Abstract
PURPOSE
The aim of this study was to evaluate the clinical findings and patient satisfaction on implant overdenture designed with Locator implant attachment or Locator bar attachment in mandibular edentulous patients.
MATERIALS AND METHODS
Implant survival rate, marginal bone loss, probing depth, peri-implant inflammation, bleeding, plaque, calculus, complications, and satisfaction were evaluated on sixteen patients who were treated with mandibular overdenture and have used it for at least 1 year (Locator implant attachment: n=8, Locator bar attachment: n=8).
RESULTS
Marginal bone loss, probing depth, plaque index of the Locator bar attachment group were significantly lower than the Locator implant attachment group (P<.05). There was no significant difference on bleeding, peri-implant inflammation, and patient satisfaction between the two denture types (P>.05). The replacement of the attachment components was the most common complication in both groups. Although there was no correlation between marginal bone loss and plaque index, a significant correlation was found between marginal bone loss and probing depth.
Implant overdentures increase the masticatory function and improve satisfaction by making up for insufficient retention and stability of a conventional dentures.12 Awad et al.3 reported high satisfaction, denture stability, and masticatory function of implant overdentures in a comparative study with conventional dentures. Meanwhile, Batenburg et al.4 reported a high implant success rate in implant overdentures through a literature review. Based on such a high success rate of the implant overdentures in edentulous patients, implant overdentures have become one of the most widely recommended treatments in mandibular edentulous patients since McGill consensus5 in 2002.
As implant overdentures have been widely used clinically and understanding about implant overdentures have become higher, the type of implant attachment and application methods have been diversely developed.6 The attachment for implant overdentures can be divided into the solitary type and bar type depending on whether it is connected to the implant or not.7 Solitary type attachments, such as ball attachment, magnet attachment, and the Locator, have advantages such as the simplicity of the oral hygiene maintenance and possibility of using in a narrow interarch space. On the other hand, a parallel implant placement is required, and the stability of the implant overdentures is inferior to that of bar type.8 Bar type attachment, such as the Hader bar, Dolder bar, and milled bar, can evenly disperse loading imposed at mastication, and the placement inclination is less limited. However, the fabrication process is complex and approximately 17 mm of interocclusal inclination is required, including approximately 2 mm of minimum space from the gingiva.9
Among the various attachments, the Locators are widely used due to its several advantages: the height is low, self-alignment is possible, reduction of retention is small due to its dual retention, and the replacement of components is easy.10 The type of Locator used in an implant includes the Locator implant attachment that is directly connected to the implant placed in a solitary type, and the Locator bar attachment that is used with a bar. The Locator bar attachment is an attachment used for the improvement of retention and stability usually after more than four implants have been placed and connected with a bar. According to the method of fixing metal female to a bar, it is classified into gold bar casting, laser welding, or drill and tapping.11 Among these, drill and tapping is a method in which a plastic thread is inserted in the place where a metal female is fixed in the wax bar status. After casting, a thread is secured by using a bar tap, and then a screw-in female is connected.12 If a bar is fabricated by using a computer aided design/computer aided manufacturing (CAD/CAM) system, then thread formation would be easy. The greatest advantage of the drill and tapping method is that it is easy to replace the metal female only without re-fabricating a bar at loss of retention due to abrasion of the metal female.11
Implant overdentures using the Locator show a high implant success rate of over 94.5%. In addition, it requires low maintenance as compared to the other solitary type attachments due to its average life of 22.6 months.1314 According to the study of Mackie et al.,15 as a result of comparing the replacement frequency of the Locator patrix and ball attachment matrix in implant overdentures by using two implants, there was no significant difference. However, the replacement frequency of the Locator patrix tended to be lower than that of the ball attachment. In a 5-year clinical study of Akça et al.,16 the Locator showed less bone resorption and higher plaque and bleeding indices than that of the ball attachment. On the other hand, Krennmair et al.17 reported that the satisfaction with the implant overdentures by using the Locator was higher than that of the conventional dentures. Many studies have been done regarding the Locator applied to implant overdentures,131415 but there are only a few comparative studies on the complications or survival rate of the implant overdentures by using a solitary type Locator implant attachment and a bar type Locator bar attachment.
Therefore, this study intended to conduct a retrospective evaluation with a medical chart and clinical examination by selecting implant overdentures cases via the Locator implant attachment or Locator bar attachment among mandibular implant overdentures produced by the Department of Prosthodontics at the Pusan National University Dental Hospital.
Study subjects: For this study, mandibular implant overdentures were produced at Pusan National University Dental Hospital for 6 years from 2008 to 2014. Among the patients who were wearing removable denture on the maxilla, those who had experienced occlusal force for at least one year after implant overdenture placement and had received regular maintenance were included in this study.
Among these patients, those who had systemic diseases that might affect implant overdenture treatment, such as immune disease, chemotherapy, hemorrhagic disease, uncontrolled diabetes, and hormonal imbalance, and alcohol or substance abuse, as well as those who did not receive regular postoperative oral examination, were excluded from the analysis.
The study was conducted on 16 patients (5 males; 11 females), who fulfilled the inclusion criteria under the review of Pusan National University Dental Hospital Institutional Review Board IRB No. PNUDH- 2015-016) (Table 1).
Implant overdentures: A total of 16 patients were divided into two groups depending on the type of Locator attachment used in the mandibular implant overdenture production, namely, LIA group (n = 8) using two implants with a Locator implant attachment (Zest Anchors Inc., Escondido, CA, USA), and LBA group (n = 8) using four implants with a Locator bar attachment to a bar (Zest Anchors Inc., Escondido, CA, USA) (Fig. 1).
Clinical examination: The following items were evaluated through clinical examinations and radiographs from the date of the final implant overdenture placement to the final hospital visit.
Implant survival rate: Based on the criteria mentioned by Cochran et al.,18 the survival rate of the implant was evaluated. The criteria are as follows: 1) absence of persistent discomfort, such as pain, foreign body sensation, and dysesthesia, among others, 2) absence of persistent peri-implant infection symptoms, such as suppuration, and absence of recurrence, 3) absence of clinical implant mobility, and 4) absence of radiolucency around the implant, and absence of rapidly progressive bone loss.
Implant marginal bone resorption and probing depth: Radiographs were taken via parallel technique using a portable X-ray (Port II, Genoray Co., Sungnam, Korea). After measuring implant major diameter and marginal bone level (the distance from the implant platform to the uppermost part of the marginal bone) using i-Solution (Olympus B × 51; Olympus Inc., Tokyo, Japan), marginal bone resorption of the implant was calculated and compared to the actual major diameter of the implant.19
Probing depth: For the Merritt-B periodontal probe, after measuring the peri-implant mesiodistal and labiolingual sides from a position parallel to the longest axis of the implant, the average was calculated.20
Peri-implant inflammation: Based on the Lőe and Silness index,21 a score from 0 to 3 was given according to the peri-implant inflammation status: 1) score 0: Absence of inflammation, 2) score 1: Mild inflammation, 3) score 2: Moderate inflammation, and 4) score 3: Severe inflammation.
Bleeding Index: Based on the criteria suggested by Mombelli et al.,22 using Merritt-B periodontal probe, the level of bleeding was measured with a score from 0 to 3: 1) score 0: No bleeding, 2) score 1: Isolated bleeding spots visible, 3) score 2: Blood forms a confluent red line on the margin, and 4) score 3: Heavy or profuse bleeding.
Plaque Index: According to the criteria of Mombelli et al.,22 after measuring the plaque attached to the surface of the implant, a score from 0 to 3 was given: 1) score 0: No detection of plaque, 2) score 1: Plaque only recognized by running a probe across the smooth marginal surface of the implant, 3) score 2: Plaque can be seen by the naked eye, and 4) score 3: Abundance of soft matter.
Calculus: Based on the presence of calculus, a score 0 or 1 was given: 1) score 0: Absence of calculus, and 2) score 1: Presence of calculus.
Complication: Following the prosthesis placement, the total treatment frequency was examined after classifying the complications into denture-related issues (resin base fracture, artificial tooth fracture, frame work fracture, new prosthesis production, remittence, etc.), attachment-related issues (abutment loosening, bar screw loosening, Locator replacement, fracture of the bar, etc.), and soft tissue-related issues (sore spot, soft tissue proliferation in the lower part of the bar, etc).
Satisfaction survey: Satisfaction with esthetics, retention, and masticatory function regarding the implant overdenture recorded at the final hospital visit was analyzed by using the Likert 5-point scale.23
Statistical analysis: An independent T-test was performed for implant marginal bone resorption, probing depth, and satisfaction, Meanwhile, a chi-square test was utilized for peri-implant inflammation, bleeding index, plaque index, presence of calculus, and complication. The correlations among the implant marginal bone resorption, probing depth, and plaque index were analyzed by using the Pearson's chi-square test. For all statistical analyses, SPSS ver. 21.0 (SPSS Inc., Chicago, IL, USA) was used, and tests were performed at a 5% significance level.
Implant survival rate: A total of 48 implants were placed on 16 patients wearing implant overdenture, and the 16 implants were placed in the LIA group using 2 implants, while the 32 implants were placed in the LBA group using 4 implants. Among them, occlusal loading was applied to 22 implants (LIA group n = 6; LBA group n = 16) during 12 months to 24 months after implant overdenture placement, 18 implants (LIA group n = 6; LBA group n = 12) during 25 months to 36 months, 8 implants (LIA group n = 4; LBA group n = 4) during 37 months to 48 months, and 4 implants (LBA group n = 4) during over 48 months. There was no failed implant, and all implants were functioning normally without clinical mobility (Table 2).
Implant marginal bone resorption and probing depth: The means and standard deviations of the implant marginal bone resorption and probing depth were presented in Table 3. In the LBA group, the implant marginal bone resorption was 1.51 ± 0.13 mm, which was significantly lower than in the LIA group (P < .05), and the probing depth was 2.80 ± 0.16 mm, which was significantly smaller than in the LIA group (P < .05) (Table 3).
Peri-implant inflammation and bleeding index: As a result of measuring the peri-implant inflammation, normal inflammation appeared most frequently, followed by mild inflammation. However, moderate and severe inflammation was not observed in both groups. Mild inflammation occurred more in the LBA group (33.3%) than in the LIA group (12.5%), but the difference was not significant (P > .05). In the bleeding index, petechia most frequently occurred in both groups. Petechia appeared slightly more frequently in the LBA group (73.3%) than in the LIA group (50%); however, it was not significant (P > .05) (Table 4).
Plaque index and calculus: The scores of the plaque index and calculus were higher in the LBA group than in the LIA group. In the case of the plaque index, the state of score 1 perceived upon probing occurred most frequently in both groups, while the LIA group (62.5%) showed a significantly higher frequency as compared to the LBA group (40%) (P < .05). Calculus appeared only in the LBA group (25%) (Table 4).
Correlations among implant marginal bone resorption, plaque index, and probing depth: The correlations among implant marginal bone resorption, plaque index, and probing depth were analyzed. There was no significant correlation between implant marginal bone resorption and plaque index (P > .05), but the implant marginal bone resorption showed a statistically significant correlation with the probing depth (P < .05, R=.606) (Table 5).
Complication: As a result of the analysis, more complications occurred in the LIA group than in the LBA group. In the LIA group, the Locator patrix replacement (50%) and soft tissue sore spot (27%) appeared frequently, while in the LBA group, the Locator patrix replacement (42%) and artificial tooth fracture (29%) appeared frequently (Table 6). The frequency of the Locator patrix replacement was higher in the LIA group (n = 9) than in the LBA group (n = 6).
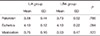
Patient satisfaction: With regard to patient satisfaction with implant overdenture, both groups showed above average satisfaction in retention, esthetics, and mastication. The LIA group for retention and the LBA group for masticatory force revealed a slightly higher satisfaction. However, there was no difference with regard to esthetics. All three cases were not statistically significant (P > .05) (Table 7).
Locator is one of the most widely used attachments due to advantages that it is less limited in the vertical space for implant overdentures production, and the replacement of parts is easy. In order to help understand the clinical use of Locators utilized for mandibular implant overdentures, the cases utilizing a solitary type Locator implant attachment (LIA) and a Locator bar attachment (LBA) splinted with a bar were compared and analyzed.
Among the 16 patients, who were selected for mandibular implant overdenture, the number of females was greater than males. It was similar with the result of a conventional dentures study conducted by Pan et al.24, indicating that satisfaction of females with conventional dentures was lower than that of the males, thus more implant overdentures were produced for females. As a result of the analysis on antagonist teeth, conventional denture accounted for 87%. When compared to a complete mandibular dentures in which degradation of retention occurs due to anatomical limitations in full edentulous patients, the need for implant overdentures seemed to be smaller in a complete maxillary dentures due to sufficient retention and support that can be obtained from the palate, among others.25
As a result of the clinical evaluation based on the criteria of Cochran et al.18, all implants placed for implant overdentures showed a high survival rate by functioning without any mobility during the observation period. Bergendal and Engquist26 reported that mandibular symphysis and ossein between mental foramens are enough for a successful osseointegration of the implants. In this study, all implants were placed between mental foramens, thereby resulting in sufficient osseointegration. They could stand the loading of the implant overdenture, thus a successful treatment was possible.
As for the implant marginal bone resorption, the LIA group showed a higher value than the LBA group (P < .05). In the LBA group, due to the use of a bar with which implants are connected, loading that occurs during mastication is efficiently dispersed, and the stress that causes fine damage is reduced. Therefore, less marginal bone resorption appeared as compared to the LIA group.27 This indicates that the type of connection between the implants has more influence on marginal bone resorption of the implant overdentures than the difference in the Locator type.
The plaque index was higher in the LBA group than in the LIA group, and calculus appeared only in the LBA group. It is thought that due to the nature of the bar, maintaining oral hygiene is difficult in the LBA group, and it is relatively easier in the solitary type LIA group.28 Gotfredsen and Holm29 reported that there was no difference in the gingival index between the ball attachment and bar type attachment in a five-year clinical study. In this study, peri-implant inflammation and bleeding index did not show significant difference between the two groups, but they tended to be slightly higher in the LBA group (P > .05).
Lekholm et al.30 reported that plaque and peri-implant inflammation do not cause implant marginal bone resorption as a result of the 7-year clinical observation. Meanwhile, Quirynen et al.31 reported that implant marginal bone resorption is correlated with probing depth. This study could not find an association between marginal bone resorption of implants used for implant overdenture and plaque index, but implant marginal bone resorption showed a correlation with probing depth, which was consistent with the result of the previous study.
With regard to complications, replacement of the Locator patrix most frequently occurred in both groups, and the frequency was higher in the LIA group than in the LBA group. Walton et al.32 reported that if the implant placement direction is not parallel, the replacement of the Locator patrix frequently occurs. In the LBA group using a bar, the parallel Locator placement is not greatly affected by implant placement inclination, thus the frequency of replacement was relatively less. However, in the LIA group, it is thought that due to an error in parallelism between the implants, abrasion of the Locator patrix frequently occurred when removing the denture. In the LBA group, artificial tooth fracture occurred second most frequently, followed by the replacement of the Locator patrix placed to increase retention, and soft tissue hyperplasia of bar implant overdenture, whose incidence was reported higher in the previous studies, appeared less frequently in this study.33 The reason may be that the prosthesis was produced by securing 2 mm of sufficient space between the bar and soft tissue through a proper interarch space evaluation.34 In the LIA group, a sore spot occurred the second most frequently, followed by the Locator patrix replacement. The reason may be that the proportion of soft tissue loading is greater in the LIA group as compared to the LBA group, while the denture stability is less.35
In both groups, there were no statistically significant differences, but high satisfaction was shown with esthetics, masticatory force, and retention. It is thought that as retention and stability increased compared to a complete denture that the patients used previously, they felt a relatively higher satisfaction with an implant overdenture.3
Due to the limitations of a small number of subjects and a short observation period, this study was not enough to show clinical differences between Locator implant attachment and Locator bar attachment in the mandibular implant overdentures. To overcome these limitations and suggest reliable clinical indications on the Locator, further long-term studies will be required in various institutions.
The following results were obtained within the limit of this study. Implant marginal bone resorption and probing depth were higher in the LIA group (P < .05), while plaque index and frequency of calculus were higher in the LBA group (P < .05). When compared to the LBA group, the LIA group showed a higher incidence of complications, and among them, loss of retention occurred most frequently. The frequency of patrix replacement for restoration of retention was higher in the LIA group than in the LBA group. The LIA group and the LBA group both showed high levels of satisfaction, and there was no significant difference (P > .05).
Figures and Tables
 | Fig. 1Intraoral view of implant overdenture attachment. (A) LIA group: Locator implant attachment utilized with two implants, (B) LBA group: Locator bar attachment utilized with four implants splinted with a bar. |
Table 1
Data of patients and implants
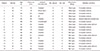
Table 2
Cumulative survival rate of the implants

Table 3
The average value of the marginal bone resorption and probing depth

| LIA group | LBA group | P | |||
|---|---|---|---|---|---|
| Mean | SD | Mean | SD | ||
| Marginal bone resorption (mm) | 1.96 | 0.20 | 1.51 | 0.13 | .04* |
| Probing depth (mm) | 2.91 | 0.24 | 2.80 | 0.16 | .02* |
Table 4
Peri-implant inflammation, bleeding index, plaque index, and calculus
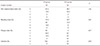
Table 5
Correlation among marginal bone resorption, plaque index, and probing depth (R: Pearson's correlation coefficient)

| Plaque index | Probing depth | |||
|---|---|---|---|---|
| R | P | R | P | |
| Marginal bone resorption | -0.213 | .154 | 0.606 | .001* |
References
1. van Waas MA. The influence of clinical variables on patients' satisfaction with complete dentures. J Prosthet Dent. 1990; 63:307–310.
2. Melas F, Marcenes W, Wright PS. Oral health impact on daily performance in patients with implant-stabilized overdentures and patients with conventional complete dentures. Int J Oral Maxillofac Implants. 2001; 16:700–712.
3. Awad MA, Lund JP, Shapiro SH, Locker D, Klemetti E, Chehade A, Savard A, Feine JS. Oral health status and treatment satisfaction with mandibular implant overdentures and conventional dentures: a randomized clinical trial in a senior population. Int J Prosthodont. 2003; 16:390–396.
4. Batenburg RH, Meijer HJ, Raghoebar GM, Vissink A. Treatment concept for mandibular overdentures supported by endosseous implants: a literature review. Int J Oral Maxillofac Implants. 1998; 13:539–545.
5. Feine JS, Carlsson GE, Awad MA, Chehade A, Duncan WJ, Gizani S, Head T, Heydecke G, Lund JP, MacEntee M, Mericske-Stern R, Mojon P, Morais JA, Naert I, Payne AG, Penrod J, Stoker GT, Tawse-Smith A, Taylor TD, Thomason JM, Thomson WM, Wismeijer D. The McGill consensus statement on overdentures. Mandibular two-implant overdentures as first choice standard of care for edentulous patients. Gerodontology. 2002; 19:3–4.
6. Schneider AL, Kurtzman GM. Bar overdentures utilizing the Locator attachment. Gen Dent. 2001; 49:210–214.
7. Trakas T, Michalakis K, Kang K, Hirayama H. Attachment systems for implant retained overdentures: a literature review. Implant Dent. 2006; 15:24–34.
8. Mericske-Stern RD, Zarb GA. Clinical protocol for treatment with implant-supported overdentures. In : Bolender CE, Zarb GA, Carlsson GE, editors. Boucher's Prosthodontic Treatment for Edentulous Patients. St. Louis: Mosby;1997. p. 527.
9. Burns DR. Mandibular implant overdenture treatment: consensus and controversy. J Prosthodont. 2000; 9:37–46.
10. Schneider AL. The use of a self-aligning, low-maintenance overdenture attachment. Dent Today. 2000; 19:24. 26.
11. Kim MS, Yoon MJ, Huh JB, Jeon YC, Jeong CM. Implant overdenture using a locator bar system by drill and tapping technique in a mandible edentulous patient: a case report. J Adv Prosthodont. 2012; 4:116–120.
12. Technique manual Locator bar attachment system. accessed on 9 December 2015. Available at: http://www.zestanchors.com/media/wysiwyg/pdf/locator/L8003-TM_REV_G_03-14_tech_manual_only.pdf.
13. Vere J, Hall D, Patel R, Wragg P. Prosthodontic maintenance requirements of implant-retained overdentures using the locator attachment system. Int J Prosthodont. 2012; 25:392–394.
14. Wang F, Monje A, Huang W, Zhang Z, Wang G, Wu Y. Maxillary four implant-retained overdentures via locator® attachment: Intermediate-term results from a retrospective study. Clin Implant Dent Relat Res. 2016; 18:571–579.
15. Mackie A, Lyons K, Thomson WM, Payne AG. Mandibular two-implant overdentures: three-year prosthodontic maintenance using the locator attachment system. Int J Prosthodont. 2011; 24:328–331.
16. Akça K, Çavuşoğlu Y, Sağirkaya E, Çehreli MC. Early-loaded one-stage implants retaining mandibular overdentures by two different mechanisms: 5-year results. Int J Oral Maxillofac Implants. 2013; 28:824–830.
17. Krennmair G, Seemann R, Fazekas A, Ewers R, Piehslinger E. Patient preference and satisfaction with implant-supported mandibular overdentures retained with ball or locator attachments: a crossover clinical trial. Int J Oral Maxillofac Implants. 2012; 27:1560–1568.
18. Cochran DL, Buser D, ten Bruggenkate CM, Weingart D, Taylor TM, Bernard JP, Peters F, Simpson JP. The use of reduced healing times on ITI implants with a sandblasted and acid-etched (SLA) surface: early results from clinical trials on ITI SLA implants. Clin Oral Implants Res. 2002; 13:144–153.
19. Yoo HS, Kang SN, Jeong CM, Yoon MJ, Huh JB, Jeon YC. Effects of implant collar design on marginal bone and soft tissue. J Korean Acad Prosthodont. 2012; 50:21–28.
20. Quirynen M, Naert I, van Steenberghe D, Teerlinck J, Dekeyser C, Theuniers G. Periodontal aspects of osseointegrated fixtures supporting an overdenture. A 4-year retrospective study. J Clin Periodontol. 1991; 18:719–728.
21. Loe H, Silness J. Periodontal disease in pregnancy I. Prevalence and severity. Acta Odontol Scand. 1963; 21:533–551.
22. Mombelli A, van Oosten MA, Schurch E Jr, Land NP. The microbiota associated with successful or failing osseointegrated titanium implants. Oral Microbiol Immunol. 1987; 2:145–151.
23. Likert R. A technique for the measurement of attitudes. Arch Psychol. 1932; 22:140–155.
24. Pan S, Awad M, Thomason JM, Dufresne E, Kobayashi T, Kimoto S, Wollin SD, Feine JS. Sex differences in denture satisfaction. J Dent. 2008; 36:301–308.
25. Vervoorn JM, Duinkerke AS, Luteijn F, van de Poel AC. Assessment of denture satisfaction. Community Dent Oral Epidemiol. 1988; 16:364–367.
26. Bergendal T, Engquist B. Implant-supported overdentures: a longitudinal prospective study. Int J Oral Maxillofac Implants. 1998; 13:253–262.
27. Krennmair G, Krainhöfner M, Piehslinger E. Implant-supported mandibular overdentures retained with a milled bar: a retrospective study. Int J Oral Maxillofac Implants. 2007; 22:987–994.
28. Lindquist LW, Rockler B, Carlsson GE. Bone resorption around fixtures in edentulous patients treated with mandibular fixed tissue-integrated prostheses. J Prosthet Dent. 1988; 59:59–63.
29. Gotfredsen K, Holm B. Implant-supported mandibular overdentures retained with ball or bar attachments: a randomized prospective 5-year study. Int J Prosthodont. 2000; 13:125–130.
30. Lekholm U, Adell R, Lindhe J, Brånemark PI, Eriksson B, Rockler B, Lindvall AM, Yoneyama T. Marginal tissue reactions at osseointegrated titanium fixtures. (II) A cross-sectional retrospective study. Int J Oral Maxillofac Surg. 1986; 15:53–61.
31. Quirynen M, van Steenberghe D, Jacobs R, Schotte A, Darius P. The reliability of pocket probing around screw-type implants. Clin Oral Implants Res. 1991; 2:186–192.
32. Walton JN, Huizinga SC, Peck CC. Implant angulation: a measurement technique, implant overdenture maintenance, and the influence of surgical experience. Int J Prosthodont. 2001; 14:523–530.
33. Kuoppala R, Näpänkangas R, Raustia A. Outcome of implant-supported overdenture treatment-a survey of 58 patients. Gerodontology. 2012; 29:e577–e584.
34. Pasciuta M, Grossmann Y, Finger IM. A prosthetic solution to restoring the edentulous mandible with limited interarch space using an implant-tissue-supported overdenture: a clinical report. J Prosthet Dent. 2005; 93:116–120.
35. Meijer HJ, Starmans FJ, Steen WH, Bosman F. Location of implants in the interforaminal region of the mandible and the consequences for the design of the superstructure. J Oral Rehabil. 1994; 21:47–56.




 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download