Abstract
PURPOSE
To compare marginal and internal gaps of zirconia substructure of single crowns with those of three-unit fixed dental prostheses.
MATERIALS AND METHODS
Standardized Co-Cr alloy simulated second premolar and second molar abutments were fabricated and subsequently duplicated into type-III dental stone for working casts. After that, all zirconia substructures were made using Lava™ system. Marginal and internal gaps were measured in 2 planes (mesial-distal plane and buccal-palatal plane) at 5 locations: marginal opening (MO), chamfer area (CA), axial wall (AW), cusp tip (CT) and mid-occlusal (OA) using Replica technique.
RESULTS
There were significant differences between gaps at all locations. The mean ± SD of marginal gap in premolar was 43.6 ± 0.4 µm and 46.5 ± 0.5 µm for single crown and 3-unit bridge substructure respectively. For molar substructure the mean ± SD of marginal gap was 48.5 ± 0.4 µm and 52.6 ± 0.4 µm for single crown and 3-unit bridge respectively. The largest gaps were found at the occlusal area, which was 150.5 ± 0.5 µm and 154.5 ± 0.4 µm for single and 3-unit bridge premolar substructures respectively and 146.5 ± 0.4 µm and 211.5 ± 0.4 µm for single and 3-unit bridge molar substructure respectively.
CONCLUSION
Independent-samples t-test showed significant differences of gap in zirconia substructure between single crowns and three-unit bridge (P<.001). Therefore, the span length has the effect on the fit of zirconia substructure that is fabricated using CAD/CAM technique especially at the occlusal area.
Metal-ceramic restoration has been used successfully in dentistry. Although it provides favorable results in terms of strength, form and function, it usually shows unaesthetic appearance from metal underneath, especially at the cervical part of the restoration or from the opaque porcelain layer.1 In addition, metal substructure obstructs the light transmission to underlying natural tooth, and its oxide discoloration affects the appearance of the prosthesis. For some patients, alloys, used in PFM restorations, may induce allergic reaction to the patients.1 Therefore, the high-gold-content alloys are sometimes used to solve the unaesthetic problem in fixed dental prosthesis with low allergic reaction to the patients, but this type of alloys is relatively expensive.2,3 When first high-alumina content porcelain was developed for fabrication of all-ceramic crown,4 it presented superior aesthetics similar to natural dentition, however it is relatively weak with limited clinical use and prone to fracture under function. Before the application of zirconia in fabrication fixed dental prosthesis (FDP), it was found that the primary cause of failures of all-ceramic FDP was the fracture of the connector5,6,7,8,9 which differed from that reported for metal-ceramic FDP.10,11 Since then, zirconia-based ceramic has been developed and introduced as restorative materials for fabrication of FDP especially in posterior region because of its excellent mechanical properties. This ceramic has the highest fracture toughness and strength compared with other substructure ceramics.12 In combination with CAD/CAM technique, this high strength ceramic can be conveniently fabricated from partially sintered or fully sintered blocks by avoiding conventional steps such as waxing, investing, and casting. However, machining from fully dense block requires robust milling equipment, and it is questionable for the accuracy of milling the thin section of brittle material.13 For partially sintered zirconia, it can be easily machined using CAM system and subsequently sintered to retrieve fully dense framework. However, large sintering shrinkage approximately of 25% needs to be compensated by calculation of software design.13,14
Since the introduction of zirconia as FDP, the fracture of zirconia framework has been rarely reported.15,16 Apart from the excellent mechanical properties of the framework, the long-term clinical success of zirconia-based restoration can be influenced by marginal and internal fit of the prostheses.17,18,19,20 The poor marginal fit leads to plaque accumulation and secondary caries, induces periodontal disease, and creates microleakage.15,21,22,23,24,25,26 It was reported that the highest rate of marginal discoloration was found in zirconia FDP.16 This may be resulted from the marginal inaccuracy of those zirconia frameworks. A variety of acceptable marginal openings were recommended. Hung et al.27 and Weaver et al.28 suggested that an acceptable marginal opening were 50 to 75 µm and 70 ± 10 µm respectively. Nevertheless, there is an agreement that marginal discrepancy between 100-150 µm is clinically acceptable.20,29,30,31,32 However, there have been still very few data available on the measurement of the fit in zirconia substructure compared between the different types of fixed dental restorations. Therefore, the objective of this study was to compare the marginal and internal gaps of zirconia substructure of single crown and those of three-unit fixed dental prostheses.
Commercially available Y-TZP zirconia block (Lava™ zirconia block, 3M ESPE, St. Paul, MN, USA) and CAD/CAM system (Lava™ Scan ST Design, Lava™ CNC 500 Milling Machine and Lava™ Furnace 200, 3M ESPE, St. Paul, MN, USA) were used in this study. Ivorine® maxillary teeth (Columbia Dentoform® Corp, Long Island City, NY, USA) were embedded in model stone type III (Comet 3, Ultima, Ayutthaya, Thailand) simulating a second premolar and a second molar in a position of abutments for zirconia all-ceramic single crowns (premolar and molar) and three-unit fixed dental prostheses (tooth 25-27). A putty type silicone impression (Express, 3M ESPE, St. Paul, MN, USA) was made as a silicone index to control volumetric reduction of abutment teeth in this study. After that, Ivorine® maxillary teeth were prepared as complete-coverage zirconia all-ceramic single crowns and a three-unit bridge restorations. After preparation was completed, the Ivorine® abutment teeth in model stone type III (Kerr Lab, Orange, CA, USA) platform were duplicated using silicone duplicate material (Wirosil, BEGO, Bremen, Germany) and casted for a standardized Co-Cr model (Fig. 1).
Impressions of standardized Co-Cr model were taken using customized perforated plastic tray and polyether impression material (Impregum™ 3M ESPE, St. Paul, MN, USA). Then all impressions were poured with die stone type IV (Velmix, Kerr Lab, Orange, CA, USA) for working models. After models were fully set, all models were labeled and divided into 2 groups (n=10/group): single crowns (premolar and molar) and 3-unit bridge before transferring to the milling center. Zirconia substructures were fabricated using the Lava™ system (3M ESPE, St. Paul, MN, USA). The same standard setting was employed to all scanning models with cement spacer: 15 µm at the margin and finish line; additional cement space of 50 µm (65 µm total) at 2 mm above the margin of restoration; and additional 65 µm (85 µm total) at the occlusal area. 0.5 mm thick substructures were fabricated for all crowns and bridges. When substructure fabrication process was finished, all the definitive substructures were returned to their respective groups and examined by the investigators for any defect. The internal replica technique was employed by loading low-viscosity silicone impression material (Express XT, 3M ESPE, St. Paul, MN, USA) on the inner surface of the substructure and seating substructure on Co-Cr model using 50 N load. Subsequently, heavy body silicone impression material (Express XT, 3M ESPE, St. Paul, MN, USA) was used to stabilize the thin layer of light body impression material for easy handling and to determine the gaps of zirconia substructure (Fig. 2).
All the replicas of abutment teeth, which adhered to custom plastic tray, were sectioned with razor blade (Dorco Co., Ltd., Seoul, Korea) in the mid-plane at buccal-lingual surface and mesial-distal surface. Each part of the replica was examined under optical light microscope (Nikon eclipse E400 POL, Sendai, Japan) at a magnification of ×50, and photograph was taken for gap measurement using DSLR camera (Canon EOS 450D, Sendai, Japan). Finally, the gaps were measured in 5 positions (9 points/section) (Fig. 3 and Fig. 4): marginal opening (MO), chamfer area (CA), axial wall (AW), cusp tip (CT), occlusal adaptation (OA) using Image pro plus program v.7.0 (Media Cybernatics, Rockville, MD, USA).
All marginal and internal gap data were collected and analyzed using independent t-test statistic at a significance level of 0.05 (SPSS version 11, Armonk, NY, USA) to determine if statistical differences exist between both types of substructures in terms of marginal and internal gaps at the different measurement positions.
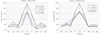
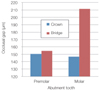
There were significant differences of marginal and internal gaps between single crown and three-unit bridge at all locations. The mean ± SD of marginal gap in premolar was 43.6 ± 0.4 µm and 46.5 ± 0.5 µm for single crown and 3-unit bridge substructure respectively. For molar substructure the mean ± SD of marginal gap was 48.5 ± 0.4 µm and 52.6 ± 0.4 µm for single crown and 3-unit bridge respectively (Fig. 5).
The largest gaps were found at the occlusal area, which were; 150.5 ± 0.5 µm and 154.5 ± 0.4 µm for single and 3-unit bridge premolar substructures respectively; and 146.5 ± 0.4 µm and 211.5 ± 0.4 µm for single crown and 3-unit bridge molar substructure respectively (Fig. 6).
All-ceramic restorations have become increasingly popular because of their esthetics, biocompatibility and improved strength. Previously, all-ceramic restorations require some steps in fabrication process that could lead to an inaccuracy of the restorations. CAD/CAM technology was introduced to derive precision and enhance the predictability of restorations, however, scanning process, software design, milling system, and material processing may compromise the accuracy of this method.33 The success of zirconia all-ceramic restoration depends on several factors, and one of the most important factors that makes zirconia all-ceramic restoration achieve acceptable longevity is the fit of the restorations which can be determined by marginal and internal gaps in the restorations. Misfit can affect retention, fracture strength34 and thus reduce longevity of restorations from the adverse effects of poor fit such as; damage to the adjacent tissue; or increased dissolution of the cementing medium.35 For marginal and internal gaps of zirconia restorations, it was found that the fit of zirconia restoration is influenced by heterogeneity in terms of experimental methodology, milling system, manufacturers, sintering states of the zirconia, sample size and span length.36 In this study, the marginal gap values all zirconia substructures were less than 60 µm, which was less than that of the clinically acceptable value. For the internal gap, this study showed the axial and occlusal gaps were in the range of 31-90 µm and 108-215 µm respectively. The axial gap values were slightly less than that of previous studies.36 In this study, internal relief for cement space was 15 microns, with 50 microns additional horizontal gap at 2 mm above the collar position, and 65 µm additional occlusal gap. When compared with the manufacturer's parameters, the gap in chamfer area of premolar and molar substructure were in the range of 36-62 µm and 51-82 µm respectively, which were slightly greater than setting parameter of the system.
The most used approaches to determine the adaptation of the restorations are embedded and replica techniques. The embedded method may be considered as the most accurate method for measuring the marginal and internal fit, however, the disadvantage is the destruction of the material from the cutting. In this study, the replica technique that is the non-destructive method was used to determine the gap under zirconia substructure. By using the low-viscosity impression material to represent the marginal and internal gap width, this approach can be as accurate as the embedded method. This method was used to investigate the accuracy of single crown and fixed dental prostheses in clinical studies.24,37,38 In this study, 50-N load was employed to insert zirconia substructure onto the standard abutment to ensure the complete seating of the substructure. This applied load was employed according to our pilot study, which we found that there was no difference of marginal gap between the zirconia substructures with low-viscosity impression material and those without the material.
From this study, the gap values in three-unit substructures were higher than those of single crowns. The study also showed that even though the manufacturer's recommended parameters were set for CAD/CAM zirconia system, the gaps were not as precise as the setting parameter by the system especially at the occlusal area. This may be because of the more complex shape of the occlusal surface of the molar and the larger dimension of bridge framework than those of single crown substructure. Those factors may influence the adaptation of the zirconia framework. In addition, the calculation of the CAD/CAM software may not as precise as it should be. Therefore, it has to be considered that a tendency for the greater gaps than the expected value could be found. In addition, as in the tooth preparation step, clinicians should always remind themselves to prepare enough space for the restorations. Because the gaps increment in the restorations can be greater than the set-up value of the system when the FDPs have larger span length, it should be considered that the span length, the type of the restorations or other factors may have a significant effect on the marginal and internal gaps of zirconia restorations. There should be further studies to investigate other factors to clarify how those effects could be avoided in routine CAD/CAM fabrication for zirconia restorations.
According to the experimental results, all the marginal gaps were less than 120 microns, which is clinically acceptable for the system used in this study. However, the measured gaps tended to be greater than those of the parameter set by CAD system especially at the occlusal area. In addition, the fit of zirconia substructure was also affected by the dimension of the restorations in which the gaps of bridge substructure was larger than those of single-unit substructure.
Figures and Tables
References
1. Rosenblum MA, Schulman A. A review of all-ceramic restorations. J Am Dent Assoc. 1997; 128:297–307.
2. Magne P, Belser U. Esthetic improvements and in vitro testing of In-Ceram Alumina and Spinell ceramic. Int J Prosthodont. 1997; 10:459–466.
3. Shepard FE, Moon PC, Grant GC, Fretwell LD. Allergic contact stomatitis from a gold alloy-fixed partial denture. J Am Dent Assoc. 1983; 106:198–199.
4. McLean JW, Hughes TH. The reinforcement of dental porcelain with ceramic oxides. Br Dent J. 1965; 119:251–267.
5. Kelly JR, Tesk JA, Sorensen JA. Failure of all-ceramic fixed partial dentures in vitro and in vivo: analysis and modeling. J Dent Res. 1995; 74:1253–1258.
6. Olsson KG, Fürst B, Andersson B, Carlsson GE. A long-term retrospective and clinical follow-up study of In-Ceram Alumina FPDs. Int J Prosthodont. 2003; 16:150–156.
7. Sorensen JA, Cruz M, Mito WT, Raffeiner O, Meredith HR, Foser HP. A clinical investigation on three-unit fixed partial dentures fabricated with a lithium disilicate glass-ceramic. Pract Periodontics Aesthet Dent. 1999; 11:95–106. quiz 108.
8. Sorensen JA, Kang SK, Torres TJ, Knode H. In-Ceram fixed partial dentures: three-year clinical trial results. J Calif Dent Assoc. 1998; 26:207–214.
9. Vult von Steyern P, Jönsson O, Nilner K. Five-year evaluation of posterior all-ceramic three-unit (In-Ceram) FPDs. Int J Prosthodont. 2001; 14:379–384.
10. Libby G, Arcuri MR, LaVelle WE, Hebl L. Longevity of fixed partial dentures. J Prosthet Dent. 1997; 78:127–131.
11. Campbell SD, Sozio RB. Evaluation of the fit and strength of an all-ceramic fixed partial denture. J Prosthet Dent. 1988; 59:301–306.
12. Kelly JR. Dental ceramics: current thinking and trends. Dent Clin North Am. 2004; 48:viii513–530.
13. Denry I, Kelly JR. State of the art of zirconia for dental applications. Dent Mater. 2008; 24:299–307.
14. Abduo J, Lyons K, Swain M. Fit of zirconia fixed partial denture: a systematic review. J Oral Rehabil. 2010; 37:866–876.
15. Sailer I, Fehér A, Filser F, Gauckler LJ, Lüthy H, Hämmerle CH. Five-year clinical results of zirconia frameworks for posterior fixed partial dentures. Int J Prosthodont. 2007; 20:383–388.
16. Sailer I, Pjetursson BE, Zwahlen M, Hämmerle CH. A systematic review of the survival and complication rates of allceramic and metal-ceramic reconstructions after an observation period of at least 3 years. Part II: Fixed dental prostheses. Clin Oral Implants Res. 2007; 18:86–96.
17. Raigrodski AJ. Contemporary materials and technologies for all-ceramic fixed partial dentures: a review of the literature. J Prosthet Dent. 2004; 92:557–562.
18. Raigrodski AJ. Contemporary all-ceramic fixed partial dentures: a review. Dent Clin North Am. 2004; 48:viii531–544.
19. Devigus A, Lombardi G. Shading Vita YZ substructures: influence on value and chroma, part I. Int J Comput Dent. 2004; 7:293–301.
20. Beuer F, Neumeier P, Naumann M. Marginal fit of 14-unit zirconia fixed dental prosthesis retainers. J Oral Rehabil. 2009; 36:142–149.
21. Glauser R, Sailer I, Wohlwend A, Studer S, Schibli M, Schärer P. Experimental zirconia abutments for implant-supported single-tooth restorations in esthetically demanding regions: 4-year results of a prospective clinical study. Int J Prosthodont. 2004; 17:285–290.
22. Lang NP, Kiel RA, Anderhalden K. Clinical and microbiological effects of subgingival restorations with overhanging or clinically perfect margins. J Clin Periodontol. 1983; 10:563–578.
23. Valderhaug J, Heloe LA. Oral hygiene in a group of supervised patients with fixed prostheses. J Periodontol. 1977; 48:221–224.
24. Reich S, Wichmann M, Nkenke E, Proeschel P. Clinical fit of all-ceramic three-unit fixed partial dentures, generated with three different CAD/CAM systems. Eur J Oral Sci. 2005; 113:174–179.
25. Bindl A, Mörmann WH. Marginal and internal fit of all-ceramic CAD/CAM crown-copings on chamfer preparations. J Oral Rehabil. 2005; 32:441–447.
26. Schaerer P, Sato T, Wohlwend A. A comparison of the marginal fit of three cast ceramic crown systems. J Prosthet Dent. 1988; 59:534–542.
27. Hung SH, Hung KS, Eick JD, Chappell RP. Marginal fit of porcelain-fused-to-metal and two types of ceramic crown. J Prosthet Dent. 1990; 63:26–31.
28. Weaver JD, Johnson GH, Bales DJ. Marginal adaptation of castable ceramic crowns. J Prosthet Dent. 1991; 66:747–753.
29. Boening KW, Walter MH, Reppel PD. Non-cast titanium restorations in fixed prosthodontics. J Oral Rehabil. 1992; 19:281–287.
30. Fransson B, Oilo G, Gjeitanger R. The fit of metal-ceramic crowns, a clinical study. Dent Mater. 1985; 1:197–199.
31. Kokubo Y, Ohkubo C, Tsumita M, Miyashita A, Vult von Steyern P, Fukushima S. Clinical marginal and internal gaps of Procera AllCeram crowns. J Oral Rehabil. 2005; 32:526–530.
32. Quintas AF, Oliveira F, Bottino MA. Vertical marginal discrepancy of ceramic copings with different ceramic materials, finish lines, and luting agents: an in vitro evaluation. J Prosthet Dent. 2004; 92:250–257.
33. Bornemann G, Lemelson S, Luthardt R. Innovative method for the analysis of the internal 3D fitting accuracy of Cerec-3 crowns. Int J Comput Dent. 2002; 5:177–182.
34. Tuntiprawon M, Wilson PR. The effect of cement thickness on the fracture strength of all-ceramic crowns. Aust Dent J. 1995; 40:17–21.
35. Karlsson S. A clinical evaluation of fixed bridges, 10 years following insertion. J Oral Rehabil. 1986; 13:423–432.
36. Abduo J, Lyons K, Swain M. Fit of zirconia fixed partial denture: a systematic review. J Oral Rehabil. 2010; 37:866–876.
37. Reich S, Kappe K, Teschner H, Schmitt J. Clinical fit of four-unit zirconia posterior fixed dental prostheses. Eur J Oral Sci. 2008; 116:579–584.
38. Wettstein F, Sailer I, Roos M, Hämmerle CH. Clinical study of the internal gaps of zirconia and metal frameworks for fixed partial dentures. Eur J Oral Sci. 2008; 116:272–279.




 PDF
PDF ePub
ePub Citation
Citation Print
Print





 XML Download
XML Download