MATERIALS AND METHODS
A total of 439 patients with SCC of the tongue were diagnosed and treated in the Department of Oral and Maxillofacial Surgery, Seoul National University Dental Hospital. Patients were treated over a 12.5-year period from January 1, 2001 to June 30, 2013 and were managed by four maxillofacial surgeons specializing in oral cancer, along with their reconstruction teams. Among the 439 diagnosed patients, 211 satisfied the inclusion criteria for this study. These criteria included a pathologic diagnosis of malignancy in the tongue, the availability of clinical information regarding intraoral prosthesis, and panoramic radiograph data revealing the type and location of the prosthesis.
These 211 patients were categorized according to sex, age, position and type of prosthesis, and primary location of the tongue malignancy. This study protocol was fully approved by the Institutional Review Board of Seoul National University Dental Hospital. Most patients exhibited advanced stage III or IV cancer and received a radical, combined-modality treatment regimen consisting of chemotherapy, surgery, and/or radiotherapy. Patients' clinical and demographic information, such as age, sex, tobacco history, previous cancer therapy, specific primary site in the tongue, histological diagnosis, and tumor staging data, including T (tumor size), N (nodal), and M (metastatic) staging, were collected.
A thorough dental history was reviewed for each patient. This history included the frequency and presence of prosthesis, such as fixed or partial dentures. The inclusion criteria for this study were as follows: (1) diagnosed with both clinical and pathological malignancy of the tongue; (2) available clinical information regarding dentition and previous treatment; (3) available panoramic radiographs for identifying the types and locations of the prostheses. Exclusion criteria included: (1) diagnosed with clinical or pathological malignancy of the tongue; and (2) insufficient clinical and panoramic information for identifying the type and location of prosthesis.
Patients were categorized according to the following variables:
(1) Sex
(2) Age (0-19 years, 20-29 years, 30-39 years, 40-49 years, 50-59 years, 60-69 years , and older than 70 years)
-
(3) Position of crown and/or bridge (Fig. 1)
Group 0: no crown or bridge
Group 1: right molar area (from the right first premolar to the right third molar)
Group 2: anterior teeth area (from the right canine to the left canine)
Group 3: left molar area (from the left first premolar to the left third molar)
Group 4: bilateral molar area
Group 5: right molar and anterior teeth areas
Group 6: anterior teeth and left molar areas
Group 7: right molar, anterior teeth and left molar areas
(4) Position of dentures (maxilla, mandible, or both)
(5) Location of SCC of the tongue [right border (type a), left border (type b), bilateral borders (type c), and other location (type d)14]
Univariate analyses were performed using the Pearson Chi-square test, Student's t-test, and one-way analysis of variance in SPSS for Windows, version 12. Analyses were performed in two different ways, frequency analysis and cross analysis. P values less than 0.05 were considered to be statistically significant. Frequency analysis was conducted to determine the relationships of SCC of the tongue with patient sex, age, location, type of prosthesis (crown and/or bridge), and prosthesis position. Cross analysis was also conducted to analyze possible relationships between the location of the SCC of the tongue and the presence of a crown and/or a bridge, the position of each prosthesis, and the presence of other removable dentures.
RESULTS
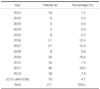
Among the 439 patients initially identified, 62 lacked sufficient clinical information for inclusion, and 166 patients were not diagnosed with a tongue lesion that was both clinically and pathologically malignant; thus, these 228 patients were excluded. The data from the remaining 211 patients, including their panoramic radiographs, clinical chart records, and pathological diagnoses, were reviewed and compared. Frequency analyses of these data are shown in
Table 1.
Of the 211 patients included in the study, 80 (37.9%) were female and 131 (62.1%) were male. The mean patient age was 54.9 years; the age bracket with the most patients was 50-59 years (60 patients, 28.4%), followed by 60-69 years (40 patients, 19.0%), 70 years and above (40 patients, 19.0%), 40-49 years (33 patients, 15.6%), 30-39 years (27 patients, 12.8%), and less than 20 years (11 patients, 5.2%). Regarding the location of SCC of the tongue, 104 patients (49.3%) had a lesion located on the right lateral border of the tongue, and 93 patients (44.1%) had a lesion on the left lateral border (
Table 2). The distribution of prostheses included 134 patients (63.5%) with at least one prosthesis and 77 patients (36.5%) without a prosthesis; this difference was statistically significant (
P<.05). Fewer patients had a crown (91, 43.1%) than did not have a crown (120, 56.9%); similarly, fewer patients had a bridge (99, 46.9%) than did not have a bridge (112, 53.1%). The number of patients with both a crown and a bridge was 56 (41.8%) (
Table 3).
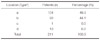
Regarding the position of the crown and/or the bridge, group 7 had the most patients (43, 20.4%) followed by group 4 (33, 15.6%), and group 1 (19, 9.0%); regarding the location of the crown, group 1 had the most patients (29, 13.7%) followed by group 4 (21, 10.0%); regarding the location of the bridge, each group showed similar frequencies except group 7 (31, 14.7%) (
Table 4). Of the patients included in the study, 73 (34.6%) wore dentures; 47 of those had both upper and lower dentures, a 22.3% overall frequency (
Table 5).
Cross analysis was performed to investigate possible relationships between the location of the lesion and the presence of a prosthesis (
Table 6), the location of the lesion and the position of the crown and/or bridge (
Table 7), the location of the lesion and the presence of a prosthesis (
Table 8), and the location of the lesion and the position of dentures (
Table 9). No significant relationship was observed between the presence of a prosthesis and the location of the lesion (
P=.723); thus, it is still unclear why patients with a crown and/or bridge have more frequent SCC of the tongue compared with patients without prostheses. Moreover, no significant association was observed between the presence of a crown and/or bridge and the location of the lesion (
P=.230), the presence of a crown alone and the location of the lesion, or the presence of a bridge alone and the location of the lesion (
P=.674 and 0.066, respectively). Regarding the position of a prosthesis, no significant relationship was observed between the position of a crown and location of the lesion (
P=.071) or between the position of a bridge and location of the lesion (
P=.716). Similarly, the location of the lesion was not significantly associated with the presence of dentures (
P=.409), and the position of dentures was not associated with location of the lesion (
P=.073).
DISCUSSION
Oral SCC is commonly observed in the tongue, lip, gingival tissue, palate, and floor of the mouth.
15 SCC of the buccal mucosa is common among Asian populations due to cultural betel quid and tobacco chewing habits; for instance, 40% of all oral cancers in Sri Lanka are found on the buccal mucosa.
1,
9
The tongue is the most common site of oral cancer among European and US populations and accounts for 40-50% of all oral cancers.
1,
15 Many contributing factors of SCC of the tongue have been identified, and SCC of the tongue is believed to be a multifactorial condition.
9,
16 Alcohol and tobacco have been hypothesized to exert their carcinogenic effects via a contact mechanism; for example, tobacco smoking is more strongly associated with tongue cancer when patients have been heavily exposed to inhaled smoke. On the other hand, alcohol consumption exerts a stronger effect on structures belonging to the food channel and reservoir systems, such as the tongue. This explanation is consistent with studies in animal models that have investigated the effect of ethanol on the mucosal penetration of nitrosonornicotine in the oral mucosa. The detection of DNA from HPV subtypes 6 and 16 in exfoliated oral cavity cells has been shown to be strongly associated with an elevated risk for tongue cancer; moreover, DNA-based studies of HPV isolates found in exfoliated oral tissue from case subjects showed that HPV types 16, 18, 31, 33, and 35 were the most common. However, a definitive association between tongue cancer risk and the detection of high-risk HPV types has not yet been proven.
1,
15,
16
This study was conducted to identify contributing factors in tongue cancer. The patients in this study exhibited a similar clinical/demographic distribution, including sex, age, and primary tumor site of the tongue, as has been observed in other studies of oral cancer patients. Of the patients in the study, 62.1% were male and 28.4% were female, the mean patient age was 54.9 years, and patients aged 50-59 years old were the most prevalent. No suitable studies were available against which to compare the presence and locations of intraoral prostheses. This study did have a few disadvantages; for example, the duration of the intraoral prosthesis was not included, the study did not examine whether patients received prosthetic treatment by professionals, and the study did not examine marginal adaptation to the prosthesis. Additionally, the raw materials of the dental prostheses were not examined in this study. To fully investigate the possible relationships between dental prosthesis and SCC of the tongue, more extensive data need to be obtained from patients with SCC of the tongue, and prospective studies focusing on the physical properties of these prostheses and their biochemical influences on the tongue should be performed.
Cross analysis did not reveal any significant association between location of the prosthesis and SCC of the tongue. However, the number of patients with a crown and/or a bridge (134, 63.5%) was significantly different from the number of patients without prosthesis (77, 36.5%). These retrospective findings suggest that any prosthetic margin, crown surface, or bridge surface is capable of inflicting mechanical irritation on the tongue, and that these irritations may contribute to the development of SCC of the tongue. People who wear dentures are known to have a higher prevalence of oral mucosal lesions compared with people who do not wear dentures, crowns, or bridges; these oral mucosal lesions can develop into malignancies in the oral cavity. Among people who wear dentures, those who wear complete dentures have been shown to have a higher incidence of lesions compared with people who wear partial dentures.
17 Oral cancer can also be observed in the contact area between the teeth and the prosthesis; in particular, tongue malignancies of the lateral border have been observed opposite from the flange extension of the lower denture.
18 Another related study found that metallurgically-flawed gold crowns contribute to SCC of the tongue.
19
However, these findings are controversial. Other studies have found no correlation between denture wearing and oral malignancies,
20 denture type and oral mucosal lesions, or the use of dentures and SCC of the tongue.
21,
22 Lockhart et al.
18 observed 28 intraoral malignancies in the contact area of either the teeth or prosthetic appliances; moreover, all 10 patients with SCC of the tongue were associated with a flange extension of a lower denture. Kinnebrew et al.
19 reviewed a case of a 25-year-old woman with SCC of the tongue and concluded that the lesion was physically associated with a metallurgically-flawed gold crown that had been used for 15 years. However, Albuquerque et al.
22 concluded that dentures are not an etiologic factor for SCC of the tongue, since no definitive association between SCC of the tongue and denture use was demonstrated. Furthermore, Jainkittivong et al.
17 reported that no association was found between pathologic conditions of the intraoral mucous membrane and denture type.
Physical trauma has been proposed to act as a contributing factor that could determine the location of oral cancer, which may explain a possible relationship between trauma and cancer location. Inflammatory reactions in the oral cavity induced by either dental trauma or physical irritation have been considered to be important contributing factors for oral cancer. In support of this hypothesis, inflammatory changes in the thin atrophic mucous membrane have been observed.
23 Many other possible relationships have been proposed, but these relationships have not yet been confirmed.
Chronic trauma is frequently found in people who wear dentures, and other pathological conditions associated with the use of dentures such as Candida-induced denture stomatitis, denture-related hyperplasia, angular cheilitis, and traumatic ulcers are known to be related to SCC of the tongue. Unfortunately, this retrospective study did not investigate the presence of premalignant lesions in the patients. However, ulcerations of the tongue caused by chronic trauma resulting from poorly fabricated dentures, fractured restorations, sharp edges on worn teeth, and ill-fitting crowns and/or bridges were confirmed in most cases. The tongue mucosa is thought to be more permeable to noxious substances and therefore more vulnerable to external carcinogens. Moreover, the mucosal epithelium of the tongue becomes thinner with age, and the rate of collagen synthesis by connective tissue also decreases.
Regarding trauma, chronic irritations caused by ill-fitted dentures, fractured restorations, and other erosive factors can alter the tongue mucosa. Together with other factors such as alcohol and tobacco, these factors may lead to the development of oral cancer. Some studies have reported that SCC in the anterior two-thirds of the tongue is often accompanied by local traumatic irritation. Clearly, many people with years of chronic mucosal irritation from a dental or prosthetic source do not develop cancer. However, our study suggests that, of the people who do develop cancer, a high percentage of these cancers will arise in areas that are in direct contact with teeth and appliances. Neither this study investigate the quality of the prostheses such as marginal discrepancy of crown, the duration of prostheses, or quality of occlusion, and no significant differences were observed between the position of the prosthesis and the location of the SCC of the tongue. These results may only support the hypothesis that mechanical trauma is the cause of SCC of the tongue.
One of the possible precancerous conditions for SCC is leukoplakia.
24 Earlier studies have indicated that oral galvanism is a contributing factor for oral leukoplakia, and that the removal of the metal prosthesis resulted in the resolution of the leukiplakia.
25 Oral galvanism can be generated by the presence of more than two adjacent metal prostheses, which can introduce current flow.
26 The intraoral electrical phenomenon of galvanism could increase the proliferation of leukoplakia cells, induce apoptosis, and simulate some morphological features of SCC. This galvanic current, which affects ornithine decarboxylase, is upregulated in many cancers, which is important because the Na
+K
+-ATPase acts as an ion transporter.
25
Electrical actions from prosthetic metal materials of crowns and/or bridges should be considered an important etiologic factor of SCC of the tongue. Although the currents generated are minute, they can form a type of weak battery. Over time, this electrical battery can result in irritating injury to the tongue mucosa and the surrounding muscles.
Galvanic current is a type of miniature battery formed by electric circuits resulting from the presence of dissimilar metals in the mouth. Prosthetic metals, such as gold, silver, copper, and mercury, show different electrical potentials in the aqueous saliva of the oral cavity. Thus, if two dissimilar prostheses are placed in the mouth, a simple galvanic battery, called an electromotive series, will be formed.
26 As the tongue moves, the positions of the two metals (one above and the other below, one on the left and the other on the right, or one in an anterior location and the other in a posterior location) constitute a new electrolyte, resulting in peculiar taste perceptions. If these metals are connected externally, electric current flows from one metal to another by means of an external conductor circuit. The mobile tongue mucosa is a good conductor, and saliva can be considered a solution composed of several electrolytes. Therefore, prosthetic metal, when it is bathed in saliva and placed near a tongue conductor, forms a simple galvanic battery in the oral cavity.
This electrical action of prosthetic metals has been proposed to be one of the main contributing factors to SCC of the tongue. Three different aspects - galvanometer measurement, local action, and polarization - have been proposed as mechanisms through which the electrical actions contribute to SCC of the tongue.
26
Firstly, galvanometer measurements of metals in situ have been shown to have a relationship with some accompanying pathologic changes. An oral cavity with more than one metallic restoration can conduct currents ranging as high as 80 microamperes, with the exception of an oral cavity containing only fillings of 24-carat gold. The value of the current dropped within five seconds to a steady minimum, which was approximately 10% of the initial value, when the contactors were held in place for an appreciable length of time. Both high and low values were obtained in oral cavities with pathologic lesions; these values were not significantly different from those obtained in mouths with no untoward symptoms. Subsurface porosity in the vicinity of the discoloration, accompanied by a thin, silvery surface layer of gold, was found in the metallurgic study. Peaks of copper, gold, silver, and palladium were also examined in the interior and on the surface of a crown. The elements identified on the discolored surface of the crown were copper, silicon, chlorine, silver, and gold. However, much more silver and much less gold were identified on the discolored surface compared with the interior of the crown. The discolored surface of the crown was found to be high in silver solder (AgCu) or to contain gold solder with a high silver content. The resultant corrosion products of silver, revealed by the chlorine and silver peaks, suggest that electrogalvanism had occurred. This electrogalvanism promotes chronic galvanism.
The second relevant finding is that metal alloys have local actions and induce pathological changes. Copper and gold alloys are physical mixtures of separate and distinct crystals. When these crystals coexist on the surface of a restoration, potential differences will exist between the crystals and the saliva, thereby constituting a miniature galvanic cell. In this instance, the external circuit is the restoration itself, and the internal circuit is completed by the saliva and related soft tissues. Any white mucosal lesions, such as leukoplakia, can be produced by this local action effect. Similar to the manner in which nickel dermatitis can be caused by wrist watches and spectacle frames, the nickel found in white gold alloys has an electrolytic battery action when it is in contact with dissimilar metals and an acid or an alkaline fluid. When an electrolyte perspirates and acts upon the base, metal salts are formed. Moreover, such action is more pronounced in the presence of heat. Nickel salts cause irritations where the metal comes in contact with the skin.
The third important finding related to galvanic currents is that of polarization. Polarization is present in the oral cavity immediately after restorations are inserted and is manifested by a reduction in the normal current. This polarization phenomenon is also known to cause a metallic taste, which is noticeable immediately after the insertion of a restoration and disappears shortly afterward. The presence of continuous or intermittent depolarizing agents can permit current to flow, resulting in damage to the tongue mucosa. These lesions can be traced to electrical causes; however, galvanometer readings bear no relation to the normal current flow in these cases. Moreover, current does not normally flow between restorations; this observation is consistent with the resistance of metals to wear. Electrical energy is produced at the expense of one of the electrodes in an ordinary battery. If currents on the order of those of a normal battery were flowing between restorations, some of the restorations would be eroded over the course of several years.
25,
26
Among the present patients with SCC of the tongue, 63.5% more had a crown or a bridge compared with the number of patients without prosthesis. We investigated the cause of this difference but did not find any significant association between these prostheses and location of the lesion (P=.723). However, the precise relationship between dental prostheses and SCC of the tongue remains controversial. We did not classify dental materials used in prostheses in this study. Therefore, we could not conclude that prostheses and galvanic phenomena play a major role in the etiology of SCC of the tongue. Also, the biochemical effects of oral prostheses and their contributions to SCC of the tongue need to be addressed in future studies.
Finally, early diagnosis remains a key element for adequate therapy of oral SCC, including SCC of the tongue. Clinicians should be aware that single ulcers, tumors, red plaques, or white plaques, particularly if any of these persist for more than two weeks, may be manifestations of malignancy. In these cases, a prompt biopsy of the suspicious lesion should be performed.
27 Moreover, the entire oral cavity, including the tongue, should be routinely examined in all patients with any prostheses.




 PDF
PDF ePub
ePub Citation
Citation Print
Print










 XML Download
XML Download