Abstract
PURPOSE
The purpose of this study is to evaluate the stability of interface between Co-Cr-Mo (CCM) UCLA abutment and external hex implant.
MATERIALS AND METHODS
Sixteen external hex implant fixtures were assigned to two groups (CCM and Gold group) and were embedded in molds using clear acrylic resin. Screw-retained prostheses were constructed using CCM UCLA abutment and Gold UCLA abutment. The external implant fixture and screw-retained prostheses were connected using abutment screws. After the abutments were tightened to 30 Ncm torque, 5 kg thermocyclic functional loading was applied by chewing simulator. A target of 1.0 × 106 cycles was applied. After cyclic loading, removal torque values were recorded using a driving torque tester, and the interface between implant fixture and abutment was evaluated by scanning electronic microscope (SEM). The means and standard deviations (SD) between the CCM and Gold groups were analyzed with independent t-test at the significance level of 0.05.
RESULTS
Fractures of crowns, abutments, abutment screws, and fixtures and loosening of abutment screws were not observed after thermocyclic loading. There were no statistically significant differences at the recorded removal torque values between CCM and Gold groups (P>.05). SEM analysis revealed that remarkable wear patterns were observed at the abutment interface only for Gold UCLA abutments. Those patterns were not observed for other specimens.
Dental implant has been recognized as an effective rehabilitation method for edentulous area, and the success rate of dental implant is very high.123 Dental implants are becoming more popular, and the major expenses are being invested in materials and components used to make implant prosthesis. Different abutments can be used in cases where sufficient interarch distance is available. However, for cases with insufficient interarch distance where prosthesis retrieval is not possible, UCLA abutment can be utilized as screw-retained form. This can be performed by combining the abutment with superstructure through casting. The UCLA abutment can be connected directly to the implant fixture when considering the bone resorption pattern and the position of the opposing dentition. This method has an advantage in forming the emergence profile,4 and gold alloy has been a choice of material for this case. However, due to a dramatic increase in the price of gold, other materials with economic advantage are now emerging as alternatives. Proposed alternative abutment materials include Zirconia, Titanium alloy, and Co-CR-Mo (CCM) alloy, and many studies of these materials have been performed both in vitro and in vivo.567
Of the materials mentioned above, CCM alloy has been used to construct artificial joints in orthopedics since the early 1990s.8 Recently, the abutments manufactured with CCM alloy have become commercially available, and clinical cases have also been reported. However, biological safety, mechanical stability, and performance compared with gold abutments have not been fully investigated, and there is a lack of published studies of CCM UCLA abutments in implant prostheses. CCM alloy forms a thicker oxidized layer than other alloys when casted at high temperature. Also, although the manufacturing process may cause differences in strength and hardness, CCM alloy has higher strength and hardness than gold alloy and titanium alloys. On the other hand, the problem can be raised with regards to the use of CCM UCLA abutment since the surface treatment to remove thick oxidized layer can harm the interface between implant fixture and abutment by disturbing the screw joint stability.
The null hypothesis is that thermocyclic functional loading does not affect the removal torque value or interface wear patterns for prostheses using either CCM or Gold UCLA abutments. The purpose of this study was to evaluate the stability of interface between CCM UCLA abutment and external hex implant.
16 external hex implants (US II, Osstem Co., Seoul, Korea) with a diameter of 4.1 mm and a length of 15 mm were used.
The Gold UCLA abutment was cast using a gold alloy; a centrifugal casting machine was used to produce the gold crown from the wax pattern, which had a diameter of 7 mm and a height of 8 mm. A total of eight specimens were fabricated for this group. The CCM UCLA abutment was cast using Ni-Cr alloy for PFM crown; a centrifugal casting machine was used to produce the abutment from the wax pattern, which had a diameter of 7 mm and a height of 8 mm. To simulate making the PFM crown, the prosthesis was burned out. After burn-out, the oxidized layer was removed using glass beads under approximately 4 - 6 bars pressure, and then the prosthesis was polished using laboratory handpiece and rouge equipped with a cotton wheel. A total of eight specimens were fabricated for this group.
A standard mold was used, consistent with the mold used in chewing simulator CS4 (SD Mechatronic, Feldkirchen, Westerham, Germany) (Fig. 1). A fixture was embedded in the prepared mold with clear acrylic resin (Ortho-jet self-curing acrylic resin, Lang dental manufacturing Co Inc., Wheeling, IL, USA) to fill the mold (Fig. 2). It was also ensured that the upper-most margin of the mold was consistent with the margin 1 mm under the interface between fixture and abutment while the mold was completely filled with resin. The mold was incrementally filled with resin twice to avoid polymerization shrinkage.
The superstructure was connected to the fixture, which was embedded in the abutment screw. To simulate clinical procedure during connection, screw tightening was performed with a hand torque wrench at 30 Ncm torque. The screws were tightened three times in 10 minutes intervals.910 Table 1 presents the alloy and screw materials used for the implant fixture and the abutment hex structure.
The mold was placed into the chewing simulator (Fig. 2), and the stylus was positioned 3 mm away from the crown center. The cyclic loading procedure could produce a space at the interface between the mold and resin. Therefore, when the set value was inserted into the computer program and the simulation started (Table 2), it was ensured that the pin inside the mould was positioned perpendicularly to the stylus axis.
Removal torque value was measured after cyclic loading. A driving torque tester (Biomaterials Korea Inc., Seoul, Korea) was used to measure the removal torque value. The advantage of this tester was that it had constant rotational velocity and vertical load, which ensured reproducibility. The driving torque tester was rotated counter-clockwise at 3 rpm. The removal torque value was recorded every 0.1 seconds using the QuickDataAcq software program (SDK Developer, London, UK). The first peak of the resulting data was selected as the representative value.
After measuring the removal torque value, the abutment screw was removed, and the fixture and abutment were separated. Scanning electron microscopy (SEM) was performed, and micrographs were taken above the hex structure at 50×magnification (S-800, Hitachi, Ltd., Tokyo, Japan).
Independent t-tests were conducted based on the calculated mean and standard deviation of the removal torque values for Gold and CCM UCLA abutments. SPSS version 18.0 for Windows (SPSS Inc., Chicago, IL, USA) was used for statistical analyses.
In chewing simulation, loosening of abutment screw and fracture or deformation of prosthesis or implant fixture were not observed. The typical graph taken from representative samples, showing changes of removal torque value with respect to elapse of time (every 0.1 seconds) is presented in Fig. 3. The first peak in each graph was selected as the representative value. The tendency for most graphs is that removal torque value steeply increased up to the first peak then gradually decreased.
Fig. 4 shows means and standard deviations in each group. In Gold group, the minimum value was recorded as 16.60 (in Ncm) and the maximum value was recorded as 25.35 (in Ncm). In CCM group, the minimum value was 13.31 and the maximum was 25.11. The mean values in Gold group and CCM group were 20.31 and 20.38, respectively. In independent t-test, the P-value was 0.976 (>.05) and there was no significant difference between the two groups.
At the interface of CCM UCLA abutment, no remarkable wear patterns were observed (Fig. 5). In contrast, at the interface of Gold UCLA abutment, wear patterns were observed in the shape of a concentric circle around the screw hole. In the case with Gold abutment, remarkable wear patterns were observed, and most specimens showed irregular scratches at the surface of the interface (Fig. 6).
At the interface of fixture in Gold and CCM group, it showed areas that had contacts with abutment in the shape of concentric circle around the screw hole, but remarkable wear patterns were not observed. The CCM abutment has greater physical strength and hardness than implant fixture, so it was expected that it would show more remarkable wear patterns. However, from the result of SEM photographs, it appeared that there were no considerable mechanical damages (Fig. 7, Fig. 8).
In this study, we measured the removal torque value to evaluate the interface between abutment and fixture on the prosthesis using Gold and CCM UCLA abutment, by investigating the differences in stability between the two groups.
Henry et al.11 reported that the most frequent complication of a single implant restoration during the first 5 years was screw loosening. Becker and Becker12 reported that screw loosening in the molar region occurred in approximately 38% of all prostheses, and other studies showed that screw loosening was the most frequent complication in dental implant restorations. Screw loosening enables plaque accumulation in the gap at the prosthesis-abutment interface. The screw can be fractured once it becomes loosened and is subject to continual loading. There are also greater fracture risks for loosened screws when additional loading is applied to the adjacent implant.13
In this study, removal torque value was measured to evaluate the stability of screw joint. A hand torque wrench was used to tighten the screws, using the same method as that used in clinical practice. After chewing simulation, driving torque tester was used for measuring the removal torque value. Goheen et al.14 reported that errors can occur during manual screw tightening and that a mechanical tightening device must be used to avoid these errors. Torque control device used in this study can limit the maximum torque by folding anterior portion of the handle. However, torque error still occurs even with the aid of this torque device,15 which ranges from 17.0 - 58.6%.16 For an external hex implant connected with a butt-joint, 90% of the tightening torque was needed to overcome the friction at the screw contact surfaces, whereas 10% of the torque was converted to preload.17 In the current study, the preload transmitted out to the screw joint and the removal torque value were measured using a driving torque tester because it was reported to show higher reproducibility.18 Standlee et al.19 reported that the screw tightening speed also influenced the preload. Considering these combined results, we attempted to conduct the screw tightening procedure using the same method as that used in clinical practice.
The screws used in this study were composed of the following materials: titanium alloy was used for the CCM UCLA group, and ebony gold coated with tungsten carbide and carbon was used for the Gold UCLA group. The factors influencing preload produced by screw tightening include tension of friction, yield strength of screw material, elastic modulus, and fatigue.20 The friction coefficient is influenced by hardness of screw thread, torque speed, surface treatment, and presence and quality of lubricant.131521 As different abutment screws were used in the two groups in our study, conclusions drawn from direct comparisons between the two groups may be subject to errors. The study comparing titanium and gold screws by Haack et al.17 reported yield strengths of 110 and 99.36 Gpa, respectively. When the manufacturer-recommended torque was applied, the yield strengths of titanium and gold screws were 56 and 57.7%, respectively, although the extent of screw elongation and the preload were greater for gold screws. They also reported that titanium screws had lower removal torque values when subjected to more cycles of tightening and loosening. However, Jörnéus et al.22 reported that the screw tightening torque was more important than the screw materials; therefore, the effect of producing the proper preload using a torque wrench was a more important factor for the outcome than the type of screw materials and configuration. The fixture-abutment interface of an external hex implant is less stable than that of an internal hex implant. However, Theoharidou et al.23 reported that both external and internal hex implants for single implant restorations had similar screw loosening frequencies of 97.6 and 93.7%, respectively. In the current study, both titanium and ebony gold screws had the same recommended torque of 30 Ncm, and the two materials were fundamentally titanium alloy. Although the surface treatment might have influenced the result, we attempted to apply the same torque as that applied by Jörnéus et al.,22 who emphasized the importance of torque tightening. In this study, tightening torque was applied three times with 10 minutes interval so that elongation of screw could be guided. Therefore, the preload was reduced primarily due to the settling effect910 during screw loosening. Our simulation imposed 1,000,000 chewing cycles with 5 kg of loading. In the study by Truninger et al.,24 which reflected the simulation of loading condition in anterior portion, oblique force was loaded to abutment in 30 angles to the long axis of the crown. Bates et al.25 reported that the maximum force of mastication in the first human molar was 300 - 500 N. Richter26 reported that the vertical load in molar and premolar was 120 - 150 N. In our study, we designed the loading position to be 3 mm distant from the centre of the crown; therefore, this experimental design simulated the lateral masticatory force. Although the force loaded in the current study was less than the average masticatory force reported in the literature, it was believed to sufficiently simulate the intraoral environment by reconstructing the dynamic intraoral masticatory forces using the chewing simulator.
The mean removal torque values measured after chewing simulation using thermocyclic functional loading were 20.31 and 20.38 Ncm for the Gold and CCM UCLA abutments, respectively. The number of recorded data points that fell outside of the standard deviation was 4 for the Gold UCLA abutment group and 1 for the CCM UCLA abutment group. The differences between maximum and minimum removal torque values were 8.75 and 11.80 Ncm for the Gold and CCM UCLA abutments, respectively. The mean removal torque values and the recorded data distributions did not significantly differ between the Gold and CCM UCLA abutment groups.
The pattern of changes of removal torque value recorded in the graph after chewing simulation showed the following observations: removal torque steeply increased up to the first peak; it was thought that the given preload was completely lost; and then removal torque value decreased gradually showing consistent values. It was thought that consistent value could be explained by the friction between fixture and abutment screw. Generally, in external hex implant, strain results from tightening rotational force and external loading is concentrated on the abutment screw,27 and the only force is the preload of abutment screw, imposed at the abutment-implant fixture interface.28 From this point of view, the stability of abutment-fixture interface is equivalent for the two groups, based on similar mean removal torque values, standard deviations, and removal torque value distribution patterns with respect to elapsed time. However, the SEM micrographs did not reveal any significant wear patterns for the abutment interfaces of the CCM UCLA abutment group, whereas remarkable wear patterns and irregular scratches were observed at the abutment interfaces on most specimens of the Gold UCLA abutment group. It is challenging to evaluate which group had greater wear based only on SEM micrographs, but we can anticipate that wear patterns at the interface of the CCM group will be more destructive due to differences in strength and hardness between CCM and titanium alloys. The CCM alloy may cause significant mechanical damage to the fixture when loaded for long periods. The current study did not simulate sufficiently extended loading conditions to accurately predict long-term clinical outcome. Future studies will be necessary to study the actual masticatory force effects under extensively prolonged cyclic loading conditions.
There is not enough evidence on CCM UCLA abutments in vivo and in vitro, although they are commercially available. Therefore, detailed studies are required to predict any potential problems before their use becomes widespread in clinical practice. Further studies on clinical applications of internal hex implants and multiple-implant supported prostheses also are required.
CCM forms an oxidized layer, which provides anticorrosion properties. This is an important property to prevent direct contact of biological tissues to non-precious alloys. However, if tribocorrosion takes place at the interface of CCM alloy, it is harmful to the living body due to direct release of metal ion. Especially in orthopedics, studies regarding this issue report this phenomenon caused at metal-metal articular surface.29 Of course, when applied in dentistry, loading condition is very different, so it is hard to correlate this issue to the field of dentistry. The current study focused on only mechanical properties with potential applications for the field of prosthodontics. Therefore, further study is required to focus on biological properties at the abutment-implant interfaces of CCA and Gold UCLA abutments.
Figures and Tables
Fig. 2
A schematic diagram of connecting implant and prosthesis & loading position that is 3 mm away from the crown center.

Fig. 3
Typical graph of changes in the removal torque values with respect to elapsed time, which were measured every 0.1 sec by a driving torque tester.
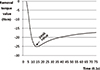
Fig. 4
Means and standard deviations of removal torque value of the CCM and Gold UCLA abutment groups.

Fig. 5
Representative SEM photograph at interface of abutment in the CCM group (original magnification: ×50).

Fig. 6
Representative SEM photograph at the interface of abutment in the Gold group (arrows : remarkable wear patterns, original magnification: ×50)

Fig. 7
Representative SEM photograph at the interface of fixture in the CCM group (original magnification : ×50).
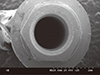
Fig. 8
Representative SEM photograph at the interface of fixture in the Gold group (original magnification : ×50).
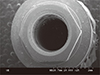
Table 1
Materials and manufacturer of implant components used in this study

Table 2
Test parameters of chewing simulation

References
1. Merickse-Stern R, Aerni D, Geering AH, Buser D. Long-term evaluation of non-submerged hollow cylinder implants. Clinical and radiographic results. Clin Oral Implants Res. 2001; 12:252–259.
2. Becker W, Becker BE, Alsuwyed A, Al-Mubarak S. Long-term evaluation of 282 implants in maxillary and mandibular molar positions: a prospective study. J Periodontol. 1999; 70:896–901.
3. Bahat O. Brånemark system implants in the posterior maxilla: clinical study of 660 implants followed for 5 to 12 years. Int J Oral Maxillofac Implants. 2000; 15:646–653.
4. Lewis SG, Llamas D, Avera S. The UCLA abutment: a four-year review. J Prosthet Dent. 1992; 67:509–515.
5. Baldassarri M, Hjerppe J, Romeo D, Fickl S, Thompson VP, Stappert CF. Marginal accuracy of three implant-ceramic abutment configurations. Int J Oral Maxillofac Implants. 2012; 27:537–543.
6. Leutert CR, Stawarczyk B, Truninger TC, Hämmerle CH, Sailer I. Bending moments and types of failure of zirconia and titanium abutments with internal implant-abutment connections: a laboratory study. Int J Oral Maxillofac Implants. 2012; 27:505–512.
7. Nothdurft FP, Doppler KE, Erdelt KJ, Knauber AW, Pospiech PR. Fracture behavior of straight or angulated zirconia implant abutments supporting anterior single crowns. Clin Oral Investig. 2011; 15:157–163.
8. Marti A. Cobalt-base alloys used in bone surgery. Injury. 2000; 31:18–21.
9. Breeding LC, Dixon DL, Nelson EW, Tietge JD. Torque required to loosen single-tooth implant abutment screws before and after simulated function. Int J Prosthodont. 1993; 6:435–439.
10. Dixon DL, Breeding LC, Sadler JP, McKay ML. Comparison of screw loosening, rotation, and deflection among three implant designs. J Prosthet Dent. 1995; 74:270–278.
11. Henry PJ, Laney WR, Jemt T, Harris D, Krogh PH, Polizzi G, Zarb GA, Herrmann I. Osseointegrated implants for single-tooth replacement: a prospective 5-year multicenter study. Int J Oral Maxillofac Implants. 1996; 11:450–455.
12. Becker W, Becker BE. Replacement of maxillary and mandibular molars with single endosseous implant restorations: a retrospective study. J Prosthet Dent. 1995; 74:51–55.
13. Patterson EA, Johns RB. Theoretical analysis of the fatigue life of fixture screws in osseointegrated dental implants. Int J Oral Maxillofac Implants. 1992; 7:26–33.
14. Goheen KL, Vermilyea SG, Vossoughi J, Agar JR. Torque generated by handheld screwdrivers and mechanical torquing devices for osseointegrated implants. Int J Oral Maxillofac Implants. 1994; 9:149–155.
15. Mitrani R, Nicholls JI, Phillips KM, Ma T. Accuracy of electronic implant torque controllers following time in clinical service. Int J Oral Maxillofac Implants. 2001; 16:394–399.
16. Gutierrez J, Nicholls JI, Libman WJ, Butson TJ. Accuracy of the implant torque wrench following time in clinical service. Int J Prosthodont. 1997; 10:562–567.
17. Haack JE, Sakaguchi RL, Sun T, Coffey JP. Elongation and preload stress in dental implant abutment screws. Int J Oral Maxillofac Implants. 1995; 10:529–536.
18. Koistinen A, Santavirta S, Lappalainen R. Apparatus to test insertion and removal torque of bone screws. Proc Inst Mech Eng H. 2003; 217:503–508.
19. Standlee JP, Caputo AA, Chwu MY, Sun TT. Accuracy of mechanical torque-limiting devices for implants. Int J Oral Maxillofac Implants. 2002; 17:220–224.
20. Yousef H, Luke A, Ricci J, Weiner S. Analysis of changes in implant screws subject to occlusal loading: a preliminary analysis. Implant Dent. 2005; 14:378–382.
21. Jaarda MJ, Razzoog ME, Gratton DG. Effect of preload torque on the ultimate tensile strength of implant prosthetic retaining screws. Implant Dent. 1994; 3:17–21.
22. Jörnéus L, Jemt T, Carlsson L. Loads and designs of screw joints for single crowns supported by osseointegrated implants. Int J Oral Maxillofac Implants. 1992; 7:353–359.
23. Theoharidou A, Petridis HP, Tzannas K, Garefis P. Abutment screw loosening in single-implant restorations: a systematic review. Int J Oral Maxillofac Implants. 2008; 23:681–690.
24. Truninger TC, Stawarczyk B, Leutert CR, Sailer TR, Hämmerle CH, Sailer I. Bending moments of zirconia and titanium abutments with internal and external implant-abutment connections after aging and chewing simulation. Clin Oral Implants Res. 2012; 23:12–18.
25. Bates JF, Stafford GD, Harrison A. Masticatory function - a review of the literature. III. Masticatory performance and efficiency. J Oral Rehabil. 1976; 3:57–67.
26. Richter EJ. In vivo vertical forces on implants. Int J Oral Maxillofac Implants. 1995; 10:99–108.
27. Merz BR, Hunenbart S, Belser UC. Mechanics of the implant-abutment connection: an 8-degree taper compared to a butt joint connection. Int J Oral Maxillofac Implants. 2000; 15:519–526.
28. Schwarz MS. Mechanical complications of dental implants. Clin Oral Implants Res. 2000; 11:156–158.
29. Delaunay C, Petit I, Learmonth ID, Oger P, Vendittoli PA. Metal-on-metal bearings total hip arthroplasty: the cobalt and chromium ions release concern. Orthop Traumatol Surg Res. 2010; 96:894–904.




 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download