Abstract
PURPOSE
The aim of this study was to compare the changes in retentive force of stud attachments for implant overdentures by in vitro 2-year-wear simulation.
MATERIALS AND METHODS
Three commercially available attachment systems were investigated: Kerator blue, O-ring red, and EZ lock. Two implant fixtures were embedded in parallel in each custom base mounting. Five pairs of each attachment system were tested. A universal testing machine was used to measure the retentive force during 2500 insertion and removal cycles. Surface changes on the components were evaluated by scanning electron microscopy (SEM). A Kruskal-Wallis test, followed by Pairwise comparison, was used to compare the retentive force between the groups, and to determine groups that were significantly different (α<.05).
RESULTS
A comparison of the initial retentive force revealed the highest value for Kerator, followed by the O-ring and EZ lock attachments. However, no significant difference was detected between Kerator and O-ring (P>.05). After 2500 insertion and removal cycles, the highest retention loss was recorded for O-ring, and no significant difference between Kerator and EZ lock (P>.05). Also, Kerator showed the highest retentive force, followed by EZ lock and O-ring, after 2500 cycles (P<.05). Based on SEM analysis, the polymeric components in O-ring and Kerator were observed to exhibit surface wear and deformation.
A complete denture has been the standard treatment strategy to restore functionality and aesthetics in edentulous patients. From the aesthetic point of view, replacing the missing natural teeth with a complete denture provides satisfactory results. However, it is a great challenge to achieve satisfactory results in terms of reduced pain, increased stability, retentive force, and occlusal load support;12 especially in the case of a mandibular arch presenting severe resorption of the alveolar ridge, the use of a complete denture involves great difficulties.3
Since the introduction of the concept of osseointegration by Brånemark, various prosthetic treatment options using osseointegrated implants have been applied in the treatment of edentulous patients, with high success rates being demonstrated in longitudinal clinical studies.456 Implant treatment options for edentulous patients can be classified into the fixed prosthesis and removable prosthesis types.7 A fixed prosthesis provides psychological stability and greatly improves masticatory performance, but presents disadvantages related to aesthetics and pronunciation, oral hygiene care, and the need for an increased number of implants.8 In contrast, the advantages of a removable prosthesis, such as an implant overdenture, include improved aesthetics and oral hygiene care, easier fabrication of prosthodontic restorations, and cost-effectiveness. Disadvantages of this type include the psychological resistance to wearing a removable part and the need for relining, resulting from continuous resorption of the posterior residual ridge.8 A severely resorbed ridge could adversely affect the jaw relation or interocclusal distance, making it difficult to place a sufficient number of implants; however, a removable prosthesis requiring a small number of implants was proven to be more advantageous than a fixed prosthesis, in terms of biomechanical consequences.9 The 2002 McGill Consensus recommended a mandibular 2-implant overdenture as the first-choice standard of care for edentulous patients.10 Moreover, empirical studies have reported that patients wearing implant overdentures display higher masticatory performance and denture-related satisfaction, and experience less problems with the dentures in daily life, compared to patients wearing conventional complete dentures.1112
Implant overdentures consist of the implant, an abutment including the attachment, and a denture base, which accommodates counterpart attachment.13 The selection of the appropriate overdenture attachment system greatly influences patient satisfaction, because of its direct association with the stability of the denture and the retentive force.14 The attachment system could be either a bar attachment or a stud attachment.15 The advantages of bar attachment include allowing the splinting of implants and improving the retentive force and stability; however, it presents difficulties in meeting the oral hygiene requirements.16 In comparison, the stud attachment offers easier oral hygiene management and less problems related to the limited inter-arch space.17 Furthermore, due to additional advantages including cost-effectiveness, simple fabrication design, and easy repair, various stud attachments such as the Locator attachments are preferred by many practitioners.18
The most common mechanical problem presented by implant overdentures is the loss in retention, caused by wear, deformation, and fracture of the components of the attachment system over time.1920 A number of studies have reported that changes in the attachment surface lead to the loss of frictional contact through the loosening of the attachment components. Changes in the mechanical properties of the materials used, especially the hardness and elastic modulus, could affect the wear pattern.21222324 With the popularization of implant overdentures, a wide range of stud attachments of various designs and composed of different materials have been used in clinical settings. Despite this widespread use, the wear properties or retention loss resulting from long-term use of attachment are yet to be extensively researched.
The purpose of this study was to compare the changes in retentive force and patterns of surface wear of three types of stud attachments by measuring retentive force and evaluating surface changes over repetitive insertion and removal cycles.
The upper mounting that accommodated the counterpart attachment of the attachment system was fabricated using an orthodontic acrylic resin block (Orthodontic resin; Dentsply, York, PA, USA) with dimensions of 44 × 27 × 47 mm (Fig. 1A). Two holes (8 mm in diameter) were prepared on this block, positioned 22 mm apart (Fig. 1B).25 An acrylic resin block was fabricated as the lower mounting for placement of the implant fixture, with the same dimension as the upper mounting (Fig. 1A). Two 10 mm length holes (22 mm apart) were drilled parallel to each other and perpendicular to the horizontal surface, using an 4.1 mm drill (Osstem Implant Co., Busan, Korea). Two implant fixtures were inserted (S-clean 4.0 × 10 mm; Dentis Co., Daegu, Korea) into the holes of the lower mounting and fixed with acrylic resin (Orthodontic resin; Dentsply) (Fig. 1C). An index in the center region of each block was prepared, in order to check whether the upper mounting fits exactly into the lower mounting.
Three types of stud attachments were investigated: (1) Kerator (Daekwang IDM Co., Seoul, Korea), comprised of a nylon matrix and a cylindrical patrix, (2) O-ring (Dentis Co., Daegu, Korea), with a rubber matrix and a ball patrix, and (3) EZ lock (Samwon Co., Yangsan, Korea), composed of titanium springs and ceramic balls (Fig. 2, Table 1).
The abutments including the attachments were screwed into their respective implant fixtures, in accordance with the manufacturer protocols, using the specified drivers and torque wrenches (Straumann AG, Basel, Switzerland). The abutments comprising the Kerator and O-ring attachments were fastened with 30 Ncm, and that containing the EZ lock was fastened with 20 Ncm. The black matrix was inserted to the metal housing for the Kerator and O-ring attachments, and placed on the corresponding patrix. All spaces between the metal housing and abutment were blocked out using baseplate wax to prevent the flow of acrylic resin into the areas with undercuts and the upper mounting placed accurately upon the lower mounting. An adequate amount of autopolymerizing acrylic resin (Pattern Resin, GC Co., Tokyo, Japan) was applied to the relief areas of the upper mounting, completely covering the metal housing. After 20 minutes following the separation of the upper and lower mountings, wax and excess acrylic resin were removed with a sharp scalpel. Both parts were stored at room temperature for over 24 hours to allow complete polymerization. The black matrices of the Kerator and O-ring attachments were then replaced with blue nylon and red rubber for testing, respectively (Fig. 3). A total of 15 specimens (5 per attachment system) were prepared in this manner.
All specimens were subjected to repeated insertion and removal cycles, and the respective retentive forces measured using a universal testing machine (MTS systems Co., Eden Prairie, MN, USA). The lower mounting was seated on the fixed part of this machine, while the upper mounting was attached to the operation part. The specimen was placed in a position such that the force could be applied in a perpendicular direction, verifying the accurate placing of the upper mounting onto the lower mounting.
The crosshead speed for the simulation was set at 60 mm/min, which mimicked the speed with which a patient removes his/her denture according to clinical instructions. The mountings were subjected to 2500 cycles of insertion and removal, a value calculated on a 2-year basis, under the assumption that the process of insertion and removal of the denture is repeated by a patient 3-4 times a day.26 The retentive force of each attachment system was measured 3 times, at baseline and the end of 100, 250, 500, 1000, 2000, and 2500 cycles.
Upon completion of the 2500 cycles of insertion and removal, the wear and deformation on each attachment surface was examined by scanning electron microscopy analysis (S-3500, Hitachi Ltd., Tokyo, Japan).
For statistical analysis of the results, the Statistical Package for Social Sciences (SPSS) software, version 21 (IBM SPSS Statistics, Chicago, IL, USA) was used. The Shapiro-Wilk test and Levene's test were performed to validate the normality of distribution and homogeneity of variance, respectively. These were followed by the Kruskal-Wallis test and pairwise comparison for the validation of statistical significance of the difference according to the attachment system. The pre-post difference after 2500 cycles of insertion and removal was compared by paired-sample t-test. For all values, a significance level of 5% was applied to establish statistical significance.
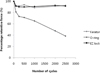
Table 2 and Fig. 4 present the means and standard deviations of the retentive force for each attachment system, measured during the repeated insertion and removal cycles.
The greatest initial retentive force was demonstrated by the Kerator (12.80 N), followed by the O-ring (9.19 N) and EZ lock (5.93 N); there was no statistically significant difference between the Kerator and O-ring (P>.05). The greatest final retentive force after 2500 cycles of insertion and removal was demonstrated by Kerator (11.87 N), followed by EZ lock (5.43 N) and O-ring (3.54 N), with all differences being statistically significant (P<.05).
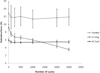
Significant retention loss was observed in all three attachment systems upon completion of the 2500 cycles of insertion and removal, compared to the initial retentive force (P<.05). The greatest retention loss rate, i.e. the difference between the initial retentive force and final retentive force (completion of 2500 cycles of insertion and removal), was observed in the O-ring (5.66 N, 61.54%), followed by the EZ lock (0.50 N, 8.43%) and Kerator (0.93 N, 7.26%) (Fig. 5 and Fig. 6). However, there was no statistically significant changes between EZ lock and Kerator (P>.05). On the other hand, upon comparison of the standard deviation and coefficient of variation for the retentive force at each measurement step, the Kerator was observed to present higher values compared to the other two systems.
Scanning electron microscopy (SEM) of the surface morphology of the attachments upon completion of 2500 insertion and removal cycles revealed that the nylon matrix of Kerator and the rubber matrix of O-ring incurred noticeable deformation and deterioration, whereas the ceramic ball of the EZ lock did not exhibit any noticeable signs of wear, except for slight surface scratches (Fig. 7). With regards to the patrix for all attachments, a strip-shaped wear track was observed on the titanium alloy of O-ring, whereas the TiN-coated titanium alloy of Kerator and EZ lock did not display any perceivable surface changes or damages (Fig. 8).
The implant overdenture is a removable prosthesis obtaining retention and support through attachment, with the choice of attachment system being directly associated with patient satisfaction and prosthetic prognosis. A wide variety of attachment systems are currently available; each possess their respective advantages and disadvantages, and the selection must be made based on the individual patient dental arch shape, interarch space, ease of adjustment, functional life, and retentive force.13
There has been no clear consensus concerning the optimal retentive force of a denture. However, according to a previous report, a stud attachment should have a retentive force of at least 4 N.27 A 20N retentive force (approximate) is considered to be sufficient for a 2-implant mandibular overdenture, whereas a 5-7 N retentive force is believed to support the stabilization of implant overdentures.2829 However, a very limited amount of data with regards to the retentive force of the attachment is provided by the manufacturers. In addition, the literature regarding the initial retentive force of the attachment system varies widely, even for similar types of attachment systems, depending on the experimental conditions, such as the direction of application of force, crosshead speed, and the distance and angle of attachments.24
The mean value of the initial retentive force observed for each of the three types of stud attachments examined in this study was 12.80 N for Kerator, 9.19 N for O-ring, and 5.93 N for EZ lock. The final retentive force values were 11.87, 5.43, and 3.54 N for the Kerator, EZ lock, and O-ring attachments, respectively. It might be advisable to improve the retentive force of the dentures containing attachments such as the EZ lock (which demonstrates a low initial retentive force) or the O-ring (displaying a large retention loss) according to the functional aspect of the magnitude of retentive force. This could be achieved by securing the largest possible area for the coverage of the denture base, and providing adequate border sealing within the neutral zone between the tongue and cheeks, similar to when producing a conventional complete denture.
Examinations of the attachments following repeated insertion and removal revealed less retention loss in Kerator compared to the O-ring, and a statistically non-significant difference from that of EZ lock. The Kerator attachment system is a solitary and resilient type, similar to the Locator attachment system. It is easy to insert and remove, and constitutes a dual retention system that includes inside and outside of the patrix, with the nylon matrix linked to the implant. Moreover, it is comprised of a nylon matrix displaying varied retentive force, allowing for easy adjustment of the retentive force. In this experiment, a blue nylon matrix, expressing similar initial retentive force as the O-ring, was used to minimize the influence of the initial retentive force. Despite such similar baseline conditions, an evaluation of the initial retentive force of two Kerator specimens demonstrated higher values than the retentive force (5.3 N) presented by the manufacturer. This may be due to a production quality fluctuation; however, it may also be explained by the intra-matrix redistribution of undercuts for the moment of a force likely to occur despite the vertical removal force applied in the experiment, along with the additive effects of the retentive force obtained by acting as a guiding plane of inner core of the nylon matrix against removal force.26
As depicted in the SEM images, the nylon matrix of Kerator incurred substantial deformation and deterioration, especially in the central core area, compared to the outer ring area. Such surface loss appears to be gross surface deformation and cohesive failure, associated with the specific component composition of nylon. The slight retention loss in the Kerator attachment, despite the serious deformation and deterioration, is considered to be consistent with the fact that the outer ring is primarily responsible for the retentive force, rather than the seriously deteriorated core. On the other hand, the increased retention loss may also be expected due to the extensive creep response of nylon (which has a low glass transition temperature) in the 37℃ humid oral environment, and its strong affinity for water uptake, which triggers additional creep, and accelerates wear and deformation.30
The Kerator retention loss pattern, which depends on the cycles of insertion and removal, shows a peculiar fluctuation: an initial decrease in the retentive force, followed by an increase. This phenomenon could be attributed to the increased surface roughness as a result of the surface change caused by repeated insertion and removal. This in turn increases fine mechanical friction, ultimately resulting in the increase in retentive force.31
On the other hand, as previously mentioned, the O-ring showed the highest retention loss after 2500 insertion and removal cycles, with the loss in retentive force increasing linearly in proportion to the number of insertion and removal cycles. The O-ring attachment demonstrated the highest fluidity, with the retentive force being a result of the elasticity of its rubber ring, undercut structure of the patrix, and the frictional resistance between the rubber ring and patrix. Rubber generates friction as a result of the contact force on the contact surface, and the deformation of the rubber itself. The frictional force of rubber is comprised of hysteresis and adhesion, and is caused by the visco-elastic properties of rubber. The coefficient of friction between metal and rubber is much higher than that between metal and metal, as are the frictional force and wear speed. Rubber shows a peculiar tendency of wear because of a variety of complex factors. While materials such as metal and plastic generate scratches parallel to the wear directions, rubber forms a ridge pattern perpendicular to the wear direction, and concurrently, small rubber debris.32 Surface wear or tear resulting from this mechanism may trigger a fine increase in diameter, causing retention loss.33
The wear tracks on the O-ring were detected on the rubber matrix as well as on the titanium patrix at the maximum convexity, which is the primary frictional contact area. This phenomenon, of parallel wear in rubber and metal, can be partially explained by the chemical reaction that occurs on the surface as a result of wear in the rubber. Specifically, this reaction arises from the direct attack on the metal by the free radicals of rubber generated as a result of the wear process, which is accelerated with the stabilization of the free radicals.34 This result supports the observations of a previous study, that O-rings must be replaced every 6-9 months, depending on the type of the prosthesis, dietary habit, and the degree of ease of insertion and removal.35
EZ lock was subject to slight retention loss after repeated insertion and removal. In particular, it offered a uniform retentive force, outperforming the other two attachment systems. EZ lock is a solitary, resilient type of attachment system which was recently developed in South Korea, characterized by titanium alloy springs and 3 ceramic balls within the housing.
The performance of the EZ lock attachment may be attributed to the excellent resistance of the ceramic balls to frictional wear, compared to the polymer structures of the other attachment systems using nylon (Kerator) or rubber (O-ring). The better performance of the EZ lock could also be because of the lower hardness of the other systems compared to the ceramic and the less intense force exerted by the spring of the EZ lock system. Based on the smaller standard deviation and coefficient of variation of EZ lock, it can be expected to offer more uniform retentive force in the oral environment compared to other systems (which use materials such as plastic, nylon, and rubber). Additional clinical studies must be performed to explore this aspect.
In general, the retention loss of an attachment may be caused by wear, deformation, and fracture of the metal or plastic structures.1920 As demonstrated by the SEM images taken in this study, wear and deformation were markedly manifested in rubber structures than in the metal structures. This result is consistent with the results of other studies, where wear was hardly observed on metal structure surfaces in in vitro tests, in contrast to plastic structures.36 Specifically, no wear was observed in the TiN-coated titanium patrices of Kerator and EZ lock, presumably due to the effect of the TiN-coating, which is known to enhance surface hardness and wear resistance.37 However, the wear in attachments is a complex process that involves adhesive, abrasive, surface fatigue, and corrosive factors, and its mechanism has not been clearly understood; therefore, the arguments presented thus far are based on speculations.38
The results of this study have limitations in explaining the retention loss, dependent on the initial retentive force and duration of use in the oral environment. While the retention loss was observed in the experiment only as a result of mechanically repeated insertion and removal cycles, numerous other factors could influence the retentive force in the real oral environment. Furthermore, the retentive force of a denture can be greatly affected by its functional location, in addition to the number or type of attachment.39 Consequently, further studies would be required to investigate the effects of the implant alignment and angulation, as well as the occlusal load, parafunctional factors, foods, saliva, plaque, and denture cleaners.
Although the limitations of this in vitro study, we concluded that the material and design of attachment are factors that influence the retention loss and wear patterns of the structures. The retention loss of the attachments following repeated insertions and removals, compared to the initial retentive force, may be partially explained by the changes in the surface of the structures, such as wear and deformation. After 2500 insertion and removal cycles, all attachments exhibited significant loss in retention. Especially, the deviation of retention was appeared as large, and deformation and wear were higher in synthetic polymers matrix.
Figures and Tables
 | Fig. 1Custom base mountings fabricated using acrylic resin. (A) Frontal view of the upper and lower mountings. (B) Bottom view of the upper mounting. (C) Top view of the lower mounting with implant fixtures. |
 | Fig. 2Attachment systems used in this study. From left to right: Kerator blue, O-ring red, and EZ lock. |
 | Fig. 6Graphical representation of the percentage retentive force during 2500 insertion and removal cycles. |
 | Fig. 7Images of the matrices obtained by scanning electron microscopy (left: ×30, right: ×180 magnification) of the different attachment systems after 2500 cycles. (A, B) Kerator nylon matrix exhibiting wear changes, especially in the central core. (C, D) O-ring rubber matrix exhibiting deterioration and deformation. (E, F) EZ lock ceramic ball displaying a scratched surface. Boxes in (A, C, and E) correspond to (B, D, and F), respectively. |
 | Fig. 8Images of the patrices obtained by scanning electron microscopy (left: ×25, right: ×35 magnification) of the different attachment systems, after 2500 cycles. (A, B) Kerator titanium nitride-coated cylindrical patrix showed an absence of detectable wear. (C, D) O-ring uncoated titanium ball patrix exhibiting wear tracks (arrow). (E, F) The EZ lock titanium nitride-coated ball patrix also displayed absence of detectable wear. |
Table 1
Characteristics of the attachment systems investigated in this study

Table 2
Mean, standard deviation (SD), and coefficient of variation (CV) of retentive force and retention loss in each group

References
1. Gunne HS, Bergman B, Enbom L, Högström J. Masticatory efficiency of complete denture patients. A clinical examination of potential changes at the transition from old to new denture. Acta Odontol Scand. 1982; 40:289–297.
2. Bergman B, Carlsson GE. Clinical long-term study of complete denture wearers. J Prosthet Dent. 1985; 53:56–61.
3. van Waas MA. The influence of clinical variables on patients' satisfaction with complete dentures. J Prosthet Dent. 1990; 63:307–310.
4. Zitzmann NU, Marinello CP. A review of clinical and technical considerations for fixed and removable implant prostheses in the edentulous mandible. Int J Prosthodont. 2002; 15:65–72.
5. Adell R, Eriksson B, Lekholm U, Brånemark PI, Jemt T. Long-term follow-up study of osseointegrated implants in the treatment of totally edentulous jaws. Int J Oral Maxillofac Implants. 1990; 5:347–359.
6. Albrektsson T, Zarb G, Worthington P, Eriksson AR. The long-term efficacy of currently used dental implants: a review and proposed criteria of success. Int J Oral Maxillofac Implants. 1986; 1:11–25.
7. Petropoulos VC, Smith W. Maximum dislodging forces of implant overdenture stud attachments. Int J Oral Maxillofac Implants. 2002; 17:526–535.
8. Misch CE. Contemporary implant dentistry. 2nd ed. Missouri: CV Mosby;1999. p. 67–72.
9. Caldwell CW, Clark AE. Dental implant prosthodontics. Philadelphia: JB Lipponeott Co.;1991. p. 313.
10. Feine JS, Carlsson GE, Awad MA, Chehade A, Duncan WJ, Gizani S, Head T, Lund JP, MacEntee M, Mericske-Stern R, Mojon P, Morais J, Naert I, Payne AG, Penrod J, Stoker GT, Tawse-Smith A, Taylor TD, Thomason JM, Thomson WM, Wismeijer D. The McGill consensus statement on overdentures. Mandibular two-implant overdentures as first choice standard of care for edentulous patients. Montreal, Quebec, May 24-25, 2002. Int J Oral Maxillofac Implants. 2002; 17:601–602.
11. Haraldson T, Jemt T, Stålblad PA, Lekholm U. Oral function in subjects with overdentures supported by osseointegrated implants. Scand J Dent Res. 1988; 96:235–242.
12. Melas F, Marcenes W, Wright PS. Oral health impact on daily performance in patients with implant-stabilized overdentures and patients with conventional complete dentures. Int J Oral Maxillofac Implants. 2001; 16:700–712.
13. Davis DM. Role of implants in the treatment of edentulous patients. Int J Prosthodont. 1990; 3:42–50.
14. Raghoebar GM, Meijer HJ, van't Hof M, Stegenga B, Vissink A. A randomized prospective clinical trial on the effectiveness of three treatment modalities for patients with lower denture problems. A 10 year follow-up study on patient satisfaction. Int J Oral Maxillofac Surg. 2003; 32:498–503.
15. Trakas T, Michalakis K, Kang K, Hirayama H. Attachment systems for implant retained overdentures: a literature review. Implant Dent. 2006; 15:24–34.
16. Naert I, Gizani S, Vuylsteke M, van Steenberghe D. A 5-year randomized clinical trial on the influence of splinted and unsplinted oral implants in the mandibular overdenture therapy. Part I: Peri-implant outcome. Clin Oral Implants Res. 1998; 9:170–177.
17. van Kampen F, Cune M, van der Bilt A, Bosman F. Retention and postinsertion maintenance of bar-clip, ball and magnet attachments in mandibular implant overdenture treatment: an in vivo comparison after 3 months of function. Clin Oral Implants Res. 2003; 14:720–726.
18. Cardoso RC, Gerngross PJ, Dominici JT, Kiat-amnuay S. Survey of currently selected dental implants and restorations by prosthodontists. Int J Oral Maxillofac Implants. 2013; 28:1017–1025.
19. Goodacre CJ, Bernal G, Rungcharassaeng K, Kan JY. Clinical complications with implants and implant prostheses. J Prosthet Dent. 2003; 90:121–132.
20. Walton JN, Ruse ND. In vitro changes in clips and bars used to retain implant overdentures. J Prosthet Dent. 1995; 74:482–486.
21. Besimo CH, Graber G, Flühler M. Retention force changes in implant-supported titanium telescope crowns over long-term use in vitro. J Oral Rehabil. 1996; 23:372–378.
22. Wichmann MG, Kuntze W. Wear behavior of precision attachments. Int J Prosthodont. 1999; 12:409–414.
23. Bayer S, Steinheuser D, Grüner M, Keilig L, Enkling N, Stark H, Mues S. Comparative study of four retentive anchor systems for implant supported overdentures--retention force changes. Gerodontology. 2009; 26:268–272.
24. Alsabeeha NH, Payne AG, Swain MV. Attachment systems for mandibular two-implant overdentures: a review of in vitro investigations on retention and wear features. Int J Prosthodont. 2009; 22:429–440.
25. Sinclair PM, Little RM. Maturation of untreated normal occlusions. Am J Orthod. 1983; 83:114–123.
26. Stephens GJ, di Vitale N, O'Sullivan E, McDonald A. The influence of interimplant divergence on the retention characteristics of locator attachments, a laboratory study. J Prosthodont. 2014; 23:467–475.
27. Lehmann KM, Arnim FV. Studies on the retention forces of snap-on attachments. Quintes Dent Technol. 1978; 7:45–48.
28. Setz I, Lee SH, Engel E. Retention of prefabricated attachments for implant stabilized overdentures in the edentulous mandible: an in vitro study. J Prosthet Dent. 1998; 80:323–329.
29. Pigozzo MN, Mesquita MF, Henriques GE, Vaz LG. The service life of implant-retained overdenture attachment systems. J Prosthet Dent. 2009; 102:74–80.
30. Alsabeeha NH, Swain MV, Payne AG. Clinical performance and material properties of single-implant overdenture attachment systems. Int J Prosthodont. 2011; 24:247–254.
31. Rutkunas V, Mizutani H, Takahashi H, Iwasaki N. Wear simulation effects on overdenture stud attachments. Dent Mater J. 2011; 11. 25.
32. Schallamach A. A theory of dynamic rubber friction. Wear. 1963; 6:375–382.
33. Nagaoka E, Nagayasu Y, Yamashita H, Matsushiro H, Okuno Y. Study of retention in attachments for overdenture. (II) O-ring attachment. J Osaka Univ Dent Sch. 1980; 20:215–226.
34. Gent AN, Pulford CTR. Wear of metal by rubber. J Mater Sci. 1979; 14:1301–1307.
35. Winkler S, Piermatti J, Rothman A, Siamos G. An overview of the O-ring implant overdenture attachment: clinical reports. J Oral Implantol. 2002; 28:82–86.
36. Gamborena JI, Hazelton LR, NaBadalung D, Brudvik J. Retention of ERA direct overdenture attachments before and after fatigue loading. Int J Prosthodont. 1997; 10:123–130.
37. Mezger PR, Creugers NH. Titanium nitride coatings in clinical dentistry. J Dent. 1992; 20:342–344.
38. Halling J. Introduction to Tribology. 5th ed. London: Wykham Publications;1976. p. 63–82.
39. Williams BH, Ochiai KT, Hojo S, Nishimura R, Caputo AA. Retention of maxillary implant overdenture bars of different designs. J Prosthet Dent. 2001; 86:603–607.




 PDF
PDF ePub
ePub Citation
Citation Print
Print





 XML Download
XML Download