INTRODUCTION
MATERIALS AND METHODS
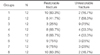
Group 1: Unaltered intact teeth without any cavity preparation were used as the negative control (G1, NC).
Groups 2-8: Endodontic access cavities were prepared with a high-speed diamond bur under constant water cooling, and the canals were instrumented with #10 to #40 K-files (Mani Inc., Tochigi, Japan) and distilled water. The canals were dried with absorbent paper points and obturated with laterally condensed gutta-percha cones (Ariadent, Tehran, Iran) and AH26 sealer (DensplyDeTrey, Konstaz, Germany). MOD cavities were prepared down to the canal orifice with the gingival margin placed 1mm apical to the cemento-enamel junction. The buccolingual width of each cavity was one-third of the intercuspal distance at the occlusal isthmus and one-third of the bucco-lingual width of the crown at two boxes with parallel walls, and the cavities extended into the pulp chamber so that axial between the proximal box and the pulp chamber was removed. Measurements were made with a digital caliper (Mitutoyo Digimatic, Mitutoyo, Kawasaki, Japan) with 0.1-mm sensitivity for proper and accurate standardization of cavity dimensions. In Group 2, MOD-prepared only, these teeth were not restored and were used as the positive control (G2, PC).
Group 3 (ComZ): All cavity surfaces were etched with 37% phosphoric acid (3M ESPE, St. Paul, MN, USA) for 15 seconds, rinsed for 20 seconds, and gently air-dried, leaving the tooth moist. Two consecutive coats of Adper Single Bond (3M ESPE) were applied and gently dried for 2 to 5 seconds, then light-cured for 10 seconds with a halogen light unit (VIP Junior, Bisco, Schaumburg, IL, USA) at 600 mW/cm2 light intensity. The cavities were then restored with a methacrylate- based composite (Z250, 3M ESPE) using an oblique incremental technique. Each layer was placed at 1.5 mm thickness and cured for 40 seconds with the same unit.
Group 4 (FRCZ): After etching and bonding similar to Group 3, a flowable composite (Filtek Flow, 3M ESPE) coated the cavity surfaces. Before curing, a piece of polyethylene ribbon fiber (3 mm width, 6.5 mm long) (Ribbond Inc., Seattle, WA, USA) was cut and saturated with resin and then embedded inside the flowable composite coated buccal and lingual walls and cavity floor in a buccal to lingual direction (u-shaped) from the occlusal one-third of the buccal wall to the occlusal one-third of the lingual wall. After curing for 20 seconds, the cavities were restored with Z250 composite as performed in Group 3.
Group 5 (ComS): The self-etching primer of Silorane Adhesive System (3M ESPE, St. Paul, MN, USA) was applied to the cavity for 20 seconds and gently air dried for 10 seconds, and light-cured for 10 seconds. Bond was applied and light-cured for 10 seconds. Silorane-based composite (Filtek P90, 3M ESPE, St. Paul, MN, USA) was applied and cured similar to Z250 in Group 3.
Group 6 (FRCS): After bonding procedures in the same manner as described in Group 5, the cavity was coated with a layer of the preheated (at 55℃) silorane composite. Immediately, the prepared fiber similar to Group 4 was embedded inside the preheated silorane composite. Similar to Group 5, the restoration was completed.
Group 7 (NI/ComZ): Nano ionomer primer (Ketac Nano primer, 3M ESPE) was applied for 15 seconds, air dried, and light-cured for 10 seconds; then two pastes (Ketac N 100) were mixed and placed above the gutta-percha to reproduce the floor and axial wall of the MOD cavity in vital teeth. The cavity was restored with Z250 similar to Group 3.
Group 8 (NI/ComS): Ketac N100 was applied as described for Group 7 and the restoration was completed with silorane composite similar to Group 5. The eight groups were presented in Fig. 1.
RESULTS
DISCUSSION
CONCLUSION
All restorative treatments significantly increased fracture resistance of maxillary premolars compared to cavity-prepared one.
The fiber insertion revealed no additional positive effect on the strength of the restored teeth using methacrylate- and silorane-based composites; however, it increased restorable fracture of methacrylate-based restored teeth.
The use of NI core under methacrylate-based composite had a positive effect on fracture resistance and fracture line.
Only FRCS restored teeth revealed a similar strength to that of the intact teeth; however, the other restorative materials except for methacrylate-based composite with or without fiber exhibited comparable results to FRCS in terms of resistance.




 PDF
PDF ePub
ePub Citation
Citation Print
Print






 XML Download
XML Download