Abstract
PURPOSE
The purpose of this study was to compare removal torques and surface topography between laser treated and sandblasted, large-grit, acid-etched (SLA) treated implants.
MATERIALS AND METHODS
Laser-treated implants (experimental group) and SLA-treated implants (control group) 8 mm in length and 3.4 mm in diameter were inserted into both sides of the tibiae of 12 rabbits. Surface analysis was accomplished using a field emission scanning electron microscope (FE-SEM; Hitachi S-4800; Japan) under ×25, ×150 and ×1,000 magnification. Surface components were analyzed using energy dispersive spectroscopy (EDS). Rabbits were sacrificed after a 6-week healing period. The removal torque was measured using the MGT-12 digital torque meter (Mark-10 Co., Copiague, NY, USA).
RESULTS
In the experimental group, the surface analysis showed uniform porous structures under ×25, ×150 and ×1,000 magnification. Pore sizes in the experimental group were 20-40 mm and consisted of numerous small pores, whereas pore sizes in the control group were 0.5-2.0 mm. EDS analysis showed no significant difference between the two groups. The mean removal torque in the laser-treated and the SLA-treated implant groups were 79.4 Ncm (SD = 20.4; range 34.6-104.3 Ncm) and 52.7 Ncm (SD = 17.2; range 18.7-73.8 Ncm), respectively. The removal torque in the laser-treated surface implant group was significantly higher than that in the control group (P=.004).
A variety of implant systems have been developed and adopted over time, and several systems have been improved by the addition of distinctive features. Each system has its own advantages and disadvantages. Implant systems have been changing continuously to accommodate patients' needs. Various methods of successful implantation for osseointegration have been proposed. Proper design, material, surface treatment, surgical method, host site and leading conditions1,2 have all been the parameters of focus in research on successful implant systems.
The present study was undertaken to compare implant osseointegration according to the surface treatment method applied. The surface structure of the implant influences bone reaction more than any other factor.3 Therefore, previous research focused on increasing the host's osteoinduction and biological adaptation. Multiple surface treatments have been proposed for increasing the success rate of osseointegration, the amount and quality of bone at the implant-bone interface.4,5,6,7,8
There are many methods for treating the surface of an implant. The typical method is to spray it with a titanium plasma hydroxyapatite (HA) coating, Al2O3, or TiO2, at the first stage. Afterward, surface roughness is formed by an HCl/H2SO4-like acid. This is known as the sandblasted, large-grit, acid-etched (SLA) method. The resorbable blasting media method is used to form surface roughness by spraying biologically friendly media such as Al2O3, TiO2 and HA.9 Because of its density, MgO is known to be an influential factor on the bone's reaction to an implant.10
SLA creates two types of microscopic rough surfaces: macro and micro. Macro surfaces are formed by sandblasting and can obtain an ideal stability between bones. Micro surfaces are formed by acid etching and can promote cell activity. Thus, SLA has beneficial effects on bone and biocompatibility.9
It has been reported that an SLA surface has good biocompatibility and forms better-quality bone.11,12,13,14 Recent research has shown that altering the implant surface using a laser method (i.e., laser-etched implant, LEI) helps to increase the osseointegration rate.15 This type of surface has also been found to have its own unique surface form. The laser surface blocks contamination of extraneous factors and has a high level of surface purity, resulting in customized surface roughness. The laser-treated surface maintains a pure, non-contaminated surface with porosity structures forming over the entire surface. This porosity structure increases the roughness of the surface, which increases the strength of osseointegration.16,17
There is a substantial amount of research comparing these previously available surface treatments discussed above, but no study has directly compared SLA and laser surface treatment. Therefore, our aim in the present research was to compare SLA-treated and laser-treated implant surfaces.
The experimental implant was manufactured with the laser surface treatment method. The control implant was an SLA implant (Super-line, Dentium, Seoul, Korea). Both implants were made with the same diameter and design (∅ 3.4 mm × 8.0 mm)(Fig. 1).
The experimental implant surfaces were treated with glass fiber in an Nd:YAG laser (Jenoptic AG, Jena, Germany) with linear motion. Machined titanium implant surfaces were treated with an Nd:YAG laser with a 15 kHz wavelength, 10 W rated output, and pulse width of 2 µsec.
Glass fiber illuminant in the most accurate focus was irradiated onto the surface of the implants in a contactless manner. The focus size was 400 mm in diameter. Every surface was uniformly treated. The speed of implant rotation corresponded to the speed of illuminant from the intermittent laser.
We performed field emission scanning electron microscopy (SEM), whereby the film was examined using a scanning electron microscope (S-4800, Hitachi, Tokyo, Japan). SEM was used to observe surfaces of both the experimental and control groups under ×25, ×150 and ×1,000 magnifications. Analyses of surface elements and components were conducted using energy dispersive spectroscopy (EDS, Horiba, Kyoto, Japan).
A total of 12 adult New Zealand white rabbits (experimental animal) were used for this experiment. The mean weight of the rabbits was approximately 3.0 kg before the first surgery. Each implant was inserted into both sides of the rabbit tibiae. Six weeks after the installation surgery, the removal torque rate was measured with a torque meter.
Approval for this study was obtained from the committee of animal ethics (approval number: KNU 2011-51). Two milliliters of tiletamine/zolazepam (Zoletil50, Virbac Korea, Seoul, Korea) per kg and 5 mg of xylazine (Rompun, Bayer Korea, Seoul, Korea) per kg were injected into the muscles. Right before the surgery, 2% lidocaine (Yuhan Corporation, Seoul, Korea) was injected under the skin for local anesthesia.
Before the surgical procedures, fur was removed on the distal side of the tibia and the skin was cleaned with a blended solution of iodine and 75% ethanol. After tissue incision, the epiphysis area of the tibia was exposed. In the experimental group, an implant with a laser-treated surface was inserted into the right tibia, and in the control group, an implant with an SLA-treated surface was inserted into the left tibia. The implant protocol was conducted according to the manufacturer's instructions. A cover screw was used following implant installation. Suturing was done using 4-0 vicryl sutures.
After the surgery, rabbits were given sufficient healing time while isolated in a proper environment for 24 hours to recover fully.
For 3 days, 0.3 mL each of methampyrone (Novin-50, Bayer Korea, Seoul, Korea) and butaphosphan (Catosal, Bayer Korea, Seoul, Korea) were injected intramuscularly. Six weeks after the surgery, rabbits were sacrificed and measurements were performed.
The bone responses were estimated using a removal torque test.18 The removal torque was measured by the maximum shear stress (Ncm) of the surfaces between the bone and implant. After sacrifice, the skin of the 10 rabbits was incised and the soft tissue was elevated. The cover screws were removed to measure the removal torque. A digitally operated torque gauge MGT-12 (Mark-10 Corporation, New York, NY, USA) coupled with a specially devised connector measured the maximum shear stress causing bone fracture of the bone and implant interface.
CT scanning was conducted after each removal torque test to visualize the connection between the implant and cortical bone. Results were evaluated with all samples, which were confirmed to have been implanted bi-cortically after scanning with micro-CT. Samples were prepared by making an 8-mm cut per rabbit on the major axis of the tibia (Fig. 2). A micro CT (X-EYE 3000, SEC, Suwon, Korea) with a 160 kvp anode voltages and 200 mm alternating voltage was used. Results were obtained using the HARMONY program (DRGEM, Gwangmyeong, Korea) and icat3D program (Mevisys, Daejeon, Korea).
The removal torque rate was statistically analyzed with the Mann-Whitney U test (SPSS statistic 17.0, IBM Co., Chicago, IL, USA). Values are shown as means and standard deviations. The level of significance was P≤.05.
The experimental group (Fig. 3A) observed more roughened surface than the control group (Fig. 3B). Therefore, the experimental group (Fig. 3C) showed significant amount of rods and cones. The control group (Fig. 3D) showed porous structure. The pore sizes of experimental group (Fig. 3E and Fig. 3G) ranged from 24-40 mm, however that of the control group (Fig. 3F and Fig. 3H) was 0.5-2.0 mm.
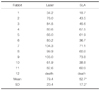
In the EDS analysis, Ti, O and C were the only three elements found in the laser-treated implant surfaces. Ti and C were found in SLA-treated implant surfaces (Fig. 4 and Fig. 5; Table 1 and Table 2).
Removal torques were measured 6 weeks after the surgery (Table 3).
In the experimental group, the mean torque value of the laser-treated implant surface was 79.4 Ncm (SD = 20.4; range: 34.6-104.3 Ncm). In the control group, the mean torque value of the SLA-treated surface implant was 52.7 Ncm (SD = 17.2; range: 18.7-73.8 Ncm). The removal torque of the laser-treated implant surfaces was significantly higher than that of the SLA-treated implant surfaces (P=.004).
All samples were confirmed to have been implanted bicortically after scanning with micro-CT (Fig. 6).
The result of this study is consistent with the other study.15 In rabbit experiments, it was concluded that the maximum removal torque rate increased significantly in laser-treated implant surfaces.15
The reason why laser-treated implant surface showed higher RTQ could be explained as follows : According to bone to implant contact from the micro-CT exam of this study (Fig. 6). The contact length between fixture and bone were 10.92 mm at the experimental group and 6.75 mm at the control group is the fixture body. These are the median values among eleven specimens in each group, the large difference (10.92 + 0.62 vs 6.75 + 0.71) in the bone-implant contact between two groups can influence the removal torque results (Fig. 6).
The surface observations shown in Fig. 4 using field emission SEM highlights the differences between the surface areas of the two implants. The laser-treated implant surface had regular porosity structures approximately 40 mm in size over the entire surface. These structures have microscopic porosity features that play an important role in widening the external surface area. By contrast, the SLA-treated implant surface had only 0.5-2.0 mm porosity structures over the entire surface and there was no microscopic porosity feature. It means that SLA treatment has less effect on increasing the surface area than does laser treatment.
The EDS analysis showed that Ti, O and C were the only three elements found in laser-treated implant surfaces. Ti and C were found in SLA-treated implant surfaces (Table 1, Fig. 4), it means laser surface could have thicken oxide layer than that of SLA surface. According to the result of EDS analysis of this (Fig. 4 and Fig. 5; Table 1 and Table 2) showed more oxide at laser-treated surfaces than the SLA-treated surfaces. Because 26.17% oxygen ratio mean that there are thick oxide layer were found at the surface the role.
According to a recent study which focused on nanotomograpy or nano-scale geometry,19 there are peak and valley shapes on the threads of the implant, and only the valleys, but not the peaks, were laser-treated in previous research.These researchers19 proposed that untreated structures at the peaks provide better resistance against plaque attacks and peri-implantitis. Indeed, various studies of laser-treated metal or implant surfaces found improved osseointegration. However, further research will be needed to apply laser treatment methods at the nano-scale.
Titanium surface contamination is an important factor affecting mechanical stability and osteoinduction ability.20,21 There is also a possibility of surface contamination by extraneous factors during the manufacturing process. A laser-treated surface can block contamination by extraneous factors, and has a high level of surface purity, resulting in customized surface roughness.16
According to Sennerby's study,22 a healing period of 6-week is sufficient to replace immature bone with lamellar bone. In the area of the tibia with a lot of compact bone, the removal torque value remained unchanged after 6 weeks, which established the appropriate healing time for rabbits at 6 weeks.22 In addition, in a recent study, laser-treated surfaces with acid-etched surfaces showed significant change over an experimental period of 4 weeks.23 Therefore, for the future research, an experiment period of 4 weeks could be planned for the evaluation of the early loading effect of laser-treated surface.
Laser-treated implant surfaces had regular porosity structures, that plays an important role in widening the external surface area. After evaluating the removal torque rate after 6 weeks, the removal torque comparison showed that the removal torque of laser-treated implant surfaces was significantly higher than that of SLA-treated implant surfaces (P=.0041)
Figures and Tables
Fig. 3
Experimental and control group implant images obtained by field emission SEM: (A) Experimental group (×25); (B) control group (×25); (C) experimental group (×150); (D) control group (×150); (E) experimental group (×1,000); (F) control group (×1,000); (G) experimental group (×1,000); (H) control group (×1,000).

Fig. 6
Micro-CT three-dimensional images using the AutoCAD 2011 (Autodesk, San Rafael, CA, USA). (A) Experimental; (B) control. The experimental group was observed 10.92 mm, 0.62 mm. The control group was observed 6.75 mm, 0.71 mm. These images were selected to present contact layer of laser-treated surface as it is not the average but the median value.

References
1. Albrektsson T, Brånemark PI, Hansson HA, Lindström J. Osseointegrated titanium implants. Requirements for ensuring a long-lasting, direct bone-to-implant anchorage in man. Acta Orthop Scand. 1981; 52:155–170.
2. Roberts WE. Fundamental principles of bone physiology, metabolism and loading. In : Naert I, van Steengerghe D, Worthington P, editors. Osseointegration in oral rehabilitation. Carol Stream, IL: Quintessence;1993. p. 163–164.
3. Carlsson L, Röstlund T, Albrektsson B, Albrektsson T. Removal torques for polished and rough titanium implants. Int J Oral Maxillofac Implants. 1988; 3:21–24.
4. Gotfredsen K, Nimb L, Hjörting-Hansen E, Jensen JS, Holmén A. Histomorphometric and removal torque analysis for TiO2-blasted titanium implants. An experimental study on dogs. Clin Oral Implants Res. 1992; 3:77–84.
5. Cordioli G, Majzoub Z, Piattelli A, Scarano A. Removal torque and histomorphometric investigation of 4 different titanium surfaces: an experimental study in the rabbit tibia. Int J Oral Maxillofac Implants. 2000; 15:668–674.
6. Klokkevold PR, Nishimura RD, Adachi M, Caputo A. Osseointegration enhanced by chemical etching of the titanium surface. A torque removal study in the rabbit. Clin Oral Implants Res. 1997; 8:442–447.
7. Wennerberg A, Albrektsson T, Andersson B, Krol JJ. A histomorphometric and removal torque study of screw-shaped titanium implants with three different surface topographies. Clin Oral Implants Res. 1995; 6:24–30.
8. Ferguson SJ, Langhoff JD, Voelter K, von Rechenberg B, Scharnweber D, Bierbaum S, Schnabelrauch M, Kautz AR, Frauchiger VM, Mueller TL, van Lenthe GH, Schlottig F. Biomechanical comparison of different surface modifications for dental implants. Int J Oral Maxillofac Implants. 2008; 23:1037–1046.
9. Marin C, Bonfante EA, Granato R, Suzuki M, Granjeiro JM, Coelho PG. The effect of alterations on resorbable blasting media processed implant surfaces on early bone healing: a study in rabbits. Implant Dent. 2011; 20:167–177.
10. Kang SH, Cho SA. Comparison of removal torques for lasertreated titanium implants with anodized implants. J Craniofac Surg. 2011; 22:1491–1495.
11. Hofmann AA, Bloebaum RD, Bachus KN. Progression of human bone ingrowth into porous-coated implants. Rate of bone ingrowth in humans. Acta Orthop Scand. 1997; 68:161–166.
12. Hall J, Miranda-Burgos P, Sennerby L. Stimulation of directed bone growth at oxidized titanium implants by macroscopic grooves: an in vivo study. Clin Implant Dent Relat Res. 2005; 7:S76–S82.
13. Mangano C, Perrotti V, Iezzi G, Scarano A, Mangano F, Piattelli A. Bone response to modified titanium surface implants in nonhuman primates (Papio ursinus) and humans: histological evaluation. J Oral Implantol. 2008; 34:17–24.
14. Schwartz Z, Martin JY, Dean DD, Simpson J, Cochran DL, Boyan BD. Effect of titanium surface roughness on chondrocyte proliferation, matrix production, and differentiation depends on the state of cell maturation. J Biomed Mater Res. 1996; 30:145–155.
15. Hallgren C, Reimers H, Chakarov D, Gold J, Wennerberg A. An in vivo study of bone response to implants topographically modified by laser micromachining. Biomaterials. 2003; 24:701–710.
16. Gaggl A, Schultes G, Müller WD, Kärcher H. Scanning electron microscopical analysis of laser-treated titanium implant surfaces--a comparative study. Biomaterials. 2000; 21:1067–1073.
17. Cho SA, Jung SK. A removal torque of the laser-treated titanium implants in rabbit tibia. Biomaterials. 2003; 24:4859–4863.
18. Kang SH, Cho SA. Comparison of removal torques for lasertreated titanium implants with anodized implants. J Craniofac Surg. 2011; 22:1491–1495.
19. Palmquist A, Emanuelsson L, Brånemark R, Thomsen P. Biomechanical, histological and ultrastructural analyses of laser micro- and nano-structured titanium implant after 6 months in rabbit. J Biomed Mater Res B Appl Biomater. 2011; 97:289–298.
20. Wie H, Herø H, Solheim T. Hot isostatic pressing-processed hydroxyapatite-coated titanium implants: light microscopic and scanning electron microscopy investigations. Int J Oral Maxillofac Implants. 1998; 13:837–844.
21. Han CH, Johansson CB, Wennerberg A, Albrektsson T. Quantitative and qualitative investigations of surface enlarged titanium and titanium alloy implants. Clin Oral Implants Res. 1998; 9:1–10.
22. Sennerby L, Thomsen P, Ericson LE. Early tissue response to titanium implants inserted in rabbit cortical bone. Part I. Light microscopic obserrvations. J Mater Sci Mater Med. 1993; 4:240–250.
23. Rong M, Zhou L, Gou Z, Zhu A, Zhou D. The early osseointegration of the laser-treated and acid-etched dental implants surface: an experimental study in rabbits. J Mater Sci Mater Med. 2009; 20:1721–1728.




 PDF
PDF ePub
ePub Citation
Citation Print
Print







 XML Download
XML Download