Abstract
PURPOSE
The aim of the study was to evaluate the effect of abutment shade, ceramic thickness, and coping type on the final shade of zirconia all-ceramic restorations.
MATERIALS AND METHODS
Three different types of disk-shaped zirconia coping specimens (Lava, Cercon, Zirkonzahn: ø10 mm × 0.4 mm) were fabricated and veneered with IPS e.max Press Ceram (shade A2), for total thicknesses of 1 and 1.5 mm. A total of sixty zirconia restoration specimens were divided into six groups based on their coping types and thicknesses. The abutment specimens (ø10 mm × 7 mm) were prepared with gold alloy, base metal (nickel-chromium) alloy, and four different shades (A1, A2, A3, A4) of composite resins. The average L*, a*, b* values of the zirconia specimens on the six abutment specimens were measured with a dental colorimeter, and the statistical significance in the effects of three variables was analyzed by using repeated measures analysis of variance (α=.05).The average shade difference (ΔE) values of the zirconia specimens between the A2 composite resin abutment and other abutments were also evaluated.
RESULTS
The effects of zirconia specimen thickness (P<.001), abutment shade (P<.001), and type of zirconia copings (P<.003) on the final shade of the zirconia restorations were significant. The average ΔE value of Lava specimens (1 mm) between the A2 composite resin and gold alloy abutments was higher (close to the acceptability threshold of 5.5 ΔE) than th ose between the A2 composite resin and other abutments.
The effort of imitating the beauty of natural teeth in the esthetic dentistry led to the development of ceramic copings which had similar translucency and strength to natural teeth. The translucency of coping was recognized as one of the key factors determining the optical characteristics of all-ceramic restorations. The color of ceramic restorations can be expressed according to the CIE L*a*b* system. L* represents lightness, a* represents redness on the positive axis and greenness on the negative axis, and b* represents yellowness on the positive axis, and blueness on the negative axis.
The use of zirconia restorations with adequate translucency and high fracture strength is increasing. The fracture strength of zirconia restorations was reported to be twice that of alumina restorations.123 Relatively thin zirconia coping allowed a sufficient amount of veneering porcelain, making the restoration more translucent.
Recent studies reported that the thickness of the coping and veneering porcelain influenced the final shade of allceramic crowns.456 Repeated sintering was also found to influence the shade of all-ceramic crowns.4 Leucite-reinforced ceramic crowns had a greater thickness effect on a* and b* values, and Spinell ceramic crowns on L* and b* values.5 All-ceramic crowns with low translucency had a less thickness effect, while those with high translucency had a greater thickness effect on their shades.6
Heffernan et al.78 compared the translucency of various all-ceramic crowns. In their study, In-Ceram Spinell, IPS Empress, and IPS Empress 2 showed the highest translucency, with Procera having an intermediate value, and In-Ceram Alumina and In-Ceram Zirconia the lowest translucency. Zirconia crowns have lower translucency than Spinell or Empress crowns, but they may mask the dark shade of a metal post or a stained abutment due to their low translucency.
Because zirconia crowns have been widely used in anterior areas, their esthetic characteristics including translucency were investigated using various methods.78910111213141516 Zirconia crowns became more translucent as they became thinner, although the effect was weaker than that of glass ceramic.9 Zirconia crowns were less translucent than glass ceramic ones with the same thickness because the dense oxide ceramic structure of zirconia allowed more absorption and reflection rather than transmission of light.1011 The translucency of zirconia crowns depended on the coloring and manufacturing methods of the coping, as well as the veneering technique.101112 Color pigmentation of zirconia coping reduced its translucency, while pressed veneering made zirconia crowns more translucent than layered veneering.1012
Two methods, which were absolute and relative translucency measuring methods, have been used for studying the translucency of all-ceramic crowns. The absolute translucency was measured by a spectrophotometer or a spectroradiometer, which detected the whole light transmitted through the ceramic crown. The relative translucency measuring method was used to compare the relative translucency of various all-ceramic crowns by the contrast ratio or translucency parameter that was measured on a black and white background.678910111213141516 Some zirconia crowns with high translucency were proven to have light-scattering characteristics similar to human dentin in recent studies, but they showed higher L* and lower a*, b* values than dentin.14
There have been some recent studies on the shade-masking ability of highly translucent lithium disilicate glassceramics,171819 but similar studies on zirconia crowns were not common. The purpose of the present study was to evaluate the effects of abutment shade, ceramic thickness, and coping type on the final shade of three different types of zirconia crowns, and also to evaluate the masking ability of zirconia crowns with different thicknesses and abutment shades. The null hypothesis was that there were no significant differences in the average L*, a*, b* values of zirconia specimens with different abutment shades, ceramic thicknesses, and coping types.
Disk-shaped zirconia copings with uniform dimensions (Ø 10 mm × 0.4 mm) were prepared from three different zirconia systems: Lava (3M ESPE, St. Paul, MN, USA), Cercon (Degudent GmbH, Hanau, Germany), and Zirkonzahn (Zirkonzahn GmbH, Gais, Italy). The zirconia copings went through milling, cleaning, and drying as pre-sintered zirconium oxide. They were then sintered according to the manufacturer's instructions and ground using 1000 grit sandpaper. Each zirconia system had twenty coping specimens.
IPS e.max Press Ceram powder (A2 shade, Ivoclar Vivadent, Schaan, Liechtenstein) was built up and sintered on the prepared zirconia copings to total thicknesses of 1 mm (0.4 mm coping + 0.1 mm liner + 0.3 mm dentin porcelain + 0.2 mm enamel porcelain)and 1.5 mm (0.4 mm coping + 0.1 mm liner + 0.7 mm dentin porcelain + 0.3 mm enamel porcelain), as measured with an electronic caliper (Model-DC515, Lutron Electronic Enterprise Co., Ltd., Taipei, Taiwan). After the exact thicknesses were achieved, the zirconia specimens were glazed. The whole fabrication procedure was performed by one dental laboratory technician. Each zirconia specimen was cleaned in an ultrasonic cleaner for 5 minutes and dried. Zirconia restoration specimens were divided into six groups (Lava 1 mm (L1), Lava 1.5 mm (L1.5), Cercon 1 mm (C1), Cercon 1.5 mm (C1.5), Zirkonzahn 1 mm (Z1), and Zirkonzahn 1.5 mm (Z1.5)) according to their thickness and coping type. Each group had ten specimens.
The abutment specimens were made of gold alloy (type III; Pontor MPF, Cendres+Métaux SA, Biel/Bienne, Switzerland), base metal alloy (Nickel-chromium; Argeloy N.P. Special, the Argen Cor., San Diego, CA, USA), and composite resin (A1, A2, A3, A4 shades, Herculite Precis Enamel, Kerr, Orange, CA, USA). A silicone putty (Extrude XP Putty, Kerr, Orange, CA, USA) mold with disk-shaped holes (ø10 mm × 3 mm) was prepared and applied in the holes with petroleum jelly. Cold curing orthodontic acrylic resin (Ortho-Jet, Lang Dental, Wheeling, IL, USA) powder and liquid were mixed and poured in the holes of the putty mold. The fully polymerized acrylic resin disks were then separated from the silicone putty mold, invested, and cast into type III gold alloy and nickel-chromium alloy. The disk-shaped cast alloy specimens were trimmed and polished to 3 mm-thickness. Composite resin was filled in the holes of the transparent plastic mold(ø10 mm × 7 mm) applied with petroleum jelly and light-cured (A pilot study for evaluating the thickness of the resin abutment sufficient to mask the background shade was performed, and the minimum thickness was found to be 7 mm). The cured resin specimens were separated from the mold, and ground to 7 mm-thickness with 1000 grit sandpaper. The abutment specimens were divided into six groups (BM (base metal alloy), G (type III gold alloy), A1, A2, A3, and A4 (composite resins)) based on the materials used.
The CIE L*a*b* values of six abutment specimens were measured with a dental colorimeter (ShadeEye NCC, Shofu Inc., Kyoto, Japan) when the abutment specimens were placed on a black background (L = 8.6, a = 1.3, b = 0.5) and a white background (L = 91.1, a = 2.6, b = -7.1). Translucency parameter (TP) values representing the translucency of six abutments were obtained by applying the following equation.9 The TP values of six ceramic specimens with different thicknesses and coping types were also obtained (Table 1). TP values below 2 were considered to represent the material with translucency low enough to completely mask the black background.10 The color measurement by the dental colorimeter used D65 as a light source under the standard lighting system (Super Light-VI, BoTeck, GunPo, Korea). The dental colorimeter was calibrated, and measurements were made using an elastic touch probe placed perpendicular to the specimens on a 45 degree plate (45/0-degree geometry).
L*: brightness, a*: redness to greenness, b*: yellowness to blueness, B: black background, W: white background
Six groups of the zirconia specimens were matched with six groups of the abutment specimens for the final shade evaluation. Each zirconia specimen was stabilized on each abutment specimen with translucent Choice try-in paste (Bisco Inc., Schaumburg, IL, USA). The color of the zirconia specimens on the abutments was measured three times in the 'analyze mode' using a dental colorimeter (ShadeEye NCC, Shofu Inc., Kyoto, Japan). The L*, a*, and b* values of each combination were obtained and averaged.
In addition, the shade-masking ability of the zirconia specimens measured on the different shades of abutments was evaluated. The shade difference values (ΔE) of the zirconia specimens between the A2 shade and other shades of the abutments were obtained by the following equation. Based on previous studies, any shade difference values (ΔE) that were less than 2.6 were regarded as clinically shadematched (not-perceptible), and any ΔE values greater than 5.5 were regarded as clinically unacceptable.20212223
L*: brightness, a*: redness to greenness, b*: yellowness to blueness
Repeated measures analysis of variance (α = .05) was used to evaluate the statistical significance of the effects of the ceramic thickness, abutment shade, and types of coping on the final shade of the zirconia specimens. SAS for Windows (9.3, SAS Institute Inc., Cary, NC, USA) was used for the statistical analysis.
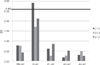
The average L*, a*, b* values of the zirconia specimens on the abutments are shown in Fig. 1, Fig. 2, and Fig. 3. When the ceramic thickness increased from 1 to 1.5 mm, the L* value decreased, and the a* and b* values increased. The gold abutment (G) showed the highest L*, a*, b* values, and the base metal abutment (BM) had the lowest L*, b* values. The average L*, a*, b* values of three types of the zirconia specimens with 1 and 1.5 mm thicknesses are compared in Fig. 4. The a* and b* values showed little difference among the zirconia specimens, but the lowest L* value was observed in the Lava specimens. According to the results from the repeated measures analysis of variance, there were significant effects of the ceramic thicknesses (P < .001), abutment shades (P < .001), and types of zirconia coping (P < .003) on the final shade of the zirconia restorations.
In a clinical case, zirconia crowns can be placed on adjacent abutments with different shades. The type and thickness of the zirconia crowns should be determined to mask the abutment shade differences. In this study, the gold abutment (G) showed the highest L*, a*, and b* values, and other abutments showed lower values with only minute differences among themselves. It was necessary to determine whether these differences were within the acceptable range of the human eye. The shade differences (ΔE) of the zirconia specimens between the A2 resin (control: the same shade as the ceramic specimens) and other shades of abutments were compared in Fig. 5 and Fig. 6. For the 1 mmthick zirconia specimens, the ΔE value between the gold alloy and A2 resin abutments was the greatest (> 2.6). Other abutments showed minor differences (ΔE) from the A2 resin abutment, and the values were 1 or less. Lava showed the highest ΔE value (5.5) between the A2 resin and gold alloy abutments, and Zirkonzahn showed the lowest. The 1.5 mm-thick ceramic specimens had overall lower ΔE values (< 2.6 except Lava between A2 and gold) than the 1 mm-thick ones.
The null hypothesis in the present study was rejected based on the results showing significant differences in L*, a*, b* values related to abutment shade, ceramic thickness and coping type. The influence of the abutment shade on the final color of the all-ceramic crowns was significant, affecting the L*, a*, and b* values, as shown in Fig. 1, Fig. 2, and Fig. 3. The zirconia specimens, when measured on the gold alloy abutments, showed the highest L*, a*, and b* values, regardless of the ceramic thickness or coping type. This result was in agreement with the previous study. Shimada et al.24 found in their colorimeter study that the all-ceramic crowns placed on gold alloy abutments showed significantly higher L*, a*, and b* values than those on composite or silver-palladium alloy abutments. They used IPS Empress 2 for ceramic specimens. In contrast, Azer et al.25 found that the final shade of the IPS Empress crowns was not affected by the different shades of the composite cores. They used composite cores with small differences in shade, such as A3, B3, C3, and D3.
Shimada et al.24 also found in their study that not only the abutment shade but also the ceramic thickness (0.8, 1, 1.2, 1.4, 1.6, 1.8 mm) affected the final shade of IPS Empress 2 specimens. Dozić et al.26 reported that the ceramic thickness was inversely related to the translucency and could affect the final shade of the all-ceramic crown. The present study compared the shade values of the 1 mmand 1.5 mm-thick zirconia specimens and found a significant difference between the thicknesses.
Wang et al.9 showed there were differences in translucency among various zirconia ceramics, such as Cercon Base, Lava, or Zenotec. Crispin et al.27 reported that one of the primary elements affecting the shade of all-ceramic crowns was the translucency of the coping. In the present study, the translucency of each zirconia system was not directly measured. Instead, the shade of zirconia specimens placed on different shades of abutments was measured. The type of zirconia coping was, thus, found to affect the final shade of the zirconia restoration.
In the present study, ΔE values of the zirconia specimens between the A2 and other shades of abutments were obtained to evaluate the shade masking ability of the zirconia crowns. The ΔE values of three types (L, C, and Z) of 1 mm-thick zirconia specimens were all found to be the highest (> 2.6) between the A2 resin and gold alloy abutments, compared to other abutments. Lava (L), among three types, showed the highest ΔE value (close to 5.5) between the A2 resin and gold alloy abutments (Fig. 5). For the 1.5 mmthick zirconia specimens, all three types also showed the highest ΔE values between the A2 resin and gold alloy abutment, and Lava (L) presented a ΔE value between 2.6 and 5.5 (Fig. 6). Although the translucency of Lava zirconia crowns was lower than that of IPS e.max Press or InCeram Spinell, the shade of a gold alloy post and core adjoining an A2 shade tooth would not be completely masked even with Lava zirconia crowns.79
There have been some studies on the minimum color difference (ΔE) perceivable by human observers. Seghi et al.28 stated that alterations in color perception could occur as a result of any number of uncontrolled factors, including fatigue, aging, emotions, lighting conditions, and metamerism, but human eye-brain combinations could detect very small differences in color between two objects. They reported that a measured color difference value of greater than 2 ΔE units was correctly detected by the observer group 100% of the time, and incorrect judgments were made only infrequently by the observers when the measured color difference fell within the 1 to 2 ΔE unit range. Compared to the perceptibility threshold, some researchers have reported that the color difference accepted by 50% of observers is 1.7 - 3.3 ΔE units.202123 Due to some intraoral variables, the clinically perceptible and acceptable color differences were reported to have higher values than those measured in a strictly controlled in vitro environment.2021222329 In the present study, therefore, 2.6 and 5.5 ΔE units were adopted as the 50% clinical perceptibility and acceptability thresholds.
The present study was aimed at not only finding the factors that affect the final shade of zirconia crowns, but also evaluating the masking ability of zirconia crowns on different shades of abutments. The shade of all of the veneered zirconia specimens was A2, which was thus chosen as the control abutment shade for comparison with other ones. Other shades of zirconia and abutment specimens also need to be compared for clinical applications.
The shade of abutments made of composite resin, in the present study, could be influenced by the background color if the abutment specimen was not thick enough for masking the color. TP values for four 7 mm-thick resin abutments were found to range from 0.5 to 1.42. Because TP values below 2 indicated the 100% masking ability for a black background, the four resin abutments were not affected by the shade of the background.91728
The ShadeEye NCC Chromameter (Shofu Inc., Kyoto, Japan) used in the present study is a closed-type dental colorimeter, which might introduce 'edge loss error' when measuring the color of translucent specimens.3031 'Edge loss error' occurs when light from an illuminant travels through the small window of the colorimeter. Some of the light cannot go back into the sensor window of the colorimeter when reflected. As a result, the repeatedly measured value of the color might have some variations. This closed window type colorimeter is thought to be less influenced by the outside light.
Within the limitations of an in-vitro study in mind, the present study demonstrated there were significant influences of the ceramic thickness, abutment shade and type of coping on the resulting color of three zirconia restorations (Lava, Cercon, and Zirkonzahn). Evaluations of the ΔE values of zirconia specimens (A2 shade) between different shades of abutments led to the following clinical implication: Lava crowns, when placed on a gold alloy post, may not be shade-matched with an adjacent tooth.
Figures and Tables
 | Fig. 1Mean L*a*b* values of Lava (L) zirconia specimens on different shades of abutment specimens. (A) Mean L* values, (B) Mean a* values, (C) Mean b* values.Abbreviations; L1: Lava 1 mm, L1.5: Lava1.5 mm, BM: base metal alloy, G: gold alloy, A1-A4: A1-A4 shades of composite resin, L*: lightness, a*: redness(+).greenness(-), b*: yellowness(+)/blueness(-).
|
 | Fig. 2Mean L*a*b* values of Cercon (C) zirconia specimens on different shades of abutment specimens. (A) Mean L* values, (B) Mean a* values, (C) Mean b* values.Abbreviations; C1: Cercon 1 mm, C1.5: Cercon 1.5 mm, BM; base metal alloy, G: gold alloy, A1- A4: A1-A4 shades of compsite resin, L*: lightness, a*: redness(+).greenness(-), b*: yellowness(+)/blueness(-).
|
 | Fig. 3Mean L*a*b* values of Zirkonzahn (Z) zirconia specimens on different shades of abutment specimens. (A) Mean L* values, (B) Mean a * values, (C) Mean b* values.Abbreviations; Z1: Zirkonzahn 1 mm, Z1.5: Zirkonzahn 1.5 mm, BM: base metal alloy, G: gold alloy, A1-A4: A1-A4 shades of composite resin, L*: lightness, a*: redness(+)/greenness(-), b*: yellowness(+)/blueness(-).
|
 | Fig. 4Mean L* a* b* values of Lava (L), Cercon (C), and Zirkonzahn (Z) zirconia specimens on abutment specimens. (A) Mean L* values, (B) Mean a* values, (C) Mean b* values.Abbreviations; L*: lightness, a*: redness(+)/greenness(-), b*: yellowness(+)/blueness(-).
|
 | Fig. 5ΔE values of zirconia specimens (1 mm thickness) between A2 resin and other shades of abutment specimens.Abbreviations; L1: Lava 1 mm, C1: Cercon 1 mm, Z1: Zirkonzahn 1 mm, BM: base metal alloy abutment, G: gold alloy abutment, A1-A4: A1-A4 shades of composite resin abutment, ΔE: shade difference.
|
 | Fig. 6ΔE values of zirconia specimens (1.5 mm thickness) between A2 resin and other shades of abutment specimens.Abbreviations; L1.5: Lava 1.5 mm, C1.5: Cercon 1.5 mm, Z1.5: Zirkonzahn 1.5 mm, BM: base metal alloy abutment, G: gold alloy abutment, A1-A4: A1-A4 shades of composite resin abutment, ΔE: shade difference.
|
ACKNOWLEDGEMENTS
We thank to Kyoung-Sik Park for his excellent laboratory work of the ceramic specimens and Seon-Woo Kim for the excellent statistical analysis.
References
1. Piconi C, Maccauro G. Zirconia as a ceramic biomaterial. Biomaterials. 1999; 20:1–25.
2. Ozkurt Z, Kazazoglu E, Unal A. In vitro evaluation of shear bond strength of veneering ceramics to zirconia. Dent Mater J. 2010; 29:138–146.
3. Kelly JR, Nishimura I, Campbell SD. Ceramics in dentistry: historical roots and current perspectives. J Prosthet Dent. 1996; 75:18–32.
4. Uludag B, Usumez A, Sahin V, Eser K, Ercoban E. The effect of ceramic thickness and number of firings on the color of ceramic systems: an in vitro study. J Prosthet Dent. 2007; 97:25–31.
5. Shokry TE, Shen C, Elhosary MM, Elkhodary AM. Effect of core and veneer thicknesses on the color parameters of two all-ceramic systems. J Prosthet Dent. 2006; 95:124–129.
6. Antonson SA1, Anusavice KJ. Contrast ratio of veneering and core ceramics as a function of thickness. Int J Prosthodont. 2001; 14:316–320.
7. Heffernan MJ, Aquilino SA, Diaz-Arnold AM, Haselton DR, Stanford CM, Vargas MA. Relative translucency of six all-ceramic systems. Part I: core materials. J Prosthet Dent. 2002; 88:4–9.
8. Heffernan MJ, Aquilino SA, Diaz-Arnold AM, Haselton DR, Stanford CM, Vargas MA. Relative translucency of six all-ceramic systems. Part II: core and veneer materials. J Prosthet Dent. 2002; 88:10–15.
9. Wang F, Takahashi H, Iwasaki N. Translucency of dental ceramics with different thicknesses. J Prosthet Dent. 2013; 110:14–20.
10. Spyropoulou PE, Giroux EC, Razzoog ME, Duff RE. Translucency of shaded zirconia core material. J Prosthet Dent. 2011; 105:304–307.
11. Baldissara P, Llukacej A, Ciocca L, Valandro FL, Scotti R. Translucency of zirconia copings made with different CAD/CAM systems. J Prosthet Dent. 2010; 104:6–12.
12. Luo XP, Zhang L. Effect of veneering techniques on color and translucency of Y-TZP. J Prosthodont. 2010; 19:465–470.
13. Lim HN, Yu B, Lee YK. Spectroradiometric and spectrophotometric translucency of ceramic materials. J Prosthet Dent. 2010; 104:239–246.
14. Pecho OE, Ghinea R, Ionescu AM, Cardona Jde L, Paravina RD, Pérez Mdel M. Color and translucency of zirconia ceramics, human dentine and bovine dentine. J Dent. 2012; 40:e34–e40.
15. Barizon KT, Bergeron C, Vargas MA, Qian F, Cobb DS, Gratton DG, Geraldeli S. Ceramic materials for porcelain veneers. Part I: Correlation between translucency parameters and contrast ratio. J Prosthet Dent. 2013; 110:397–401.
16. Spink LS, Rungruanganut P, Megremis S, Kelly JR. Comparison of an absolute and surrogate measure of relative translucency in dental ceramics. Dent Mater. 2013; 29:702–707.
17. Chaiyabutr Y, Kois JC, Lebeau D, Nunokawa G. Effect of abutment tooth color, cement color, and ceramic thickness on the resulting optical color of a CAD/CAM glass-ceramic lithium disilicate-reinforced crown. J Prosthet Dent. 2011; 105:83–90.
18. Ali AAB, Kang K, Finkelman MD, Zandparsa R, Hirayama H. The effect of variations in translucency and background on color differences in CAD/CAM lithium disilicate glass ceramics. J Prosthodont. 2014; 23:213–220.
19. Charisis D, Koutayas SO, Kamposiora P, Doukoudakis A. Spectrophotometric evaluation of the influence of different backgrounds on the color of glass-infiltrated ceramic veneers. Eur J Esthet Dent. 2006; 1:142–156.
20. Douglas RD, Brewer JD. Acceptability of shade differences in metal ceramic crowns. J Prosthet Dent. 1998; 79:254–260.
21. Ragain JC Jr, Johnston WM. Color acceptance of direct dental restorative materials by human observers. Color Res Appl. 2000; 25:278–285.
22. Douglas RD, Steinhauer TJ, Wee AG. Intraoral determination of the tolerance of dentists for perceptibility and acceptability of shade mismatch. J Prosthet Dent. 2007; 97:200–208.
23. Ruyter IE, Nilner K, Moller B. Color stability of dental composite resin materials for crown and bridge veneers. Dent Mater. 1987; 3:246–251.
24. Shimada K, Nakazawa M, Kakehashi Y, Matsumura H. Influence of abutment materials on the resultant color of heat-pressed lithium disilicate ceramics. Dent Mater J. 2006; 25:20–25.
25. Azer SS, Ayash GM, Johnston WM, Khalil MF, Rosenstiel SF. Effect of esthetic core shades on the final color of IPS Empress all-ceramic crowns. J Prosthet Dent. 2006; 96:397–401.
26. Dozić A, Kleverlaan CJ, Meegdes M, van der Zel J, Feilzer AJ. The influence of porcelain layer thickness on the final shade of ceramic restorations. J Prosthet Dent. 2003; 90:563–570.
27. Crispin BJ, Okamoto SK, Globe H. Effect of porcelain crown substructures on visually perceivable value. J Prosthet Dent. 1991; 66:209–212.
28. Seghi RR, Hewlett ER, Kim J. Visual and instrumental colorimetric assessments of small color differences on translucent dental porcelain. J Dent Res. 1989; 68:1760–1764.
29. Johnston WM, Kao EC. Assessment of appearance match by visual observation and clinical colorimetry. J Dent Res. 1989; 68:819–822.
30. Bolt RA, Bosch JJ, Coops JC. Influence of window size in small-window colour measurement, particularly of teeth. Phys Med Biol. 1994; 39:1133–1142.
31. Johnston WM, Hesse NS, Davis BK, Seghi RR. Analysis of edge-losses in reflectance measurements of pigmented maxillofacial elastomer. J Dent Res. 1996; 75:752–760.




 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download