.
21. Taira Y, Hai K, Matsumura H, Atsuta M. Adhesive bonding of titanium nitride-plated stainless steel for magnetic attachments. Eur J Oral Sci. 2001; 109:204–207.
22. Gillings BR. Magnetic retention for overdentures. Part II. J Prosthet Dent. 1983; 49:607–618.
23. Naert I, Quirynen M, Theuniers G, van Steenberghe D. Prosthetic aspects of osseointegrated fixtures supporting overdentures. A 4-year report. J Prosthet Dent. 1991; 65:671–680.
24. Riley MA, Williams AJ, Speight JD, Walmsley AD, Harris IR. Investigations into the failure of dental magnets. Int J Prosthodont. 1999; 12:249–254.
25. Naert I, Alsaadi G, Quirynen M. Prosthetic aspects and patient satisfaction with two-implant-retained mandibular overdentures: a 10-year randomized clinical study. Int J Prosthodont. 2004; 17:401–410.
26. Behrman SJ, Egan GF. The implantation of magnets in the jaw to aid denture retention : An original brief research report. New York State Dent J. 1953; 19:353–371.
27. Freedman H. Magnets to stabilize dentures. J Am Dent Assoc. 1953; 47:288–297.
28. Winkler S, Pearson MH. The effectiveness of embedded magnets in complete dentures during speech and mastication: a cineradiographic study. Dent Dig. 1967; 73:118–119.
29. Boucher LJ, Heupel EM. Prosthetic restoration of a maxilla and associated structures. J Prosthet Dent. 1966; 16:154–168.
30. Javid N. The use of magnets in a maxillofacial prosthesis. J Prosthet Dent. 1971; 25:334–341.
31. Naert IE, Gizani S, Vuylsteke M, van Steenberghe D. A randomised clinical trial on the influence of splinted and unsplinted oral implants in mandibular overdenture therapy. A 3-year report. Clin Oral Investig. 1997; 1:81–88.
32. Burns DR, Unger JW, Elswick RK Jr, Giglio JA. Prospective clinical evaluation of mandibular implant overdentures: Part II--Patient satisfaction and preference. J Prosthet Dent. 1995; 73:364–369.
33. Setz JM, Wright PS, Ferman AM. Effects of attachment type on the mobility of implant-stabilized overdentures--an in vitro study. Int J Prosthodont. 2000; 13:494–499.
34. Thean HP, Khor SK, Loh PL. Viability of magnetic denture retainers: a 3-year case report. Quintessence Int. 2001; 32:517–520.




 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download