Abstract
PURPOSE
The aim of this study was to assess the esthetic outcome of maxillary anterior single implants by comparing the esthetic perception of dental professionals and patients.
MATERIALS AND METHODS
Twenty-three patients with single implants in the esthetic zone were enrolled in this study. Dentists of four different dental specialties (Three orthodontists, three oral surgeons, three prosthodontists, and three periodontists) evaluated the pink esthetic score (PES)/white esthetic score (WES) for 23 implant-supported single restorations. The satisfactions of the patients on the esthetic outcome of the treatment have been evaluated according to the visual analog scale (VAS).
RESULTS
The mean total PES/WES was 12.26 ± 4.76. The mean PES was 6.45 ± 2.78 and mean WES was 5.80 ± 2.82. There was a statistically significant difference among the different specialties for WES (P<.01) and Total PES/WES (P<.01). Prosthodontists were found to have assigned poorer ratings among the other specialties, while oral surgeons gave the higher ratings than periodontists, orthodontists, and prosthodontists.
CONCLUSION
Prosthodontists seemed to be stricter when assessing aesthetic outcome among other specialties. Moreover, a clear correlation existed between dentists' and patients' esthetic perception, thereby providing rationales for involving patients in the treatment plan to achieve higher levels of patient satisfaction.
The outcome of dental implant treatment is frequently described using success criteria from clinical and radiologic aspects generally based on the defined thresholds of objective clinical parameters of peri-implant lesions.12 These parameters can be characterized by pocket probing depth (PD), modified bleeding index (MBI), modified plaque index (MPI), and radiographic observations.3 Recently, additional criteria, such as the health status, appearance of the peri-implant soft tissues, prosthodontic parameters, and patient satisfaction, have been suggested in evaluation of the success of implant treatment.4
The success of a single implant restoration in the esthetic zone depends mainly on the harmonious integration of the restoration into the patient's overall appearance, especially the peri-implant soft tissue.56 Both subjective (patients' ratings) as well as objective (esthetic scores and indices) assessment of implant esthetics are subject to growing interests,789101112 although there is no universally accepted evaluation criterion yet.
The Visual Analogue Scale (VAS) was recommended as a subjective measure of the esthetic outcome of implant-supported restorations.13 Other means to assess the esthetic outcome of single implant-supported restorations are various indices, such as implant aesthetic crown index (ICA), subjective esthetic score (SES), peri-implant and crown index (PICI), and comprehensive index comprising pink and white esthetic score (PES/WES).14151617
A challenge in assessing esthetics comes from the facts that the judgment of esthetics is subjective and that esthetic norms vary between cultures and groups. Furthermore, examiners' specialties have been shown to affect esthetic evaluation on natural teeth.18
Fürhauser et al. introduced an excellent index termed pink esthetic score (PES) for evaluation of the soft tissue around single-implant crowns that might change over time; PES could be a useful tool for monitoring long-term soft-tissue alterations.15 Reproducibility of PES and the effects of the observer's specialization were investigated in another study by recruiting general practitioners, oral surgeons, orthodontics, students in master's degree for implants, and lay persons.19
Belser et al.16 have later introduced pink esthetic score (PES) to evaluate the esthetic outcome of soft tissue around implant-supported single crowns in the anterior zone and white esthetic score (WES) to specifically focus on the visible part of the implant restoration itself. The effects of the observer's specialization were further investigated in the study by Cho et al.20 using PES/WES index, which was the only study to recruit periodontists. However, the study had limitations due to the small number of the examiners from each specialty group and no oral surgeons involved in the study.
Meijer et al.14 proposed the Implant Crown Aesthetic Index (ICAI) for evaluation of single-implant supported crowns. The limitations of the study by Meijer et al. were the small sample size and recruitment of only two specialties (oral surgeons and prosthodontics).
According to a recent study comparing the indices and their reproducibility, PES/WES and PICI seemed to be more suitable than ICAI as esthetic indices for single implant-supported crowns.17
The purpose of this study was to evaluate single implant-supported crowns in the anterior maxilla and compare objective ratings of four dental specialties with patients' evaluation.
The records from the Implant Clinic in College of Dentistry (King Saud University, Saudi Arabia) were specifically screened for patients provided with single-tooth implants located in the anterior maxilla (upper incisors, canines, and first premolars). Twenty-three patients with metal-ceramic screw-retained single-tooth implants were randomly selected and scheduled for following-up examinations between 2008 and 2014. Patient age ranged between 20 and 65 years (median: 41 years) at the time of implant surgery, and the follow-up period was 16 - 72 months (median: 32 months).
Inclusion criteria for all subjects were: 1) presence of a single implant tooth in the anterior maxilla and 2) good/fair oral hygiene. Patients were excluded if presenting one or more of the following criteria: 1) multiple implants; 2) active periodontal disease; 3) infection around the implant; 4) resorption of alveolar bone more than 2 mm; or 5) absence of crown on the contra-lateral tooth. This study was approved by the local medical ethics committee of College of Dentistry, King Saud University. The patients agreed to participate and signed an informed consent.
The clinical photographs (Fig. 1) were used primarily to assess general tooth/crown form, tooth/crown color, incisal translucency, characterization, as well as soft tissue color, curvature, and level. The photographs were taken by the same person using a Nikon D5000 digital camera (Nikon, Inc., Melville, NY, USA) and a 90 mm lens (AF-S VR Micro-Nikkor 90 mm f/2.8G IF-ED, Nikon, Melville, NY, USA) with a ring flash (EM-140 DG, SIGMA, Ronkonkoma, NY, USA), and the photographer ensured that the Frankfort horizontal plane of the patient was parallel to the ground. Photos of the implant crown and the peri-implant soft tissues, including at least one adjacent tooth on each side, were taken using two projections: one facial projection perpendicular to the facial implant crown and another incisal/occlusal projection. In addition, a photo of the reference teeth, the incisor and canine on the contralateral side, was taken.
The clinical examination involved the mean modified plaque index (mPI),21 modified sulcus bleeding index (mSBI),22 and probing depth (PD) at four aspects around each implant as indicators for bone resorption and inflammation.3 Periapical radiographs (Fig. 2) were taken for each implant using long cone technique with XCP, with the aim to evaluate the presence/absence of continuous peri-implant radiolucency and to measure the distance between the implant shoulder and the first visible bone-to-implant contact (DIB) in mm, at the mesial and distal site of each implant.23 A mean DIB value was obtained from the mesial and distal measurement at each radiograph.
A total of 12 examiners from different dental specialties were involved: three orthodontists, three oral surgeons, three prosthodontists, and three periodontists. The examiners were randomly selected from the faculty members of the College of Dentistry, King Saud University. The selected specialists were not involved in the treatment of the patients.
The examiners had a calibration session prior to the beginning of the evaluation. They were briefed on the study objectives and invited separately to the examination room, and were handed the questionnaires to assess the PES and WES. In the current study, the PES/WES index was used according to Belser et al.16 to evaluate the esthetic outcome. All variables were evaluated in comparison to the contralateral tooth.
PES was measured using the modified peri-implant soft tissue score (PES) as described by Belser et al.16 This was a modified version of the original PES scale invented by Fürhauser et al.15 The PES index involved the following five variables: mesial papilla, distal papilla, the level and curvature of the facial mucosa, root convexity, and soft-tissue color and texture at the facial side of the implant. For mesial and distal papilla, a score of 2 (Complete), 1 (Incomplete), and 0 (Absent) were assigned. For the remaining three PES parameters, a score of 2 (no discrepancy), 1 (minor discrepancy), and 0 (major discrepancy) were assigned. The highest possible score would be 10 and the threshold of clinical acceptability was set at 6.24
WES was based on the five following parameters: general tooth form, outline and volume of the clinical crown, color including the assessment of hue and value, surface texture, translucency, and characterization. A score of 2 was given if there was no discrepancy; score 1 for minor discrepancies; and score 0 for any major discrepancy observed. A maximum total WES was 10 and the threshold of clinical acceptance was set at a score of 6.24
These indices represented a close match of the peri-implant soft tissue conditions and the clinical single tooth implant crown compared to the respective features of the contra lateral natural tooth. The highest possible combined PES/WES score was 20.
A subjective patient satisfaction with implant esthetics was evaluated using Visual analogue scale (VAS). A VAS is a measurement instrument by using questionnaires for characteristics that are believed to range across a continuum of values and that cannot easily be directly measured. VAS has been applied for the patients' subjective esthetic evaluation.24
Thirteen questions (Table 1) were used to determine the patients' satisfaction to the overall implant restoration treatment. The answer for the questions was marked on a vertical line along a 100-mm long horizontal line. The distance from the start (left) to the marked line was measured in millimeter (VAS score in mm) and classified as: not satisfied (0 - 20 mm), partly satisfied (20 - 40 mm), acceptably satisfied (40 - 60 mm), satisfied (60 - 80 mm), and completely satisfied (80 - 100 mm).25
The data were analyzed with Statistical Package for Social Sciences for Windows 17.0 (SPSS Inc., Chicago, IL, USA). The differences for PES, WES, and total PES/WES among the specialty groups were assessed with the Kruskal Wallis analysis. Spearman correlation test was carried out to evaluate the relationship between VAS and total PES/WES. P values were calculated for establishing the associations and a statistical significance level of 5% was adopted.
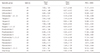
Clinical examination of the patients revealed a good oral hygiene, reflected by the mean modified plaque index (mPI) of 98.1 ± 5.81. The peri-implant soft tissues appeared healthy, which corresponded well with the low mean mSBI of 14.13 ± 18.2. The mean PD lingual was 3.22 ± 0.79 mm, buccal 2.61 ± 1 mm, distal 3.04 ± .9 mm, and mesial 2.87 ± 1.06 mm (Table 2).
The radiographic analysis of 23 implants demonstrated minimal crestal bone loss contained within the height of the collar, and no bone loss was evident to the level of the implant threads, with a mean DIB of 2.14 mm ± 1.23 (Table 2). All bone loss was contained within the height of the collar, and no bone loss was evident to the level of the implant threads.
The summarized mean of PES/WES values with their standard deviations of the single-tooth implants are presented in Table 3. The PES/WES values had a wide range from 7.4 to 16.4 with a mean score of 12.34. The PES was clearly higher than the corresponding WES. The mean PES (6.45 ± 2.38) scored above the threshold of 6. On the other hand, the mean WES (5.80 ± 2.39) scored below the threshold of 6. The two PES parameters of mesial papilla (1.50 ± 0.67) and distal papilla (1.42 ± 0.65) had the highest mean values, whereas the level of facial mucosa (1.15 ± 0.65) showed the least mean PES value. For the WES, the scores for tooth form and tooth volume/outline (mean scores of 1.07 ± .69 and 1.08 ± .69, respectively) showed the lowest mean scores of all five parameters, while the highest score was for the surface texture (1.32 ± .67). The mean total PES of the 23 single tooth implants scored < 6.
The mean total PES/WES was 13.10 ± 3.24 for the periodontists, 11.13 ± 3.97 for the prosthodontists, 11.39 ± 4.09 for the orthodontists, and 13.71 ± 4.55 for the oral surgeons (Table 4). There was a statistically significant difference among the different specialties for WES (P < .01) and total PES/WES (P < .01) according to the Kruskal Wallis analysis (Table 5). Prosthodontists were found to have assigned poorer ratings than the other groups. Oral surgeons gave the relatively higher ratings than prosthodontists, orthodontists, and periodontists.
For the soft tissue esthetics in PES, periodontists yielded the highest mean (7.07), while prosthodontists had the lowest mean (5.97) score. Periodontists had the lowest standard of deviations (1.9), while oral surgeons had the highest standard deviations (2.93).
Regarding the implant crown esthetics evaluation, oral surgeons had the highest mean score for the WES (6.84), while prosthodontists and orthodontics had the lowest mean WES (5.16) score. Periodontists had the lowest standard of deviations (1.95), while orthodontics had the highest standard deviations (2.94).
The result of the questionnaire for determining the patient satisfaction was presented in Figure 3. About 70% of the participants reported complete satisfaction with the shape of the crown. None of the respondents were unsatisfied with their treatment. About 65% of the participants reported 'completely satisfied' with the color of their crowns, and less than 5% reported 'not satisfied'. The third question addressed the symmetry of the restoration; for this, 43% of the participants reported 'completely satisfied', 35% said 'satisfied', 13% answered 'acceptably satisfied', and 9% answered 'partly satisfied'. The fourth question dealt with the alignment of the restoration with the other teeth; for this, 65% of the participants reported 'completely satisfied' and 18% reported 'partly satisfied'. The fifth statement was about the patients' satisfaction with their smile. About 56% of the participants said they were 'completely satisfied' and about 9% said they were 'not satisfied' with their smile. The next statement assessed the patient's satisfaction with the shape of their gums, for which 61% of the participants said they were 'completely satisfied'. The seventh statement was regarding their satisfaction with the gum color. About 61% of the participants reported 'completely satisfied' and 13% reported 'not satisfied'. The next statement assessed the function of the restoration during eating, for which 57% of the participants reported 'completely satisfied'. The next question assessed the patient's satisfaction with the restoration during speech, for which 76% of the participants reported 'completely satisfied'. The tenth statement assessed the patient's satisfaction with the ease of care of the restoration. About 65% of the participants reported 'completely satisfied', 22% 'acceptably satisfied', 9% 'satisfied', and about 4% 'not satisfied'. The next statement was 'did your treatment meet your expectations?', for which 76% of the participants said they were 'completely satisfied'. The 12th question assessed their satisfaction with the time taken to finish the treatment, for which about 41% said they were 'completely satisfied'. The next statement enquired their satisfaction with the cost of treatment. For this, 48% answered 'completely satisfied', 13% 'satisfied', 22% 'acceptably satisfied', 9% 'partially satisfied', and 8% 'not satisfied'.
Nowadays, with recent advances in technology and in treatment protocols and increased demands of our population to aesthetic dentistry, the focus has shifted towards esthetic demands of oral implants in a visible anterior region. Predictable functions with esthetic results are key elements for successful oral implant therapy.
The effects of an examiner's subjective opinions and dental specialties were considered to affect the perception of the esthetic assessment. This study presented the esthetic outcomes of 23 anterior maxillary single tooth implants; they were objectively assessed using a comprehensive PES/WES index according to Belser et al.16
The peri-implant crestal bone level is a criterion for implant success. The preservation of the height of the peri-implant bone crest is crucial for the papilla height and the embrasure space, which has implications for esthetics.26
All the 23 anterior maxillary single-tooth implants were clinically successful according to strict criteria defined by Buser et al.27 regarding the absence of peri-implant radiolucency, implant mobility, suppuration, and pain. The radiographic analysis showed no bone loss was evident to the level of the implant threads.
The position and inclination of implants are important in achieving the optimal esthetic outcome. The implant restoration should be symmetrical with the contra-lateral tooth, and the ideal implant restoration should imitate the appearance of the natural teeth.8 In the present study, the contra-lateral natural tooth was used as a reference for single implant treatment in the anterior maxilla. This method has been found to be effective in other studies.10
About 75% of the patients in this study stated that the treatment met their expectations. In the study by Pjetursson and Lang28 more than 90% reported complete satisfaction with their treatment. This may be due to the difference in the patient population studied, history of previous unpleasant experiences with dental treatments, an inadequacy of pre-implant prosthetic status, and patients' personal motives. This emphasizes that patients' expectations should be assessed by the dental professionals in an attempt to predict how patients will evaluate the esthetics after treatment. The majority of the patients were satisfied with their post-treatment phonetics, which was comparable with the findings of another study with a similar population.29 About half the patients were satisfied with the cost of treatment, which is similar to other studies.30
In this study, the papillae showed the highest score of all soft tissue criteria and were complete papilla fill was achieved in about 60% of all cases. This is in line with findings of Lai et al. reporting 6-month data on conventional single implant treatment.31 However, a retrospective study by Belser et al. on early implant treatment with a similar follow-up as the present study only showed 30% of the cases were complete distal papilla fill was achieved.16 A common problem associated with the surrounding soft tissue is gingival hyperplasia and inflammation around implants.32 Specific indices were used to assess the size and shape of the peri-implant soft tissue.141533 The papilla index was used to assess the size and volume of inter-proximal papillae adjacent to single-tooth implants.33 In another study, the aesthetic implant crown index was used, and this index was related to the implant restoration itself and the surrounding soft tissues.14 The results of the present study showed that the mesial and distal papilla scores were slightly less favorable (1.5 and 1.4, respectively) in comparison with other studies.1620 It is difficult to compare the papilla level between the studies because each study followed a different surgical protocol.
The level of facial mucosa in this study had the lowest PES parameter (1.15). Cosyn et al. in their study showed excellent outcome in about half of their cases.10 This might be due to the difference in the soft tissue type and the technique of implant placement. PES/WES is useful in evaluating the esthetic outcome of the single implant restoration in clinical practice. Belser et al. evaluated the esthetic outcome of maxillary anterior single tooth implants using WES/PES, and they used the VAS to evaluate the satisfaction of the patient toward the single implant in the esthetic zone.16 It has been reported that the use of oral photographs in the assessment of single-tooth peri-implant soft tissue permitted accurate and objective measurements.3435 In this study, we have reported a strong correlation between the esthetic evaluation performed by the dentist (PES/WES) and by the patient (VAS), which was comparable with the results of the study performed by Cho et al.20 Cho et al. compared patient's perception on aesthetic appearance with the perception of five trained prosthodontists and concluded that professionals might be much more critical towards the aesthetic outcome than the patients. This result was in contradiction to other studies, in which no correlation was observed.16
Previous studies tried to identify the effect of dental specialization on assessment of implant esthetics using different indices by comparing their intra-observer agreement.
The results of these studies were contradictory. For intra-observer agreement, in the study with two different specialties performed by Meijer et al., the results showed that prosthodontics were more reproducible than oral surgeons with ICAI, while the best agreement was found with oral surgeons using the same index.19 Gehrke et al. found that orthodontics were most reliable with PES/WES,36 and this was same with the other PES study.20
The results of this study demonstrated the influence of four dental specialties on their perception of esthetics. The prosthodontists gave the lowest ratings and the surgeons gave the highest rating with PES/WES. These results were different from the study by Cho et al.,20 in which prosthodontists gave poorer ratings than other groups and orthodontists were clearly more critical than the other groups. However, in the study by Cho et al., the difference between these groups was not statistically different except that for WES.
The rating arrangement of this study could be presented as following: Oral Surgeons > Periodontists > Orthodontists > Prosthodontists.
The oral surgeons, therefore, appeared to be more generous in their assessment of esthetics of implant-supported crowns. On the other hand, prosthodontists were trained to improve the aesthetics for a natural looking smile.
In addition, the use of VAS to achieve patient-centered outcome is still a matter of discussion.28 However, it has many advantages like simplicity of the statistical analysis, the elimination of language barriers, and the possibility of comparison of the results with those of other studies.
The limitation of the current study was the small sample size, which might limit the generalizability of the study results. With respect to the limitations of the study design, we wish to emphasize that this was not a randomized controlled trial, making any comparison possibly biased. Future studies of different populations and larger samples are indicated to elaborate on the current study findings.
The present study demonstrates the influence of observer specialization on PES/WES ratings. Prosthodontists are shown to be more critical when assessing aesthetic outcome among dental specialties, whereas oral surgeons are less critical. Moreover, a clear correlation between dentists' and patients' esthetic perception, thereby providing rationales for involving patients in the treatment plan to achieve higher levels of patient satisfaction.
Figures and Tables
 | Fig. 1Clinical photograph of implant-supported single-tooth restoration at the region of the left central incisor. |
 | Fig. 2Radiographic evaluation for implant-supported single-tooth restoration at the left central incisor location. |
 | Fig. 4Correlation between the total pink esthetic score (PES)/white esthetic score (WES) and the visual analog scale (VAS). |
Table 1
Patient satisfaction questionnaire

Table 2
Clinical peri-implant parameters of the 23 implants

| Valid | Minimum | Maximum | Mean | SD | |
|---|---|---|---|---|---|
| DIB mm | 23 | 0 | 5 | 2.14 | 1.23 |
| Msbi | 23 | 0 | 100 | 14.13 | 18.2 |
| mPI (%) | 20 | 0 | 100 | 98.1 | 5.81 |
| PD (L) | 23 | 2 | 5 | 3.21 | 0.8 |
| PD (B) | 23 | 1 | 5 | 2.6 | 1 |
| PD (D) | 23 | 1 | 5 | 3.04 | 0.9 |
| PD (M) | 23 | 1 | 5 | 2.9 | 1.06 |
Table 3
Summarized the PES and WES of the 23 implants

Table 4
Specialty-wise distribution of the observations
References
1. Albrektsson T, Brånemark PI, Hansson HA, Lindström J. Osseointegrated titanium implants. Requirements for ensuring a long-lasting, direct bone-to-implant anchorage in man. Acta Orthop Scand. 1981; 52:155–170.
2. Stellingsma K, Bouma J, Stegenga B, Meijer HJ, Raghoebar GM. Satisfaction and psychosocial aspects of patients with an extremely resorbed mandible treated with implant-retained overdentures. A prospective, comparative study. Clin Oral Implants Res. 2003; 14:166–172.
3. Mombelli A, Lang NP. The diagnosis and treatment of peri-implantitis. Periodontol 2000. 1998; 17:63–76.
4. Papaspyridakos P, Chen CJ, Singh M, Weber HP, Gallucci GO. Success criteria in implant dentistry: a systematic review. J Dent Res. 2012; 91:242–248.
5. Cosyn J, Eghbali A, De Bruyn H, Dierens M, De Rouck T. Single implant treatment in healing versus healed sites of the anterior maxilla: an aesthetic evaluation. Clin Implant Dent Relat Res. 2012; 14:517–526.
6. Hof M, Pommer B, Strbac GD, Sütö D, Watzek G, Zechner W. Esthetic evaluation of single-tooth implants in the anterior maxilla following autologous bone augmentation. Clin Oral Implants Res. 2013; 24:88–93.
7. Buser D, Martin W, Belser UC. Optimizing esthetics for implant restorations in the anterior maxilla: anatomic and surgical considerations. Int J Oral Maxillofac Implants. 2004; 19:43–61.
8. Luo Z, Zeng R, Luo Z, Chen Z. Single implants in the esthetic zone: analysis of recent peri-implant soft tissue alterations and patient satisfaction. A photographic study. Int J Oral Maxillofac Implants. 2011; 26:578–586.
9. Baracat LF, Teixeira AM, dos Santos MB, da Cunha Vde P, Marchini L. Patients' expectations before and evaluation after dental implant therapy. Clin Implant Dent Relat Res. 2011; 13:141–145.
10. Cosyn J, Eghbali A, De Bruyn H, Dierens M, De Rouck T. Single implant treatment in healing versus healed sites of the anterior maxilla: an aesthetic evaluation. Clin Implant Dent Relat Res. 2012; 14:517–526.
11. Hartlev J, Kohberg P, Ahlmann S, Andersen NT, Schou S, Isidor F. Patient satisfaction and esthetic outcome after immediate placement and provisionalization of single-tooth implants involving a definitive individual abutment. Clin Oral Implants Res. 2014; 25:1245–1250.
12. Traini T, Pettinicchio M, Murmura G, Varvara G, Di Lullo N, Sinjari B, Caputi S. Esthetic outcome of an immediately placed maxillary anterior single-tooth implant restored with a custom-made zirconia-ceramic abutment and crown: a staged treatment. Quintessence Int. 2011; 42:103–108.
13. Belser U, Buser D, Higginbottom F. Consensus statements and recommended clinical procedures regarding esthetics in implant dentistry. Int J Oral Maxillofac Implants. 2004; 19:73–74.
14. Meijer HJ, Stellingsma K, Meijndert L, Raghoebar GM. A new index for rating aesthetics of implant-supported single crowns and adjacent soft tissues-the Implant Crown Aesthetic Index. Clin Oral Implants Res. 2005; 16:645–649.
15. Fürhauser R, Florescu D, Benesch T, Haas R, Mailath G, Watzek G. Evaluation of soft tissue around single-tooth implant crowns: the pink esthetic score. Clin Oral Implants Res. 2005; 16:639–644.
16. Belser UC, Grütter L, Vailati F, Bornstein MM, Weber HP, Buser D. Outcome evaluation of early placed maxillary anterior single-tooth implants using objective esthetic criteria: a cross-sectional, retrospective study in 45 patients with a 2- to 4-year follow-up using pink and white esthetic scores. J Periodontol. 2009; 80:140–151.
17. Tettamanti S, Millen C, Gavric J, Buser D, Belser UC, Brägger U, Wittneben JG. Esthetic evaluation of implant crowns and peri-implant soft tissue in the anterior maxilla: Comparison and reproducibility of three different indices. Clin Implant Dent Relat Res. 2016; 18:517–526.
18. Kokich VO Jr, Kiyak HA, Shapiro PA. Comparing the perception of dentists and lay people to altered dental esthetics. J Esthet Dent. 1999; 11:311–324.
19. Gehrke P, Degidi M, Lulay-Saad Z, Dhom G. Reproducibility of the implant crown aesthetic index-rating aesthetics of single-implant crowns and adjacent soft tissues with regard to observer dental specialization. Clin Implant Dent Relat Res. 2009; 11:201–213.
20. Cho HL, Lee JK, Um HS, Chang BS. Esthetic evaluation of maxillary single-tooth implants in the esthetic zone. J Periodontal Implant Sci. 2010; 40:188–193.
21. Andersson B, Bergenblock S, Fürst B, Jemt T. Long-term function of single-implant restorations: a 17- to 19-year follow-up study on implant infraposition related to the shape of the face and patients' satisfaction. Clin Implant Dent Relat Res. 2013; 15:471–480.
22. Buser D, Bornstein MM, Weber HP, Grütter L, Schmid B, Belser UC. Early implant placement with simultaneous guided bone regeneration following single-tooth extraction in the esthetic zone: a cross-sectional, retrospective study in 45 subjects with a 2- to 4-year follow-up. J Periodontol. 2008; 79:1773–1781.
23. Weber HP, Buser D, Fiorellini JP, Williams RC. Radiographic evaluation of crestal bone levels adjacent to nonsubmerged titanium implants. Clin Oral Implants Res. 1992; 3:181–188.
24. Lavigne SE, Krust-Bray KS, Williams KB, Killoy WJ, Theisen F. Effects of subgingival irrigation with chlorhexidine on the periodontal status of patients with HA-coated integral dental implants. Int J Oral Maxillofac Implants. 1994; 9:156–162.
25. Wolfart S, Thormann H, Freitag S, Kern M. Assessment of dental appearance following changes in incisor proportions. Eur J Oral Sci. 2005; 113:159–165.
26. Mombelli A, Lang NP. Clinical parameters for the evaluation of dental implants. Periodontol 2000. 1994; 4:81–86.
27. den Hartog L, Slater JJ, Vissink A, Meijer HJ, Raghoebar GM. Treatment outcome of immediate, early and conventional single-tooth implants in the aesthetic zone: a systematic review to survival, bone level, soft-tissue, aesthetics and patient satisfaction. J Clin Periodontol. 2008; 35:1073–1086.
28. Pjetursson BE, Lang NP. Prosthetic treatment planning on the basis of scientific evidence. J Oral Rehabil. 2008; 35:72–79.
29. Hartog L, Meijer HJ, Santing HJ, Vissink A, Raghoebar GM. Patient satisfaction with single-tooth implant therapy in the esthetic zone. Int J Prosthodont. 2014; 27:226–228.
30. Palmqvist S, Soderfeldt B, Arnbjerg D. Subjective need for implant dentistry in a Swedish population aged 45-69 years. Clin Oral Implants Res. 1991; 2:99–102.
31. Lai HC, Zhang ZY, Wang F, Zhuang LF, Liu X, Pu YP. Evaluation of soft-tissue alteration around implant-supported single-tooth restoration in the anterior maxilla: the pink esthetic score. Clin Oral Implants Res. 2008; 19:560–564.
32. Adell R, Lekholm U, Rockler B, Brånemark PI. A 15-year study of osseointegrated implants in the treatment of the edentulous jaw. Int J Oral Surg. 1981; 10:387–416.
33. Jemt T. Regeneration of gingival papillae after single-implant treatment. Int J Periodontics Restorative Dent. 1997; 17:326–333.
34. Chang M, Wennström JL, Odman P, Andersson B. Implant supported single-tooth replacements compared to contralateral natural teeth. Crown and soft tissue dimensions. Clin Oral Implants Res. 1999; 10:185–194.
35. Priest G. Predictability of soft tissue form around single tooth implant restorations. Int J Periodontics Restorative Dent. 2003; 23:19–27.
36. Gehrke P, Lobert M, Dhom G. Reproducibility of the pink esthetic score-rating soft tissue esthetics around single-implant restorations with regard to dental observer specialization. J Esthet Restor Dent. 2008; 20:375–384.




 PDF
PDF ePub
ePub Citation
Citation Print
Print






 XML Download
XML Download