Abstract
PURPOSE
The aim of this in vitro study was to evaluate the effect of aging on the tear strength and cytotoxicity of four soft denture lining materials.
MATERIALS AND METHODS
Four commonly used soft denture lining materials, (Coe-Comfort™ GC America Inc., Alsip, IL, USA; Coe-Soft™ GC America Inc., Alsip, IL, USA; Visco-gel Dentsply Caulk Milford, DE, USA; and Sofreliner Tough M Tokuyama Dental Corporation Tokyo, Japan) were selected. Sixty trouser-leg designed specimens per lining material were fabricated using a stainless steel mold for tear strength testing. The specimens were divided into non-thermocycling and 1000-, and 3000- thermocycling groups. For the cytotoxicity test, twenty-four disk shaped specimens per material were fabricated using a stainless steel mold. The specimens were soaked in normal saline solution for 24 h, 48 h and 72 h. Cytotoxicity was measured by XTT assay in L929 mouse fibroblasts. Data were analyzed by two way analysis of variance and Dunnett's test (P<.05).
RESULTS
Before thermocycling, Sofreliner Tough M (10.36 ± 1.00 N) had the highest tear strength value while Coe-Comfort™ (0.46 ± 0.10 N) had the lowest. After 3000 cycles, Sofreliner Tough M (9.65 ± 1.66 N) presented the highest value and Coe-Comfort™ (0.42 ± 0.08 N) the lowest. Sofreliner Tough M, in all incubation periods was the least toxic with significant differences compared to all other materials (P<.05). Coe-Comfort™, Coe-Soft™, and Sofreliner Tough M did not show any significant differences within their material group for all incubation periods.
Chairside soft denture lining materials are becoming a valuable resource especially for dentists practicing prosthodontics and implants. Because of their viscoelastic property, these materials can act as shock absorbers and help distribute and reduce stresses on denture-bearing areas.1
The major characteristics for soft lining materials are high dimensional stability, adequate tear resistance, permanent resiliency, lack of odor and taste, ease of cleaning, adhesion to denture base and biocompatibility.2 With chairside denture lining materials, a direct technique is applied where uncured relining material is placed in the patient's mouth and auto-polymerized.3,4 Since denture liners are in direct contact with oral tissue, they have to be non-irritating, non-toxic, and incapable of supporting bacterial and fungal colonization.5,6
As time passes, the properties of soft liners can change as some ingredients may leach out from the material or extrinsic elements may be incorporated into the material.7 These materials may become more rigid and inelastic due to loss of plasticizer, thereby removing the most important characteristic physical property of a resilient denture liner which is the elastic modulus.8
Evaluating the biocompatibility of a material is a vital step towards its acceptance in addition to testing of the material's physical properties.9 Park et al.10 evaluated the cytotoxicity of short-term use soft liners after repeated elution. Their results showed decreased cytotoxicity of the tested materials after repeated elution. Another study by Ozdemir et al.7 evaluated five commonly used soft lining materials and the study results showed that all tested materials had various degrees of cytotoxicity, especially at 96-hour test period. A systematic review by Chaves et al.11 provided some evidence that heat-polymerized resins had lower cytotoxic effects than autopolymerizing denture acrylic resins and light-polymerized reline resins. Although the study evaluated cytotoxicity, the materials utilized were hard denture lining materials since only a few studies have been undertaken regarding the cytotoxicity of soft denture lining materials.12 Thus, the aim of this in vitro study was to evaluate the effect of aging on four soft denture lining materials in terms of cytotoxicity and tear strength.
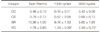
Four commonly used soft lining materials were utilized for tear strength and cytotoxicity testing (Coe-Comfort™ GC America Inc., Alsip, IL, USA; Coe-Soft™ GC America Inc., Alsip, IL, USA; Visco-gel Dentsply Caulk Milford, DE, USA; and Sofreliner Tough M Tokuyama Dental Corporation Tokyo, Japan) (Table 1).
Sixty trouser-leg designed test specimens per lining material (240 specimens total) were fabricated using a stainless steel mold with dimensions of 50 mm long, 10 mm wide, and 1 mm thick (Fig. 1). The stainless steel mold was placed on a glass slide and each material was mixed according to the manufacturers' instructions. By the use of a disposable plastic syringe, the material was injected into the stainless steel mold. An additional glass slide was placed on top of the mold and firm hand pressure was applied to remove the excess material and the material was polymerized according to the manufacturers' instr uctions. Specimens were cut vertically (25 mm long) with a number 15 blade to form the trouser leg design. The 60 specimens per lining material were divided into three groups (20 specimens per group), non-thermocycling, 1000-thermocycling, and 3000-thermocycling group. The 1000- and 3000-cycle groups of all the lining materials were subjected to thermal cycling with a dwelling time of 30 seconds and a resting time of 6 seconds with temperatures of 5℃ and 55℃. Mechanical testing was performed on a universal testing machine (Shimadzu AG10KNX, Tokyo, Japan) at a crosshead speed of 50 mm/min.
Testing of cytotoxicity and preparation of test specimens were executed in accordance with ISO 10993-5.13 Twenty-four disk specimens per lining material (96 specimens total) were fabricated using a stainless steel mold with dimensions of 10 mm diameter and 1 mm thickness (Fig. 2). The specimens were soaked in normal saline solution after final setting. The specimens were grouped in accordance to aging or incubation period (6 specimens per group), 0, 24, 48, and 72 hours, and stored at 37℃ in an atmosphere of 5% CO2. The specimens were transferred into a 24-well cluster culture plate and washed with phosphate buffered saline (PBS) and kept under ultraviolet light to avert bacterial contamination.14
L929 mouse fibroblasts (Korea cell line bank) were used to determine the cytotoxicity of the soft denture lining material. The L929 cell suspension was prepared at a concentration of 5 × 104 cells/mL and was dispensed into a 24-well cluster culture plate with direct contact with the specimens. Cells in pure culture medium were used as a control group.
The cells were grown as a monolayer culture in a cell culture dish at 37℃ in an atmosphere of 5% CO2, sub cultured two times a week, and maintained at the third passage. The culture medium used was Roswell Park Memorial Institute (RPMI) 1640 (Gibco®Life Technologies Corporation, Grand Island, NY, USA) supplemented with 10% fetal bovine serum (FBS) and 1% antibiotic-antimycotic. Adherent cells at the logarithmic phase were detached with 0.25% trypsin-ethylenediaminetetraacetic acid (EDTA) (Gibco®Life Technologies Corporation, Grand Island, NY, USA) and were incubated for 1 minute at 37℃.
The cell Proliferation Kit II (Roche, Mannheim, Germany) was used for the XTT assay. XTT labeling reagent and electron-coupling reagent were thawed in a water bath at 37℃. The vials were thoroughly mixed until clear solutions were obtained. 5 mL of XTT labeling reagent was mixed with 0.1 mL of electron coupling reagent on a dark, clean bench. A 250 µL volume of XTT labeling mixture was added per well in the 24-well cluster culture plate and the plate was incubated for 3 hours at 37℃ and 5% CO2. After incubation, 150 µL of mixture per well were aspirated and transferred to a 96-well cluster culture dish. The spectrophotometrical absorbance of the samples was measured using a microplate enzyme-linked immunosorbent assay (ELISA) reader. The wavelength used to measure the optical density (OD) of the absorbance of the formazan product was 450 nm, according to the filters available for the ELISA reader used. Cell viability and cell cytotoxicity were calculated in percentage of control groups according to the following modified formula:15
Cell cytotoxicity (%) = 100 - Cell viability (%) = (OD of the test group / OD of the control group) × 100
Cell viability was the scored according to the following classification:
Data were analyzed by two-way analysis of variance for group comparison and one-way analysis of variance for individual group comparisons using IBM SPSS version 20.0 (IBM SPSS Statistics for Windows, Version 20.0 Armonk, NY, USA). The means and standard deviations were recorded for both tests and significant differences of the results and between groups were analyzed using Dunnett's test (P<.05).
Table 2 shows the numerical tear strength test results and the same information is shown graphically in Fig. 3. Before thermocycling, Sofreliner Tough M (10.36 ± 1.00 N) had the highest tear strength value while Coe-Comfort™ (0.46 ± 0.10 N) had the lowest. After 3000 cycles Sofreliner Tough M (9.65 ± 1.66 N) still presented the highest value and Coe-Comfort™ (0.42 ± 0.08 N) the lowest. The results were significantly different from those of the other materials (P<.05). After 3000 cycles of thermocycling Coe-Comfort™, Coe-Soft™, and Sofreliner Tough M did not show any significant differences compared to their nonthermocycling and 1000-cycle groups (P<.05). With Viscogel, the tear strength value went down after 1000 cycles, compared to the non-thermocycling group, but the difference was not significant. After 3000 cycles of thermocycling, the tear strength value was significant when compared to the 1000 cycle group (P<.05).
Table 3 shows the numerical cytotoxicity test results and this information is shown graphically in Fig. 4. Sofreliner Tough M, in all incubation periods was least toxic and showed significant differences compared with all other materials (P<.05). Coe-Comfort™, Coe-Soft™, and Sofreliner Tough M did not have any significant differences across all incubation periods when compared to their respective groups (P<.05). With Visco-gel, after soaking for 24 hours, the cytotoxicity of the material decreased and showed a significant difference compared to its non-soaking group (P<.05). For Visco-gel in the 24-, 48-, and 72-hour groups, although the values changed, the changes were not significant (P<.05).
Temporary soft relining material can be used for a short period of time to improve the comfort and fit of dentures until they can be remade or permanently relined. These materials take the anatomy of the residual ridge and gel in that position and continue to flow slowly after application and distribute stress on denture-bearing tissues.4,16,17
Soft denture lining materials are mainly made up of polyethyl or polymethyl methacrylate resin with a plasticizer such as dibutyl phthalate or ethanol. Being low molecular weight compounds, these plasticizers are usually leached out in the saliva over a period of time. This leaching out of the plasticizers may result in reductions in softness of the material and also, since it is in direct contact with the oral mucosa, may cause adverse reactions like allergies and local chemical irritation.8,11
Biologic and toxicologic aspects of dental materials are important in relation to their clinical usage.18 Cytotoxicity is used to describe the cascade of molecular events that interfere with macromolecular synthesis, causing disruption of cellular functions and structural damage.7 Cell culture studies are usually the preliminary point of an evaluation of biocompatibility. In vitro cytotoxicity tests are a essential screening step in the testing of new materials used in humans because they provide an investigation of toxicity in a simplified system that reduces the effects of confounding variables.19,20 Testing of dental materials by cell culture methods is relatively simple to perform, reproducible, and cost-effective and such tests can be controlled.14
The choice of cell line for in vitro cytotoxicity testing remains controversial and a vast number of cell lines have been used.21 Continuous cell lines, like 3T3 or L929 mouse fibroblasts, are suggested by international standards for the testing of medical devices used in dentistry because of the ease of controlling cell conditions.13,22 Thonemann et al.23 indicated that L929 mouse fibroblasts are more sensitive than primary human gingival fibroblasts and differences in the responses of the cell types depend on the dental material tested. In this study, cytotoxicity was measured using a direct method which permits a more legitimate comparison between aging intervals as each set of specimens is statistically independent.24
To evaluate potential of such materials to cause irritation, the XTT colorimetric assay is applicable. XTT offers a high degree of sensitivity, while providing a considerable savings in time and labor by eliminating the need to solubilize the formazan product prior to absorbance measurements thus making it quick, easy and safe to perform.25,26 Since leaching of unreacted monomer causes a reduction in the softness of soft denture lining materials and happens intraorally during function, various accelerated aging methods have been applied to these materials to simulate oral conditions.1,10,27,28,29,30,31 By means of thermocycling, cumulative effects of fatigue arising from sudden temperature changes can be determined. In this current study, temperature variation between 5℃ and 55℃ was chosen as these temperatures depict the temperature range of foods ingested during meals and do not damage oral tissues.29 As to the use of 1000 and 3000 thermal cycles, the objective was to evaluate the cumulative effect of fatigue within soft denture liner materials rather than to represent a certain wearing time for soft denture liners.32
After subjecting Coe-Comfort™ and Coe-Soft™ to thermocycling, the tear strength of the materials was not affected after 3000 cycles. Although the values changed from non-thermocycling to 1000 cycles to 3000 cycles, statistically, the tear strength values did not have any significant differences when compared to each other. According to previous studies, leaching of plasticizers could affect the softness of the material, however with Coe-Comfort™ and Coe-Soft™ the tear strength was not affected. This result is supported by a study by Munksgaard et al.12 that investigated Coe-Comfort™, which is composed mainly of benzyl benzoate, and Coe-Soft™, which is composed mainly of benzyl salicylate. The results of these experiments showed that leaching of plasticizers happens from 1 day up to 30 days. Between 40% and 64% of the plasticizers found in the materials leached out within 30 days. The cumulative amount of plasticizers that had leached out in 30 days from each of the materials was between 128 mg g-1 and 253 mg g-1.
However this leaching of plasticizers not only affects the physical properties of the materials but also, according to past studies, may cause local irritation on the mucosa. In this current study, it was observed that both Coe-Comfort™ and Coe-Soft™ were toxic even after 72 hours (3 days) of soaking in normal saline solution. This result can also be related to the study by Munksgaard12, which showed that in 30 days there were still plasticizers leaching from the materials tested.
Different results were observed for Visco-gel. We saw that after subjecting the material to 3000 cycles of thermocycling, there was a significant difference in tear value when compared to its 1000 cycle result. We also saw that after soaking the material for 24 hours in normal saline solution, there was a significant decrease in cytotoxicity when compared to the results of the non-soaking group. Visco-gel, which is composed of phthalyl butyl glycolate has a different composition than that of Coe-Comfort™ and Coe-Soft™. This result can be supported by the study of Murata et al.33 which found that benzyl salicylate, being a larger molecule, would be expected to leach out more slowly than phthalyl butyl glycolate. According to Shanmuganathan et al.8, loss of a plasticizer like phthalyl butyl glycolate produced a more significant change in compliance than loss of benzyl salicylate.
Sofreliner Tough M gave the highest tear strength value and was the least toxic among all the materials tested. These results are supported by the study by Ciapetti et al.34 which found that among soft liners, which are similar to different silicone impression materials, vinyl poly siloxanes are nontoxic even when tested after extended exposure to cells.
Within the limitations of this in vitro study, it can be concluded that the tear strength of soft lining material depends on the type of plasticizer used. However, these factors can also contribute to toxicity over a long period of time. After interpretation of the gathered results the following conclusions were made:
Coe-Comfort™ had the lowest tear strength and the highest cytotoxicity in all incubation period.
The tear strength of Coe-Soft™ was not affected significantly by thermocycling but presented severe cytotoxicity in all incubation periods.
After 3000 cycles of thermocycling, Visco-gel showed significant increase in tear strength. Cytotoxicity significantly decreased after 24 hours of soaking and presented slight cytotoxicity after 72 hours of soaking.
Sofreliner Tough M, a silicone type soft lining material, had the highest tear strength and presented the lowest cytotoxicity.
Figures and Tables
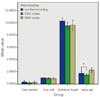 | Fig. 3Mean tear strength values for non-thermocycling, 1000, and 3000 cycle group. *significant difference (P<.05). |
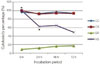 | Fig. 4Percentage of material cytotoxicity at 0 h, 24 h, 48 h and 72 h incubation period.
CC: Coe-Comfort™, CS: Coe-Soft™, SR: Sofreliner Tough M, VG: Visco-gel. *significant difference (P<.05).
|
Table 1
Four commonly used soft denture lining materials utilized for tear strength and cytotoxicity test

References
1. Sertgöz A, Kulak Y, Gedik H, Taskonak B. The effect of thermocycling on peel strength of six soft lining materials. J Oral Rehabil. 2002; 29:583–587.
2. Pesun IJ, Hodges J, Lai JH. Effect of finishing and polishing procedures on the gap width between a denture base resin and two long-term, resilient denture liners. J Prosthet Dent. 2002; 87:311–318.
3. Murphy WM, Huggett R, Handley RW, Brooks SC. Rigid cold curing resins for direct use in the oral cavity. Br Dent J. 1986; 160:391–394.
4. Qudah S, Harrison A, Huggett R. Soft lining materials in prosthetic dentistry: a review. Int J Prosthodont. 1990; 3:477–483.
5. Anusavice KJ. Phillips' science of dental materials. St. Louis; Mo.: WB Saunders;2003.
6. Causton BE. Denture base polymers and liners. In : O'Brian WJ, editor. Dental materials and their selection. Chicago: Quintessence;1997. p. 90–92.
7. Ozdemir KG, Yilmaz H, Yilmaz S. In vitro evaluation of cytotoxicity of soft lining materials on L929 cells by MTT assay. J Biomed Mater Res B Appl Biomater. 2009; 90:82–86.
8. Shanmuganathan N, Padamanabhan TV, Subramaniam R, Madhankumar S. The compliance of temporary soft lining materials-an in vivo & vitro study. Int J Sci Res Publ. 2012; 2:1–7.
9. Polyzois GL, Hensten-Pettersen A, Kullmann A. An assessment of the physical properties and biocompatibility of three silicone elastomers. J Prosthet Dent. 1994; 71:500–504.
10. Park SK, Lee YK, Lim BS, Kim CW. Changes in properties of short-term-use soft liners after thermocycling. J Oral Rehabil. 2004; 31:717–724.
11. Chaves CA, Machado AL, Vergani CE, de Souza RF, Giampaolo ET. Cytotoxicity of denture base and hard chairside reline materials: a systematic review. J Prosthet Dent. 2012; 107:114–127.
12. Munksgaard EC. Leaching of plasticizers from temporary denture soft lining materials. Eur J Oral Sci. 2004; 112:101–104.
13. International Standards Organization (ISO). 10993-5:1992. Biological evaluation of medical devices - Part 5: Tests for in vitro cytotoxicity. Geneva; Switzerland: International Standards Organization;1992.
14. Hensten-Pettersen A. Comparison of the methods available for assessing cytotoxicity. Int Endod J. 1988; 21:89–99.
15. Heravi F, Ramezani M, Poosti M, Hosseini M, Shajiei A, Ahrari F. In Vitro Cytotoxicity Assessment of an Orthodontic Composite Containing Titanium-dioxide Nano-particles. J Dent Res Dent Clin Dent Prospects. 2013; 7:192–198.
16. Jepson NJ, McCabe JF, Storer R. Evaluation of the viscoelastic properties of denture soft lining materials. J Dent. 1993; 21:163–170.
17. Lytle RB. Complete denture construction based on a study of the deformation of the underlying soft tissues. J Prosthet Dent. 1959; 9:539–551.
18. Mjör IA. Biologic assessment of restorative dental materials: interrelationship of biologic and technologic properties. Oper Dent. 1978; 3:9–13.
19. Huang FM, Tai KW, Hu CC, Chang YC. Cytotoxic effects of denture base materials on a permanent human oral epithelial cell line and on primary human oral fibroblasts in vitro. Int J Prosthodont. 2001; 14:439–443.
20. Lefebvre CA, Schuster GS. Biocompatibility of visible lightcured resin systems in prosthodontics. J Prosthet Dent. 1994; 71:178–185.
21. Hanks CT, Strawn SE, Wataha JC, Craig RG. Cytotoxic effects of resin components on cultured mammalian fibroblasts. J Dent Res. 1991; 70:1450–1455.
22. International Standards Organization (ISO). ISO 7405:1997. Pre clinical evaluation of biocompatibility of medical devices used in dentistry: Test methods for dental materials. Geneva; Switzerland: International Standards Organization;1997.
23. Thonemann B, Schmalz G, Hiller KA, Schweikl H. Responses of L929 mouse fibroblasts, primary and immortalized bovine dental papilla-derived cell lines to dental resin components. Dent Mater. 2002; 18:318–323.
24. Bouillaguet S, Shaw L, Gonzalez L, Wataha JC, Krejci I. Long-term cytotoxicity of resin-based dental restorative materials. J Oral Rehabil. 2002; 29:7–13.
25. Roehm NW, Rodgers GH, Hatfield SM, Glasebrook AL. An improved colorimetric assay for cell proliferation and viability utilizing the tetrazolium salt XTT. J Immunol Methods. 1991; 142:257–265.
26. Stevens MG, Olsen SC. Comparative analysis of using MTT and XTT in colorimetric assays for quantitating bovine neutrophil bactericidal activity. J Immunol Methods. 1993; 157:225–231.
27. Dootz ER, Koran A, Craig RG. Physical property comparison of 11 soft denture lining materials as a function of accelerated aging. J Prosthet Dent. 1993; 69:114–119.
28. Hekimoğlu C, Anil N. The effect of accelerated ageing on the mechanical properties of soft denture lining materials. J Oral Rehabil. 1999; 26:745–748.
29. León BL, Del Bel Cury AA, Rodrigues Garcia RC. Water sorption, solubility, and tensile bond strength of resilient denture lining materials polymerized by different methods after thermal cycling. J Prosthet Dent. 2005; 93:282–287.
30. Pinto JR, Mesquita MF, Nóbilo MA, Henriques GE. Evaluation of varying amounts of thermal cycling on bond strength and permanent deformation of two resilient denture liners. J Prosthet Dent. 2004; 92:288–293.
31. Qudah S, Huggett R, Harrison A. The effect of thermocycling on the hardness of soft lining materials. Quintessence Int. 1991; 22:575–580.
32. Oguz S, Mutluay MM, Dogan OM, Bek B. Effect of thermocycling on tensile strength and tear resistance of four soft denture liners. Dent Mater J. 2007; 26:296–302.
33. Murata H, Iwanaga H, Shigeto N, Hamada T. Initial flow of tissue conditioners-influence of composition and structure on gelation. J Oral Rehabil. 1993; 20:177–187.
34. Ciapetti G, Granchi D, Stea S, Savarino L, Verri E, Gori A, Savioli F, Montanaro L. Cytotoxicity testing of materials with limited in vivo exposure is affected by the duration of cell-material contact. J Biomed Mater Res. 1998; 42:485–490.




 PDF
PDF ePub
ePub Citation
Citation Print
Print





 XML Download
XML Download