Abstract
PURPOSE
This study characterized the synthesis of a modified PMMA (Polymethyl methacrylate) denture acrylic loading platinum nanoparticles (PtN) and assessed its bacterial inhibitory efficacy to produce novel antimicrobial denture base material.
MATERIALS AND METHODS
Polymerized PMMA denture acrylic disc (20 mm × 2 mm) specimens containing 0 (control), 10, 50, 100 and 200 mg/L of PtN were fabricated respectively. The obtained platinum-PMMA nanocomposite (PtNC) was characterized by TEM (transmission electron microscopy), SEM/EDX (scanning electron microscope/energy dispersive X-ray spectroscopy), thermogravimetric and atomic absorption spectrophotometer analysis. In antimicrobial assay, specimens were placed on the cell culture plate, and 100 µL of microbial suspensions of S. mutans (Streptococcus mutans) and S. sobrinus (Streptococcus sobrinus) were inoculated then incubated at 37℃ for 24 hours. The bacterial attachment was tested by FACS (fluorescence-activated cell sorting) analysis after staining with fluorescent probe.
RESULTS
PtN were successfully loaded and uniformly immobilized into PMMA denture acrylic with a proper thermal stability and similar surface morphology as compared to control. PtNC expressed significant bacterial anti-adherent effect rather than bactericidal effect above 50 mg/L PtN loaded when compared to pristine PMMA (P=.01) with no or extremely small amounts of Pt ion eluted.
CONCLUSION
This is the first report on the synthesis and its antibacterial activity of Pt-PMMA nanocomposite. PMMA denture acrylic loading PtN could be a possible intrinsic antimicrobial denture material with proper mechanical characteristics, meeting those specified for denture bases. For clinical application, future studies including biocompatibility, color stability and warranting the long-term effect were still required.
A denture base seated on oral cavity leads to changes in weakening the natural hygienic effect of tongue and salivary flow, especially, by inducing formation and deposit of biofilms on both prosthetics and adjacent mucosa.1 Though bacterial cells could be washed out by saliva and swallowed unless they adhere and replicate, once formed, biofilms are notoriously difficult to remove. Bacterial adhesion to biomaterial, inert polymer such as denture acrylic base, and the ability of many microorganisms to form biofilms on foreign bodies are well-known steps in the pathogenesis of oral infections.1,2 The insertion of denture tends to create a new available surface for plaque formation and therefore to increase the level of microorganisms in the oral cavity, In addition, roughness voids of denture surface could accelerate initial microbial adhesion as well. To overcome these complications, performative and latent antibacterial denture base material that can kill or strongly resist against bacteria, or reduce its adhesion for preventing biofilms formation.3,4 Traditional chemical-based oral disinfectants, though they could be efficient against pathogenic microbes, their volatile ingredients and byproducts could be toxic and harmful to oral mucosa or supporting tissue.5 Occasionally, even denture cleansing itself might be compromised to some aged or hospitalized patients due to mentally or physically handicapped conditions.6,7 Systemic or local antibiotic prescriptions have been made for reducing the bacterial population, however, the emergences of more resistant and virulent strains of microorganisms become great clinical challenges.
Some metal nanoparticles (NP) have been known that they act as antibacterial agents to interact directly with microorganisms.8,9 Among them, Pt, as a low-allergy and non-genotoxic noble metal for the organism,10 has been widely used as a catalyst in diverse applications. The antibacterial activity of Pt has been known since the work of Rosenberg et al.,11 who reported its inhibitory activity on Escherichia coli division. Significantly, Pt nanoparticles (PtN), cluster of Pt atoms with sizes ranging from 1 to 100 nm, are of great interest owing to their highly catalytic activity and are currently being evaluated for the ability to reduce inflammation.10,12 Contact between PtN and bacteria promotes chemical interactions that cause bacterial cell to be disintegrated.13 PtN can scavenge reactive oxygen species (ROS),13 and free radicals from antioxidant responses can trigger chain reactions that damage bacteria. Polymeric materials such as PMMA denture acrylic resin have high structural tailorability and flexibility with a distinct potential to prevent aggregation of NP,14,15 thus, they could be an excellent candidate for the formulation of the nanocomposites based on the inclusion of NP.
Metal-polymer nanocomposites, a polymer matrix NP combined as the additives, have been developed to improve mechanical properties of polymers.16 As for dental applications, the adhesive of 4-methacryloyloxyethyl trimellitic anhydride (4-META)/methyl methacrylate (MMA) in combination with PtN increased dentin bond strength, probably due to enhanced polymerization.17,18 and the addition of PtN to resin-based materials may improve the biocompatibility as an antioxidant.19 Nevertheless, to the author's knowledge, no study has ever reported to explore the denture acrylic resin containing PtN for its antibacterial activity. Currently, denture base materials that could resist the adhesion of microorganisms are still unavailable, thus, a simple, effective and latent antimicrobial denture acrylic should be required. The aim of the present research was firstly to characterize a PMMA denture acrylic containing PtN, assessing its mechanical characters through thermal, SEM/EDX and ionic elution analysis, secondly to evaluate its antibacterial effect via FACS (fluorescence-activated cell sorting) analysis as an antibacterial nanocomposite. The hypothesis was that Pt-PMMA nanocomposites (PtNC) would decrease bacterial adherence and result in a proper mechanical characters for possibility of clinical use.
PtN were synthesized by chemical reduction method as follows. Colloidal PtN were prepared by mixing the following two solutions in a homomixer (T.K. Homomixer Mark II, Tokushu Kika Kogyo Co., Ltd., Tokyo, Japan). Solution one was prepared by dissolving 6.0 g of PVP (Polyvinyl Pyrrolidon) as the stabilizing agent in aqueous solution (1908 mg/L, 250 mL) of chloroplatinic acid hydrate (H2PtCl6, Aldrich, St. Louis, USA). Solution two was prepared by dissolving 0.05 g of sodium borohydride (NaBH4) in aqueous solution (250 mL) of PVP (12.5 g). Then, those two solutions were rapidly mixed by homomixer at 3500 rpm (revolution per minute). The TEM image (Fig. 1) shows that the size of prepared PtN supplied approximately 3-5 nm.
A self cured denture base acrylic resin (Vertex®, Vertex-Dental B.V., Zeist, Netherlands) was used in this study. The maximum dose of NP loading was controlled under 2.0 weight (wt) % (approximately 200 mg/L) to consider the mechanical aspects. To synthesize modified denture base specimens combined with PtN, colloidal PtN was preliminary impregnated to the polymer (pristine denture PMMA powder) at the concentrations of 10, 50, 100, 200 mg/L respectively. Specimen without PtN incorporated (0 mg/L) was used as control. Dehydration of combined powders was conducted through drying for 120 hours at room temperature and desiccating in an oven at 37℃ for 48 hours. Completely dried powders were passed through a sieve (60 mesh) and homogenized in a ball mill for 1 hour. PtN loaded powders were then mixed with resin monomer at designated P/L ratio (1.7 g : 0.95 g by wt %) and the mixture was packed into a custom-made brass moulds then covered by two glass frames with 10 Kg static pressure. All of mixtures were cured under the manufacturer's instructions and trimmed. Fifty specimens were fabricated to uniform disk shape (20 mm × 2.0 mm) and they were divided into five groups (n = 10) according to the concentrations of PtN incorporated.
The microstructure of obtained PtNC was performed to identify the PtN in samples successfully loaded by a field emission electron microscope attached to SEM/EDX (Hitachi S-4100 FE-SEM/EDS, Tokyo, Japan) at an accelerated voltage of 20 KeV. The PtNC samples were gold sputtered under high vacuum before the analysis.
Thermogravimetric (TG) analyses and differential scanning calorimetry (DSC) were carried out simultaneously using a TG-DTA 92 (Setaram, Caluire, France) instrument with a heating rate of 10℃/min from 30 to 600℃ under nitrogen atmosphere.
An atomic absorption spectrophotometer (Analyst 100, Perkin-Elmer, Krakow, WI, USA) and shaking incubator (SI-600R, JEIO TECH, Seoul, Korea) were used. Each disc specimen (20 mm × 2.0 mm, n = 15) was put into 100 mL of sterile distilled water and stored at 37℃ under agitation. The values of eluted Pt ion were determined at 24 and 120 hours with daily replacing distilled water. The quantity of elution was scored as the amounts of Pt ion in the solution per unit of surface area of the disc (cm2) and the measurements were performed in three independent tests.
Bacteria tested in this study were S. mutans (Streptococcus mutans, ATCC 25175) and S. sobrinus (Streptococcus sobrinus, ATCC 27607). Streptococci were maintained on BHI (brain heart infusion) and they were grown under aerobic conditions. Before antimicrobial assay, specimens were stored in sterilized distilled water for 2 weeks to leach excess residual monomer then ultrasonically cleaned (Branson 2200; Branson, Danbury, CT, USA) for 1 hour. To secure the sterility of specimens, sterilization with ethylene oxide gas for 24 hours was also conducted then specimens were coated with synthetic saliva (Taliva, Hanlim Pharm. Co., Seoul, Korea) for 1 hour before contacting to bacteria to mimic the oral cavity. Bacterial species were inoculated in BHI broth and incubated for 6 hours, to the point when growth is considered to be in the logarithmic phase. Followed by inoculating 1% (v/v) of the bacterial seed suspension to 1.5 mL medium in 12-well plate (Costa, Corning Co., Corning, NY, USA) containing specimens, they were cultured for 24 hours at 37℃ condition. After incubation, all of experimental specimens were washed out 3-times with PBS (Phosphate Buffered Saline), the adherent bacteria on each samples were then detached into 1 mL PBS by sonication for four 30 second-pulses with three 30 seconds intermittent cooling. All of samples were centrifuged at 10,000 g for 3 minutes to pellet the cells. Bacterial counting of attached streptococci were performed by FACS analysis after staining with bacterial viability and counting kit (Molecular Probes, Eugene, OR, USA). Briefly, bacterial pellets were resuspended in 500 µL of PBS which contain 0.1 µL of 3.34 mM SYTO 9 nucleic acid stain (for live and dead bacteria staining) and 0.1 µL of 30 mM propidium iodide (PI, for dead bacteria-specific staining). Cells were incubated for 15 minutes at room temperature protected from light. For the final step, added 1 µL of the microsphere suspension to the stained cell sample as a reference standard for sample volume then mixed well and analyzed by flow cytometry analysis (Accuri Flow Cytometer, BD Biosciences, San Jose, CA, USA). The populations of live and dead bacteria were calculated from either the fluorescence versus side scatter cytogram or the green fluorescence versus red fluorescence cytogram. To confirm the differentiation between live and dead bacteria by fluorescent staining, stained bacterial sample images were analyzed under fluorescent microscope (Olympus BX 51, Olympus, Tokyo, Japan).
The bacterial inhibitory effects of PtNC were evaluated by one-way ANOVA, followed by Student's t-test for post-Hoc test. A significance level of 0.01 was used for statistical tests. All statistical analyses were performed using SPSS 18.0 for Windows (SPSS Inc., Chicago, IL, USA).
SEM/EDX analysis identified that Pt peak is clearly shown which indicates that PtN were successfully loaded and immobilized into PMMA (Fig. 2). The SEM images of surface of 200 mg/L PtNC (Fig. 3A) exhibited similar surface texture to that of control (Fig. 3B) with slightly increased cracking and blistering observed. Thermal analysis of 200 mg/L of PtNC showed stable polymerization phase and improved thermal stability by TG/DSC curves in comparison with control (Fig. 4). TG curve of PtNC showed closely similar aspect to that of control with a sharp weight reduction observed from 350℃ to 400℃ (Fig. 4A). DSC curve for PtNC also expressed a similar thermogram from 30℃ to 600℃ with the slightly increased endothermic peak at 389.2℃ as compared to 384.7℃ in that of control (Fig. 4B). The eluted Pt ion were not calculated from 10 to 100 mg/L Pt loaded groups at two designated times, only revealed significantly in PtNC of 200 mg/L with values of 0.11 ± 0.10 mg/L at 24 hours and 0.08 ± 0.07 at 120 hours without statistical difference between two periods (Table 1).
The bacterial anti-adhesion effect of PtNC against two streptococci tested at 24 hour-incubation is expressed as the reduction of bacterial adhesion after contact with PtNC. Most of the cells attached were viable cell while dead bacterial cells were detected less than 10% of total attached bacteria (Table 2) presented by fluorescent signal specific to live and dead cells staining (Fig. 5). Antibacterial effect of PtNC were determined by the number of viable cells from biofilm in the retrieved suspension then calculated as the percentage of the control. When compared to control, modified denture base above 50 mg/L of PtN loaded significantly reduced bacterial adhesion (P=.01) and loading 200 mg/L of PtN reduced the viable cell adherence 88.9 % in S. mutans and 88.2 % in S. sobrinus with a statistically higher effect than 50 and 100 mg/L of PtN loaded (Fig. 6). However, there were no statistical differences between two streptococci (P=.01)
The same lower case letters are not statistically different (P=.01).
Nanoparticles, ranging from 1 to 100 nm in size, derived from noble metals are regarded as non-genotoxic for the organism10,20 and their antibacterial action is highly dependent on functional groups present on the surface, which may determine toxic effects.12,21 In the present study, the size of PtN processed was platinum seeds under 5 nm in an aqueous solution through chemical ripening. The size of NP could affect their antibacterial levels, the smaller in size, especially for sizes under 30 nm,22 the higher in catalytic activities including antimicrobial action.23,24
Though the knowledge have already been acquired for the antimicrobial capacity of several colloidal NP against various bacteria,25,26 few information about the antimicrobial effect after their incorporation to polymer has been reported.23 In addition, no golden standard for the assessment on antimicrobial dental materials has been established so far, especially in denture acrylic. FACS analysis conducted in the present study is known as an analytical measurement of light scattered and fluorescence emission produced by suitably illuminated bacterial cells27 and FACS complemented with microscopic evaluation enables colony to be differentiated as viable or dead bacteria on infected samples.28 FACS could provide antibacterial compounds used in oral cavity for determining their effectiveness with simple, rapid and precise detection of the viability of microbes27 and offers several advantages over standard CFU (colony forming unit) count, which offers no information about the presence of viable but non-culturable bacteria.
According to the results of FACS, PtNC did not reveal strong bactericidal action against two streptococci but rather expressed the anti-adherent effect with no or extremely small amounts of Pt ion eluted. These results were not unexpected for solid acrylic resin bulk simply thought to have a low interaction with bacteria rather than a strong bactericidal effect. The rare or extremely restricted Pt ion or PtN eluted could be related to the structure of the hydrophobic polymer network whose water uptake may not be sufficient for ion release from particles situated in the PMMA bulk.29 Moreover, a denture acrylic Vertex® used contains a crosslinking agent, ethylene glycol dimethacryl [2-(2-Methylacryloyloxy) ethyl 2-methyl-acrylate)], and probably PtN could be strongly trapped into the crosslinked polymer structure. While antimicrobial characteristic of silver NP-incorporated polymers was explained as the ionic elution from the polymer diffused by water molecules to the aqueous medium,30 other studies announced that solid composite resin combined with NP or antiseptic microfiller, regardless of inorganic ions leaching, the bacterial inhibitory effects were due to direct contact between microorganisms and NP31.32 or the filler particles immobilized on the surface of compounds.33 Nevertheless, the mechanism of antimicrobial compound such as nanocomposite in the present study has not been fully elucidated yet. Bacterial behavior varies especially as a function of material electrostatic charge or hydrophobicity, and physico-chemical properties exhibited by material surface may influence the kinetics of microbial adhesion.23 Plastic surfaces generally possess various degrees of negative net surface charge, similarly, all living bacterial cells (including yeasts) possess a net negative surface charge.2 Kiremitci-Gumustederelioglu and Pesmen34 suggested bacterial adhesion would be reduced on negatively charged PMMA/AA (acrylic acid), while increased on positively charged PMMA/DMAEMA (dimethylamino ethyl methacrylate). It could be speculated that incorporating PtN above 50 mg/L into PMMA denture acrylic may alter the physicochemical interactions or modify the polarity of PtNC surface into more negatively charged which induce the dominant repulsive force, i.e., anti-adherent power, against the negatively charged bacterial cell wall rather than attractive force, i.e., sterilizing one. This anti-adherent effect could be correlated with the complexity of nanocomposite surface as well as the change in its chemical composition and synthesis. Well-dispersed PtN were prepared by chemical ripening with PVP as coating and stabilizing agents for effective NP dispersion in this study. PVP has been used by many researchers, to protect NP from growing and agglomerating.35 El Badawy et al.36 reported the surface charge-dependent toxicity of several coating types for NP and Silva et al.37 demonstrated the lowest charge difference as observed for PVP-silver NP against bacterial cell wall as compare to citrate and branched polyethyleneimine. They suggested that the dominant repulsive forces (lower attraction) might have played a key role in keeping PVP-silver NP away from the biologic surfaces causing the low toxicity. Hydrophobic interaction could also play an important role in bacterial adherence to PtNC surfaces because the electrical forces are minor to the hydrophobic forces, since adherence to a considerable extent occurs even in the presence of this repulsive force.2,38,39 It was reported that bacterial adherence to hydrophobic surfaces is affected by a change in interfacial free energy which corresponds to the process of attachment39 and adherence occurs whenever the sum total of interfacial tensions cellsolid is reduced.2
Regarding the clinical situation under denture in oral cavity, it would be more desirable to develop antimicrobial material characterized by anti-adherent effect whose primary scope is the prevention, not a treatment that might cause undesirable interactions with host tissues. However, further studies should be still required to confirm the bacteri-nanocomposite interaction including other unknown factors that may influence the bacterial adherence to nanocomposite surface. In addition, for clinical application, biocompatibility and long-term effect remain to be investigated as well as challenge to analysis for other strains because predicting the behavior of one or two strain is not sufficient for achieving usable indications on the properties of PtNC.
Denture base as a thermoplastic material could be influenced by temperature variances such as foods intake in the mouth, cleansing, and particularly the manufacturing stage such as curing and polishing processes.40 Thus, it is significant to assess the stability of modified PMMA composition against heat.41 Thermal stability is a general term used to determine the potential changes of a material and it has a significant implication as far as polymer fabrication processes are concerned.42 TG/DSC thermal analysis are generally used in the research of dental materials to monitor the polymerization or setting reactions of dental resins, and to measure the glass transition temperatures of polymers.40,43 Poor thermal stability of PMMA leads to a negative influence on physical properties of the composites,43 even if modified denture polymer expresses the antibacterial effect. As shown in Fig. 4, despite incorporating the highest dose (200 ppm) of PtN to PMMA resin, similar TG thermogram with control was revealed and DSC peaks were not varied significantly, which indicates that the melting point of PtNC have no apparent variation to that of pristine PMMA at the experimental temperature. TG/DSC results suggest that PtN-PMMA denture nanocomposites could be synthesized with stable thermal and physical properties regardless of PtN incorporatating. However, further mechanical evaluations such as flexural strength and optical stability should be still needed for security of clinical applications.
Within the limitations of this study, PtNC was successfully synthesized with stable thermal stability and exhibited the possibility to produce bacterial anti-adherent surfaces by acting on the nanotopology, reducing the area available for bacterial adhesion. Thus, PtNC could be a possible candidate for the application in the futuristic dental biomaterial.
Figures and Tables
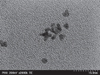 | Fig. 1TEM micrograph of PtN prepared in this study. PtN are shown as spherically shaped particles measuring 3-5 nm in diameter. |
 | Fig. 2The SEM/EDX pattern of PtNC electrode. The spectrum shows the characteristic peaks of Pt representing successful loading of PtN into PMMA. Unassigned peaks originate from polymer or external contaminants. |
 | Fig. 3SEM image of 200 mg/L PtNC (A) reveals similar surface texture with slightly increasing surface cracking and blistering as compared to control (B)(×50). |
 | Fig. 4In comparative TG-DSC analysis, PtNC showed stable copolymerization phase and thermal property regardless of PtN added. As compared to control, PtNC (200 mg/L) expressed closely overlapped TG curves with that of control at weight loss temperature ranged from 350℃ to 400℃ (A). In DSC thermogram ranging from 30℃ to 600℃, the melting point of PtNC (389.2℃) is slightly higher to that of control (384.7℃), demonstrating improved thermal property (B). |
 | Fig. 5Microscopic image (×500) of fluorescent antibody-stained attached S. mutans with live/dead staining for adherent cell counting. Live (A: control, B: 200 mg/L PtNC) and dead (C: control, D: 200 mg/L PtNC) bacteria are expressed as green versus red stain (dots). |
 | Fig. 6Anti-adherent effect of PtNC agaisnst viable streptococci. As compared with control, PtNC above 50 mg/L of PtN loaded significantly reduced bacterial adhesion and there were no statistical differences between S. mutans and S. sobrinus (P=.01). |
Table 1
Concentrations (mg/L) of eluted Pt ion from experimental PtNC and control

| PtN loaded (mg/L) | Amounts of eluted Pt ion (mg/L) | |
|---|---|---|
| 24 hours | 120 hours | |
| Control (0) | N.D.a | N.D.a |
| 10 | ||
| 50 | ||
| 100 | ||
| 200 | 0.11 ± 0.10*,b | 0.08 ± 0.07*,b |
Table 2
Numbers of viable and dead streptococci on PtNC through live and dead staining

References
1. Yildirim MS, Hasanreisoglu U, Hasirci N, Sultan N. Adherence of Candida albicans to glow-discharge modified acrylic denture base polymers. J Oral Rehabil. 2005; 32:518–525.
2. Klotz SA, Drutz DJ, Zajic JE. Factors governing adherence of Candida species to plastic surfaces. Infect Immun. 1985; 50:97–101.
3. Loesche WJ. Role of Streptococcus mutans in human dental decay. Microbiol Rev. 1986; 50:353–380.
4. Saito T, Takatsuka T, Kato T, Ishihara K, Okuda K. Adherence of oral streptococci to an immobilized antimicrobial agent. Arch Oral Biol. 1997; 42:539–545.
5. Murdoch-Kinch CA, Mallatt ME, Miles DA. Oral mucosal injury caused by denture cleanser tablets: a case report. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1995; 80:756–758.
6. Stone C, Sabes WR. Denture cleaner chemical burn. Gen Dent. 1995; 43:554–555.
7. De Visschere LM, Grooten L, Theuniers G, Vanobbergen JN. Oral hygiene of elderly people in long-term care institutions-a cross-sectional study. Gerodontology. 2006; 23:195–204.
8. Panácek A, Kolár M, Vecerová R, Prucek R, Soukupová J, Krystof V, Hamal P, Zboril R, Kvítek L. Antifungal activity of silver nanoparticles against Candida spp. Biomaterials. 2009; 30:6333–6340.
9. Rai M, Yadav A, Gade A. Silver nanoparticles as a new generation of antimicrobials. Biotechnol Adv. 2009; 27:76–83.
10. Sawosz E, Chwalibog A, Szeliga J, Sawosz F, Grodzik M, Rupiewicz M, Niemiec T, Kacprzyk K. Visualization of gold and platinum nanoparticles interacting with Salmonella enteritidis and Listeria monocytogenes. Int J Nanomedicine. 2010; 5:631–637.
11. Rosenberg B, Vancamp L, Krigas T. Inhibition of cell division in Escherichia coli by electrolysis products from a platinum electrode. Nature. 1965; 205:698–699.
12. Chwalibog A, Sawosz E, Hotowy A, Szeliga J, Mitura S, Mitura K, Grodzik M, Orlowski P, Sokolowska A. Visualization of interaction between inorganic nanoparticles and bacteria or fungi. Int J Nanomedicine. 2010; 5:1085–1094.
13. Onizawa S, Aoshiba K, Kajita M, Miyamoto Y, Nagai A. Platinum nanoparticle antioxidants inhibit pulmonary inflammation in mice exposed to cigarette smoke. Pulm Pharmacol Ther. 2009; 22:340–349.
14. Sur I, Cam D, Kahraman M, Baysal A, Culha M. Interaction of multi-functional silver nanoparticles with living cells. Nanotechnology. 2010; 21:175104.
15. Wang Y, Bansal V, Zelikin AN, Caruso F. Templated synthesis of single-component polymer capsules and their application in drug delivery. Nano Lett. 2008; 8:1741–1745.
16. Boomi P, Prabu HG, Mathiyarasu J. Synthesis and characterization of polyaniline/Ag-Pt nanocomposite for improved antibacterial activity. Colloids Surf B Biointerfaces. 2013; 103:9–14.
17. Hoshika S, Nagano F, Tanaka T, Ikeda T, Wada T, Asakura K, Koshiro K, Selimovic D, Miyamoto Y, Sidhu SK, Sano H. Effect of application time of colloidal platinum nanoparticles on the microtensile bond strength to dentin. Dent Mater J. 2010; 29:682–689.
18. Hoshika S, Nagano F, Tanaka T, Wada T, Asakura K, Koshiro K, Selimovic D, Miyamoto Y, Sidhu SK, Sano H. Expansion of nanotechnology for dentistry: effect of colloidal platinum nanoparticles on dentin adhesion mediated by 4-META/MMA-TBB. J Adhes Dent. 2011; 13:411–416.
19. Ma S, Izutani N, Imazato S, Chen JH, Kiba W, Yoshikawa R, Takeda K, Kitagawa H, Ebisu S. Assessment of bactericidal effects of quaternary ammonium-based antibacterial monomers in combination with colloidal platinum nanoparticles. Dent Mater J. 2012; 31:150–156.
20. Akin D, Sturgis J, Ragheb K, Sherman D, Burkholder K, Robinson JP, Bhunia AK, Mohammed S, Bashir R. Bacteriamediated delivery of nanoparticles and cargo into cells. Nat Nanotechnol. 2007; 2:441–449.
21. Goodman CM, McCusker CD, Yilmaz T, Rotello VM. Toxicity of gold nanoparticles functionalized with cationic and anionic side chains. Bioconjug Chem. 2004; 15:897–900.
22. Park MV, Neigh AM, Vermeulen JP, de la Fonteyne LJ, Verharen HW, Briedé JJ, van Loveren H, de Jong WH. The effect of particle size on the cytotoxicity, inflammation, developmental toxicity and genotoxicity of silver nanoparticles. Biomaterials. 2011; 32:9810–9817.
23. Campoccia D, Montanaro L, Arciola CR. A review of the biomaterials technologies for infection-resistant surfaces. Biomaterials. 2013; 34:8533–8554.
24. Kajita M, Hikosaka K, Iitsuka M, Kanayama A, Toshima N, Miyamoto Y. Platinum nanoparticle is a useful scavenger of superoxide anion and hydrogen peroxide. Free Radic Res. 2007; 41:615–626.
25. Sondi I, Salopek-Sondi B. Silver nanoparticles as antimicrobial agent: a case study on E. coli as a model for Gramnegative bacteria. J Colloid Interface Sci. 2004; 275:177–182.
26. Lima E, Guerra R, Lara V, Guzmán A. Gold nanoparticles as efficient antimicrobial agents for Escherichia coli and Salmonella typhi. Chem Cent J. 2013; 7:11.
27. Alvarez-Barrientos A, Arroyo J, Cantón R, Nombela C, Sánchez-Pérez M. Applications of flow cytometry to clinical microbiology. Clin Microbiol Rev. 2000; 13:167–195.
28. Pils S, Schmitter T, Neske F, Hauck CR. Quantification of bacterial invasion into adherent cells by flow cytometry. J Microbiol Methods. 2006; 65:301–310.
29. Damm C, Münstedt H, Rösch A. Long-term antimicrobial polyamide 6/silver-nanocomposites. J Mater Sci. 2007; 42:6067–6073.
30. Kumar R, Münstedt H. Silver ion release from antimicrobial polyamide/silver composites. Biomaterials. 2005; 26:2081–2088.
31. Ahn SJ, Lee SJ, Kook JK, Lim BS. Experimental antimicrobial orthodontic adhesives using nanofillers and silver nanoparticles. Dent Mater. 2009; 25:206–213.
32. Yoshida K, Tanagawa M, Atsuta M. Characterization and inhibitory effect of antibacterial dental resin composites incorporating silver-supported materials. J Biomed Mater Res. 1999; 47:516–522.
33. Imazato S, Ebi N, Takahashi Y, Kaneko T, Ebisu S, Russell RR. Antibacterial activity of bactericide-immobilized filler for resin-based restoratives. Biomaterials. 2003; 24:3605–3609.
34. Kiremitci-Gumusderelioglu M, Pesmen A. Microbial adhesion to ionogenic PHEMA, PU and PP implants. Biomaterials. 1996; 17:443–449.
35. Wang H, Qiao X, Chen J, Wang X, Ding S. Mechanisms of PVP in the preparation of silver nanoparticles. Mater Chem Phys. 2005; 94:449–453.
36. El Badawy AM, Silva RG, Morris B, Scheckel KG, Suidan MT, Tolaymat TM. Surface charge-dependent toxicity of silver nanoparticles. Environ Sci Technol. 2011; 45:283–287.
37. Silva T, Pokhrel LR, Dubey B, Tolaymat TM, Maier KJ, Liu X. Particle size, surface charge and concentration dependent ecotoxicity of three organo-coated silver nanoparticles: comparison between general linear model-predicted and observed toxicity. Sci Total Environ. 2014; 468-469:968–976.
38. Fletcher M, Loeb GI. Influence of substratum characteristics on the attachment of a marine pseudomonad to solid surfaces. Appl Environ Microbiol. 1979; 37:67–72.
39. Liu J, Hurt RH. Ion release kinetics and particle persistence in aqueous nano-silver colloids. Environ Sci Technol. 2010; 44:2169–2175.
40. Soygun K, Bolayir G, Boztug A. Mechanical and thermal properties of polyamide versus reinforced PMMA denture base materials. J Adv Prosthodont. 2013; 5:153–160.
41. Jerolimov V, Jagger RG, Milward PJ. Effect of the curing cycle on acrylic denture base glass transition temperatures. J Dent. 1991; 19:245–248.
42. Davy KW, Anseau MR, Berry C. Iodinated methacrylate copolymers as X-ray opaque denture base acrylics. J Dent. 1997; 25:499–505.
43. Aydogan Ayaz E, Durkan R, Bagis B. The effect of acrylamide incorporation on the thermal and physical properties of denture resins. J Adv Prosthodont. 2013; 5:110–117.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download