Abstract
PURPOSE
There is insufficient data regarding the durability of porcelain laminate veneers bonded to existing composite fillings. The aim of the present study was to evaluate the fracture resistance and microleakage of porcelain laminate veneers bonded to teeth with existing composite fillings.
MATERIALS AND METHODS
Thirty maxillary central incisors were divided into three groups (for each group, n=10): intact teeth (NP), teeth with class III composite fillings (C3) and teeth with class IV cavities (C4). Porcelain laminate veneers were made using IPS-Empress ceramic and bonded with Panavia F2 resin cement. The microleakage of all of the specimens was tested before and after cyclic loading (1 × 106 cycles, 1.2 Hz). The fracture resistance values (N) were measured using a universal testing machine, and the mode of failure was also examined. The statistical analyses were performed using one-way ANOVA and Tukey post hoc tests (α=.05).
There has been increasing interest in the use of porcelain laminate veneers (PLVs) as esthetic restorations because PLVs combine high esthetic appeal and patient satisfaction with less invasive tooth preparation.1,2 Several studies have reported the promising clinical performance of PLVs. A 10-year prospective clinical observation study reported a survival rate of 92% at 5 years, which dropped to 64% at 10 years.3 The main reasons for failure were large marginal defects and fractures, typically at locations where the enamel was replaced by a large size composite filling or exposed dentin. The researchers also observed recurrent caries, especially in margins that crossed an existing interproximal large composite filling. However, despite the high survival rate, 70% of the patients had previous composite fillings and the size of the fillings was not identified.
Another investigation reported PLV survival rates as high as 94.4% at 5 years, 93.5% at 10 years, and 82.93% at 20 years.4 This study used meticulous inclusion and exclusion criteria for patient selection. However, it did not specify how the preparations were designed in case of dentinal exposure or existing composite fillings. A recent review of studies on the survival of PLVs stressed the importance of the patient selection criteria and preparation design in the outcome.5
Controversies exist regarding the use of PLVs on teeth with small dentinal margins or composite fillings.1,6 In these situations, researchers have suggested that the veneer margin should be extended to the interproximal area to create intraenamel margins.7,8 However, this process compromises excess dental hard tissue. Alternatively, the preparation margins can be terminated on the existing composite, although this approach is thought to increase the development of microleakage and early discoloration.3
Marginal discoloration has been contributed to patient dissatisfaction with PLVs in clinical studies.3,4 It has also been considered to be a proof of a marginal defect, including partial debonding and microleakge.9 In certain circumstances, microleakage could cause fracture or debonding of laminate veneers.3 It has been suggested that the shrinkage of resin cements in the adhesive layer could generate internal stress, causing microcrack formation.10 In this situation, mechanical loading increases the stress level, potentially accelerating crack propagation and restoration fracture.3 In addition, due to the difference in the coefficients of thermal contraction of bonded surfaces, a marginal gap may form after exposure to a thermal shock in the oral environment.8 Furthermore, it has been argued that mechanical loading induces the opening and closing in the existing marginal defect and subsequent fluid percolation. Consequently, degradation of bonded surfaces due to hydrolysis or recurrent caries would be expected, which in turn results in debonding of the laminate veneer.11
However, no significant difference in fracture resistance was found between teeth restored using PLVs with the margins in the composite fillings and teeth with no restorations if all of the composite surfaces were silica-coated and silanized.6 Moreover, a recent study reported the satisfactory short-term clinical performance of teeth restored with PVLs with margins that ended in the composite.12
Considering the abovementioned issues, the aim of the present study was to evaluate the fracture resistance and microleakage of PLVs on teeth with composite fillings after aging. The null hypothesis was that class III and class IV composite fillings would not affect the fracture resistance and microleakage of the teeth restored with PLVs.
The sample size was estimated using the data of a previous study19 and a software (Minitab 13, Minitab Inc., State College, PA, USA). The calculated sample size was 10 for each group in order to detect the minimum difference of 50 N between groups.
Thirty human maxillary central incisors that were recently extracted (within 3 months) due to periodontal problems were selected for the study. Informed consent was obtained from all of the patients according to the protocol of the Clinical Research Ethics Board at Tehran University of Medical Sciences. Only teeth with no caries, cracks, or excessive wear were included in the study. Tissue tags and calculus were removed from teeth with a hand instrument and then stored in a 0.1% chloramine solution for 2 weeks and in distilled water thereafter. To ensure similarity in the dimensions of the teeth, the mesio-distal and inciso-cervical labial surfaces were measured with a digital caliper (Series 500 caliper, Mitutoyo, Kawasaki, Japan) with an accuracy of 0.01 mm. The teeth with measurements within 1 mm of the average were selected.
The teeth were randomly divided into three groups (n=10 for each group): intact teeth with no fillings (NP), teeth with class III cavities (C3) and teeth with class IV cavities (C4). In the C3 group, a III cavity (standard dimensions of 3 × 3 mm), was prepared with a 169L bur (CB23L, D+Z DIAMANT, Berlin, Germany). The incisal margin of each cavity was finished 2.5 mm below the incisal tooth edge to preserve sufficient hard tissue to support the incisal cavity margin. An autopolymerized acrylic resin (Pattern Resin, lot. 1002341, GC America Inc., Alsip, IL, USA) was fabricated in one cavity and used as a template for the remaining cavities. The cavities were etched with 35% phosphoric acid (Etching Gel, Faghihi Dental Co., Tehran, Iran) for 30 seconds, and the teeth were rinsed and gently air-dried. A single-component dentin-bonding agent was applied (Tetric N-Bond, lot. P75516, Ivoclar, Schaan, Lichtenstein) for 30 seconds and light-polymerized for 30 seconds at a light density of 600 mW/cm2 (Coltolux/Whaledent, Cuyahoga Falls, OH, USA) and a distance of 1.0 mm. All of the class III cavities were restored using a microfilled hybrid composite resin (GC Direct, A1, lot. B3001, GC America Inc., Alsip, IL, USA).
In the C4 group, each class IV cavity was prepared by extending the incisal margin of a class III cavity. The rationale for this preparation was based on the recommendations in the literature to remove the existing filling and include the cavity in the final restoration.8,13 The final dimensions of the class IV cavity were set to 3 × 5 mm.
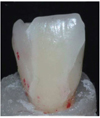
The specimens were stored in water at room temperature for 3 weeks. A silicone mold of each specimen was made (Heavy body, Zhermack, lot.74523, Badia Polesine, Italy) to standardize the preparation and guide the fabrication of the veneers. To create a butt joint, a self-limiting depth-cutting 0.3 mm bur was used to ensure an even intraenamel reduction in the labial surface. The tooth reduction was performed with a round-end tapered diamond bur (868B.314.018, Komet Dental, Lemgo, Germany). The cervical margin ended 1 mm above the cement-enamel junction. In the incisal surface, a butt joint preparation was performed with a 2 mm reduction of the incisal edge and no palatal chamfer (Fig. 1 and Fig. 2). All of the line angles were rounded, and all of the margins were finished. The impressions were made with an additional polyvinyl siloxane impression material (Regular Body, lot. 95503 Elite, Zehrmack, Badia Polesine, Italy) and a custom-made tray (Major Tray, lot 06016A, Major Prodotti Dentori, S.p.A., Moncalieri, Italy) poured with type IV dental stone (Fujirock, GC Corp., Tokyo, Japan). The veneers were fabricated with a heat-pressed all ceramic material (IPS-emax, lot. 69101, Ivocllar/Vivadent, Schaan, Liechtenstein). The pressed models were divested and cleaned. The fitness of the veneers was verified on master dies. The glazing was performed in a conventional porcelain firing furnace (VITA Vaccumat 300, VITA Zahnfabrik H. Rauter GmbH, Bad Sackingen, Germany). The intaglio surface was air-abraded with 50 µ alumina particles at 2-bar pressure at a distance of 10 mm for 5 seconds and cleaned by a sonocleaner (Prosonic 300, Sultan Health Care, Englewood, NJ, USA) with 96% ethanol for 30 seconds. The intaglio surface of the veneers was etched with 9.5% hydrofluoric acid gel (Porcelain Etch, Ultradent Product Inc., South Jordan, UT, USA) for 30 seconds, rinsed thoroughly for 1 minute and silanized (Monobond S, lot. k18374, Vivadent/Ivoclar, Schaan, Liechtenstein) for 1 minute. The teeth were cleaned using a rubber cup and polishing paste. The labial surface of each tooth was conditioned with a self-etch primer (ED Primer, lot. 00262A, Kuraray Co. Ltd., Osaka, Japan). In the C3 group, the composite surface was roughened with a fine-grit diamond bur.
The cementation was performed with an MDP-containing resin cement (Panavia F2, lot. 00168A, Kuraray, Osaka, Japan), according to the manufacturer's instructions. Mixed cement was applied to the intaglio surface of the veneers, and the veneers were positioned on the teeth and held in place with finger pressure. The excess cement was removed, and the laminates were exposed to light on all margins for 60 seconds (Coltolux 50, Coltene/Whaledent, Cuyahoga Falls, OH, USA), while all of the margins were covered with an isolation gel (Oxyguard, Kuraray, Osaka, Japan) to prevent the formation of an oxygen-inhibited layer. The laminates were finished and polished using polishing disks. After storage for 24 hours in distilled water, the specimens were subjected to 5,000 thermal cycles alternating between 5 and 55℃, with a dwelling time of 15 seconds.
Radioisotope and gamma-counting procedures were used to measure the microleakage. A double layer of nail varnish (My, Kahl & Co., Ghazvin, Iran) was painted on the tooth surface to within 1 mm of the laminate margins (Fig. 3). All of the specimens were immersed for 24 hours in 50 cc of a thallium 201 chloride solution (MDS Nordion, Fleurus, Belgium, 1 mCi specific activity). The nail varnish was scratched off the specimen surface with a scalpel, and the teeth were washed for 60 seconds with a liquid detergent material (Prill, Henkel, Saveh, Iran) applied with a swab tip. The specimens were inserted into a specific tube, with care taken to position them identically, and placed in a gamma-counting device (Kontron Gammamatic, Neufahrn, Germany). The radiation was measured with a thallium 201 photon pick of 77 Kev and an energy window of 15% for 60 seconds. To eliminate radioactive contamination, the specimens were kept in a lead-shielded container for 12 days, were then subjected to cycling loading. The periodontal ligament was simulated on the roots of teeth using a polyether elastomer (Impergum F, 3M/ESPE, Seefeld, Germany). The specimens were mounted in a circular jig, angled at 135 degrees, by using an autopolymerizing acrylic resin (Orthoresin, DentsplyDeTrey, Surry, UK). The load contact was adjusted on the cingulum (Fig. 4). The specimens were subjected to 1.2 × 106 cycles of 50 N loads at a frequency of 1.5 Hz to simulate 3 years of service.14 After loading, the specimens were removed from the acrylic block and carefully cleaned. Microleakage was measured again as described above.
The fracture resistance was measured by a universal testing machine (ZwickRoell Z050, Ulm, Germany) with a cross-head speed of 1 mm/min. A load was applied to the incisal edge and measured automatically (Fig. 5). The failure modes of broken laminate were investigated with a stereomicroscope (Zeiss OPM1, Carl Zeiss, Oberkochen, Germany) at a magnification of 20×. Failure was categorized as adhesive failure between the tooth and the laminate, cohesive failure within the laminate or mixed failure.
The homogeneity of variances and normal distribution of the data were verified by Levene's test and the Kolmogorov-Smirnov test, respectively. The mean microleakage values of the groups before and after cyclic loading were statistically analyzed by repeated-measures analysis of variance (ANOVA) using a statistics software (SPSS ver. 13, SPSS Inc., Chicago, IL, USA). The differences in fracture resistance among the groups were compared by one-way ANOVA. The differences with P<.05 were considered statistically significant.
The mean microleakage values of the test groups before and after cyclic loading are shown in Table 1. The maximum microleakage values were found in the class IV group before and after cyclic loading (8.12 × 105 and 8.26 × 105, respectively). The minimum microleakage values were found in the control group before and after cyclic loading (3.48 × 105 and 4.60 × 105, respectively). The mean microleakage values of all of the groups were higher after cyclic loading (P=.039). After cyclic loading, the microleakage values of the class IV and control groups were significantly different from each other (P=.042, Tukey's test, Table 2). The fracture resistance was highest in the control group and lowest in the class IV group (Table 3), but there was no significant difference in the mean fracture resistance between the test groups. All types of failure modes were observed in the test groups (Fig. 6), with no significant difference for any type. Seven of 10 fractures in the class IV group originated from the cavity region.
In the present study, there was no difference in the fracture resistance or microleakage between teeth restored by PLVs with typical class III composite fillings and intact teeth restored by PLVs. Therefore, the null hypothesis was accepted for the class III composite fillings and rejected for the class IV fillings. Some studies have suggested that old composite fillings should be removed before teeth are restored with PLVs.1,13 Removing an old class III composite filling and replacing it with a ceramic veneer would result in a class IV cavity. To test this strategy, the class IV test group was included in the present study.
Although the ideal setting for the experimental study of dental materials and restorations is the oral cavity, clinical trials are time-consuming and not always cost-effective.15,16 To test materials and restorations in vitro, the test conditions should match the oral environment as closely as possible.17 Therefore, thermal cycling and cyclic loading were used in the present study. Human teeth were used in this study because they have unique properties, such as bonding characteristics, elasticity, strength, thermal conductivity, ion transfer in dentinal tubules, and enamel thickness, that influence the results of in vitro investigations.18 However, the use of human teeth also presents some limitations. For example, it is difficult to standardize human teeth based on size and age. For this reason, the teeth which have considerable difference in size were excluded from this study.
Clinical investigations have identified fractures and marginal defects as the main reasons for PLV failure.3,4 Thus, fracture and microleakage were examined in the present study. No significant differences in fracture resistance were found between the test groups with composite fillings and the control group, which is in consistence with the results of Ozcan et al.19 who found no significant difference between the fracture resistance of teeth restored by composite laminate veneers with a composite filling and intact teeth. However, in their investigation, the failure loads were in the range of 299 ± 103 to 471 ± 125 N, which are higher than those observed in the present study.
The application of 1,000,000 cycles of loading may have negatively affected the fracture resistance of teeth in the present study, leading to the lower fracture resistance of our specimens. However, in a study by Stappert et al.15 who examined the longevity and failure load of ceramic veneers with three preparation designs, the laminate veneers were subjected to masticatory simulation. The range of failure loads of PLVs after cyclic loading was found higher (713.3-519.2 N) compared to the present study (170.9-118.9 N). A higher range of failure load is expected with axial loading, and thus the difference may be due to the different angles used for load application. In the present study, cyclic loading was applied to the cingulum, and static loading to failure was applied in a non-axial direction at 135 degrees to the incisal edge of the teeth.
Gresnigt et al.6 found that the fracture strength of teeth restored by PLVs with existing class III and IV composite fillings was higher than that of teeth with no restorations, although the difference was not significant. The fracture strength value reported by Gresnigt et al.6 was higher than that found in our study, potentially due to differences in the surface conditioning that was used. Gresnigt et al.6 suggested that the use of intraoral silica coating increased the strength of the PLVs on teeth with existing composite fillings. In the present study, only surface roughening was used to increase the micromechanical retention of the resin cement on the composite filling. This treatment is simple and requires no specific equipment.
The major type of failure was mixed or cohesive in all of the test groups. This finding confirmed the acceptable bond strength between the tooth-cement-ceramic interfaces. The investigation of fractured teeth in the present study revealed that the ceramic was chipped from the incisal edge in all but one specimen in the class III group. In contrast, most of the fractures in the class IV group occurred within the class IV cavity. The increased amount of unsupported porcelain could be the reason for this finding, which suggests that removing a class III composite and replacing it with porcelain may weaken the final restoration. Another study recommended using high-strength ceramic to compensate for the fracture of the PLVs.20 This approach may be worthwhile pursing in future studies.
When placing the margins of a PLV on an existing composite, it is important to consider that weak bonding may lead to microleakage and fracture. Microleakage could result from a difference in the flexure and thermal expansions of the tooth and the ceramic or resin composite.2,3,8 In the present study, thallium 201 was used to measure the microleakage.21,22,23 Thallium 201 is a cyclotron-generated radionuclide that degrades to mercury (emitting x-rays) and thallium (emitting gamma rays). A specific gamma counter or high-resolution camera can produce the gamma profile absorbed by a specimen immersed in the appropriate solution for several hours. Similar to fluid filtration, the gamma-counting method is nondestructive to the specimen, allowing other tests to be performed simultaneously. The size of the hydrated thallium 201 ion is similar to that of the hydrated potassium ion, which can enter any gap in a water molecule. Thallium tracing may reveal the amount of water contaminating a test specimen and therefore is relevant to the physiological oral condition. However, the lack of a microleakage pattern is an important drawback of this method, which may be compensated for by employing a gamma imaging camera. Another limitation of this method is its poor repeatability; all of the specimens must be examined in the same solution at the same time.
The results demonstrated that cyclic loading significantly increased the microleakage of teeth in the test groups, and microleakage after loading was significantly higher in the class IV group than in the intact teeth control group. The flexural difference between the tooth structure and ceramic materials could cause gap formation and increase microleakage. In addition, the increased surface of the tooth-resin-ceramic interface decreased the flexural strength in the class IV group teeth.24 This finding may explain the higher microleakage observed in the class IV teeth. It is not possible to compare our results with other studies due to a lack of similar research. Nevertheless, the results of the present study are consistent with the findings of published clinical trials that have demonstrated that microleakage increases as the enamel surface available for bonding decreases.25,26 It has been an anecdotal recommendation to preserve 50% to 70% of the enamel or all intraenamel margins with bonded PLV to achieve better results.25,26 An enamel margin has also been shown to improve the bond strength and reduce the nanoleakage of the composite /resin interface with resin cements.27 However, further investigation is required to determine the optimal amount of enamel surface and intraenamel margin.
Within the limitations of the present study, it may be concluded that microleakage and fracture resistance were not significantly different between PLV-restored teeth with existing class III composites and those without previous fillings. The microleakage and fracture resistance of PLV-bonded teeth with a class IV cavity were unfavorable compared with PLV-bonded intact teeth or teeth with class III cavities. These findings indicate that removing a class III composite filling to prepare the tooth for PLVs may have limited benefit in terms of preventing fracture and microleakage.
Figures and Tables
 | Fig. 1The design of PLV preparation on a tooth with class III composite filling. Blue lines demonstrates the position of inter proximal margin. |
 | Fig. 2The design of PLV preparation on a tooth with class IV cavity. The blue line demonstrates the position of interproximal margin. |
Table 1
The descriptive data for microleakage values of test groups before and after cyclic loading

Table 2
Comparison of microleakage test between test groups after cyclic loading

References
1. Calamia JR, Calamia CS. Porcelain laminate veneers: reasons for 25 years of success. Dent Clin North Am. 2007; 51:399–417.
2. Peumans M, Van Meerbeek B, Lambrechts P, Vanherle G. Porcelain veneers: a review of the literature. J Dent. 2000; 28:163–177.
3. Peumans M, De Munck J, Fieuws S, Lambrechts P, Vanherle G, Van Meerbeek B. A prospective ten-year clinical trial of porcelain veneers. J Adhes Dent. 2004; 6:65–76.
4. Beier US, Kapferer I, Burtscher D, Dumfahrt H. Clinical performance of porcelain laminate veneers for up to 20 years. Int J Prosthodont. 2012; 25:79–85.
5. Burke FJ. Survival rates for porcelain laminate veneers with special reference to the effect of preparation in dentin: a literature review. J Esthet Restor Dent. 2012; 24:257–265.
6. Gresnigt MM, Ozcan M, Kalk W, Galhano G. Effect of static and cyclic loading on ceramic laminate veneers adhered to teeth with and without aged composite restorations. J Adhes Dent. 2011; 13:569–577.
7. Guess PC, Stappert CF. Midterm results of a 5-year prospective clinical investigation of extended ceramic veneers. Dent Mater. 2008; 24:804–813.
8. Chun YH, Raffelt C, Pfeiffer H, Bizhang M, Saul G, Blunck U, Roulet JF. Restoring strength of incisors with veneers and full ceramic crowns. J Adhes Dent. 2010; 12:45–54.
9. Dennison JB, Sarrett DC. Prediction and diagnosis of clinical outcomes affecting restoration margins. J Oral Rehabil. 2012; 39:301–318.
10. Magne P, Kwon KR, Belser UC, Hodges JS, Douglas WH. Crack propensity of porcelain laminate veneers: A simulated operatory evaluation. J Prosthet Dent. 1999; 81:327–334.
11. Kuper NK, Opdam NJ, Bronkhorst EM, Ruben JL, Huysmans MC. Hydrodynamic flow through loading and in vitro secondary caries development. J Dent Res. 2013; 92:383–387.
12. Gresnigt MM, Kalk W, Özcan M. Clinical longevity of ceramic laminate veneers bonded to teeth with and without existing composite restorations up to 40 months. Clin Oral Investig. 2013; 17:823–832.
13. Summitt JB. Fundamentals of operative dentistry: A contemporary approach. 3rd ed. Chicago: Quintessence Pub;2006. p. 472.
14. Behr M, Rosentritt M, Latzel D, Kreisler T. Comparison of three types of fiber-reinforced composite molar crowns on their fracture resistance and marginal adaptation. J Dent. 2001; 29:187–196.
15. Stappert CF, Ozden U, Gerds T, Strub JR. Longevity and failure load of ceramic veneers with different preparation designs after exposure to masticatory simulation. J Prosthet Dent. 2005; 94:132–139.
16. Öztürk E, Bolay Ş, Hickel R, Ilie N. Shear bond strength of porcelain laminate veneers to enamel, dentine and enamel-dentine complex bonded with different adhesive luting systems. J Dent. 2013; 41:97–105.
17. Bayne SC. Dental restorations for oral rehabilitation - testing of laboratory properties versus clinical performance for clinical decision making. J Oral Rehabil. 2007; 34:921–932.
18. Rueggeberg FA. Substrate for adhesion testing to tooth structure - review of the literature. Dent Mater. 1991; 7:2–10.
19. Ozcan M, Mese A. Fracture strength of indirect resin composite laminates to teeth with existing restorations: an evaluation of conditioning protocols. J Adhes Dent. 2009; 11:391–397.
20. Turkaslan S, Tezvergil-Mutluay A, Bagis B, Shinya A, Vallittu PK, Lassila LV. Effect of intermediate fiber layer on the fracture load and failure mode of maxillary incisors restored with laminate veneers. Dent Mater J. 2008; 27:61–68.
21. Saraç YS, Başoğlu T, Ceylan GK, Saraç D, Yapici O. Effect of denture base surface pretreatment on microleakage of a silicone-based resilient liner. J Prosthet Dent. 2004; 92:283–287.
22. Sarac D, Sarac YS, Basoglu T, Yapici O, Yuzbasioglu E. The evaluation of microleakage and bond strength of a silicone-based resilient liner following denture base surface pretreatment. J Prosthet Dent. 2006; 95:143–151.
23. Geramipanah F, Rezaei SM, Sichani SF, Sichani BF, Sadighpour L. Microleakage of different post systems and a custom adapted fiber post. J Dent (Tehran). 2013; 10:94–102.
24. Magne P, Douglas WH. Cumulative effects of successive restorative procedures on anterior crown flexure: intact versus veneered incisors. Quintessence Int. 2000; 31:5–18.
25. Fradeani M, Redemagni M, Corrado M. Porcelain laminate veneers: 6- to 12-year clinical evaluation-a retrospective study. Int J Periodontics Restorative Dent. 2005; 25:9–17.
26. Friedman MJ. Porcelain veneer restorations: a clinician's opinion about a disturbing trend. J Esthet Restor Dent. 2001; 13:318–327.
27. Kasaz AC, Pena CE, de Alexandre RS, Viotti RG, Santana VB, Arrais CA, Giannini M, Reis AF. Effects of a peripheral enamel margin on the long-term bond strength and nanoleakage of composite/dentin interfaces produced by self-adhesive and conventional resin cements. J Adhes Dent. 2012; 14:251–263.




 PDF
PDF ePub
ePub Citation
Citation Print
Print






 XML Download
XML Download