Abstract
PURPOSE
The purpose of this study was to to analyze the effect of Type 2 diabetes on tooth mortality, implant treatment and prosthetic status.
MATERIALS AND METHODS
275 Type 2 diabetics and 300 non-diabetics, aged 40-80 years were selected for analysis. The assessment of number of teeth, missing teeth, fixed prostheses (bridge pontics), implants using panoramic radiographs and dental records were carried out.
RESULTS
Diabetes mellitus (DM) patients had a higher number of missing teeth (P<.05) and placed implants (P=.074), age (P<.05), male gender percentage (P=.042), smoker percentage (P<.05) than non-DM patients. In univariate analysis, the patients in older group showed significantly higher number of tooth loss rate at the first dental examination than the patients in younger group. Tooth loss rate of smokers did not show higher value than that of non-smokers. When multiple variables including DM, age, smoking, gender were considered together, diabetics and older group patients showed significantly higher tooth loss rate at the first dental examination than non-diabetics and younger group patients, respectively. Smokers and male group did not show a significant difference than non-smokers and female group, respectively.
CONCLUSION
Tooth mortality and implant treatment rate were significantly higher in the DM group as indicated by univariate and multivariate logistic regression analysis. Old age groups showed significantly higher odds ratios and tooth loss rate. As diabetics showed the higher tooth loss rate than non-diabetics, diabetics also had more implant restorations than non-diabetics.
Diabetes mellitus (DM) comprises a group of metabolic diseases characterized by hyperglycemia, resulting from insulin disturbance. The prevalence of diabetes is increasing worldwide and varies depending on age and race. Although increased number of new patients is diagnosed with diabetes, the seriousness of diabetic complications is not fully appreciated yet. Approximately 85-90% of diabetic cases are diagnosed with Type 2 diabetes and results from insulin resistance. Altered insulin production and insulin resistance state in Type 2 diabetics cause impairment of metabolic balance and uncontrolled or poorly controlled diabetes in their health status is associated with increased susceptibility to oral infections and poor wound healing.
Oral manifestations of diabetic patients take on a more diverse aspect. High risk of dental caries resulting from salivary dysfunction such as xerostomia,1 a greater likelihood of oral mucosal disorders such as lichen planus, recurrent aphthous stomatitis and candidiasis was reported.2-4 Also, some studies have reported that diabetic patients had more denture stomatitis and candidiasis than non-diabetics.5,6 Diabetic patients may have abnormal modifying factors in soft tissue and these soft tissue manifestations should be perceived in diabetic patients who require teeth and prosthetic restorations.
Diabetic patients are more susceptible to tooth loss than non-diabetic patients due to higher risk for periodontitis. Diabetes mellitus and periodontal disease have been considered to be biologically associated. Epidemiologic researches suggests that diabetes increases the risk of periodontal disease, resulting in increased severity of periodontitis.7,8 The relationship among diabetes mellitus, periodontal state, and subsequent tooth loss has also been reported. A case-control study showed that Type 2 diabetics had a significantly lower number of teeth present9 and a study of prognostic model for tooth survival suggested diabetes mellitus as a significant indicator for tooth loss10 There is ample evidence of the biological and epidemiological association between periodontal disease and diabetes, especially, Type 2 diabetes mellitus.11,12
The influence of diabetic condition on periodontium and oral manifestations has been reported in several articles. An explanation for increased infection susceptibility of diabetic patients is that impaired chemotaxis and defective phagocytosis or impaired adherence were caused by polymorphonuclear leukocyte (PMN) deficiencies. Moreover, the increased severity of periodontal disease in diabetic environment may reflect an alteration in the pathogenic potential of bacteria13 and increased expression of marker of systemic inflammation such as circulating C-reactive protein (CRP), enhancing a breakdown of periodontal tissues, resulting in more frequent and severe periodontal-tissue destruction.14 Several articles reported that mechanisms underlying the advanced periodontal disease associated with diabetes appear to reflect abnormal host responses.15-18 Such relationship is similar to the relationship between glycemic control and the classic complications of diabetes mellitus; nephropathy, retinopathy and altered wound healing.
In this way, diabetic patients with periodontal disease, one of the most common dental problems tend to have more tooth loss. Consequently, they require diverse and effective restoration and prosthetic modality including fixed, removable and implant treatment.
Prior to implant placement, implant site drilling procedure is performed and both bone necrosis and remodeling process are required Stable blot clot formation between the placed implant and adjacent bone is essential for new osteogenic cell population.19 Hyperglycemic state in diabetic patients may reduce clot quality due to poor, ineffective cell adhesion and abnormal collagen remodeling. So, biomechanical retention must be considered more carefully for the implant restoration of these patients.
The objective of this cross-sectional study was to analyze effect of Type 2 diabetes on tooth mortality, implant treatment and prosthetic status among patients with and without diabetes mellitus.
The subject samples were recruited from patients referred to the Department of Periodontology, Kyungpook National University Dental Hospital for treatment of chronic periodontitis between June 2009 and December 2012. Subjects with missing data for dental examinations, smoking, age, and gender were excluded. Finally, 275 subjects with Type 2 diabetes mellitus and 300 non-diabetic (control) aged 40-80 years were available for analyses.
Patients had received periodontal treatment (with surgical treatment if required) and have been on a recall schedule for supportive periodontal therapy since completing active treatment. Frequency of recalls was determined by the patient's periodontal health and oral hygiene status.
Diabetes was diagnosed when the level of fasting plasma glucose is more than 126 mg/dl or the level of two-hour postprandial glucose is more than 200 mg/dl. (American dental association: Diabetes Care 26 (supppl 1): 5, 2003) Diabetic patients were referred from Department of Endocrinology, Kyungpook National University Dental Hospital. The study protocol was reviewed and accepted by the Research Ethics Committee, Kyungpook National University (Ethics Reference No. KNUH2012-06-023-001).
Clinical examinations were conducted, including the assessment of number of teeth (third molars were excluded from the analysis), missing teeth, fixed (bridge pontics) prostheses, implants using panoramic radiographs and dental records. At the patient's first visit, the number and type of missing teeth, implants, fixed prostheses were surveyed. Extracted teeth and placed implants were also surveyed during treatment period. Confounding factors such as cigarette smoking, age, gender were assessed.
Continuous data were expressed as mean and standard deviation and comparisons between groups were performed using the independent t-test. Nominal data were presented as absolute numbers and percent values and comparisons between groups were performed using the chi-square test. For logistic regression model analysis about the number of lost teeth, the patients with 5 or more teeth loss were designated as having higher teeth loss rate. Five teeth loss was the highest quartile in the number of lost teeth.
General characteristics of the patients investigated in this study are shown in Table 1.
A total of 275 DM patients were surveyed in the study. The mean age of patients was 60.3 ± 9.36 years (41-80 years). At the first dental examination, the number of lost teeth in all patients and per patient was 1292 and 4.70 ± 5.29, respectively. The number of placed implants in all patients and per patient was 129 and 0.46 ± 1.45, respectively. The number of fixed partial dentures in all patients and per patient was 233 and 0.84 ± 1.03, respectively. During active treatment period, the number of extracted teeth in all patients and per patient was 163 and 0.59 ± 1.40, repectively.
A total of 300 non-DM patients were surveyed in the study. The mean age of patients was 56.4 ± 9.70 years (40-80 years). At the first dental examination, the number of lost teeth in all patients and per patient was 841 and 2.80 ± 3.62, respectively. The number of placed implants in all patients and per patient was 82 and 0.27 ± 1.04, respectively. The number of fixed partial dentures in all patients and per patient was 249 and 0.83 ± 1.10, respectively. During active treatment period, the number of extracted teeth in all patients and per patient was 149 and 0.49 ± 1.45, respectively.
DM patients and control patients did not show a significant difference in the number of placed implants, fixed partial dentures at the first dental exam and the number of lost teeth during active treatment period. However, these two groups showed a significant difference in age, male gender, smoker ratio and number of lost teeth at the first dental exam.
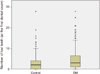
DM patients had a higher number of missing teeth (P<.05), age (P<.05), male gender percentage (P=.042), smoker percentage (P<.05) than control patients. In box plot analysis, DM patients also showed probability of high tooth loss than non-diabetics (Fig. 1).
DM patients showed significantly higher number of tooth loss rate at the first dental exam than non-DMc patients (Table 2). In addition, the patients in older group showed significantly higher number of tooth loss rate at the first dental examination than the patients in younger group. In contrast to previously demonstrated reports, the tooth loss rate of smokers did not show the higher value than that of non-smokers, but the difference was not statistically significant. Also, male group showed slightly lower tooth loss rate than female group, but did not show a significant result.
When multiple variables including diabetes mellitus, age, smoking, gender were considered together, odds ratios about diabetes mellitus and age were slightly decreased and odds ratios about smoking and gender were slightly increased (Table 3). Diabetics and older group patients showed significantly higher tooth loss rate at the first dental exam than non-diabetics and younger group patients, respectively. Smokers and gender group did not show a significant difference than non-smokers and female group, respectively.
The high level of glucose in the gingival crevicular fluid and blood stream of diabetics could change the environment of the bacterial flora, inducing qualitative changes in microbial community. This could contribute to the severity of periodontal disease and tooth loss. Also, such chronic hyperglycemia may impair the integrity of the tissues of the periodontium. An animal study reported that bone loss pattern in diabetic mice presented rougher and more irregular at crestal area and slightly greater than non-diabetic mice. They suggested that diabetes mellitus may affect independently on periodontal tissue destruction and tooth loss irrespective of the presence or absence of periodontal disease.20 As a result of the chronic hyperglycemia, the formation of AGEs (accumulated glycation end-products), which is a specific characteristic of diabetes, induces marked changes in cells and extracellular matrix components and makes the periodontium of diabetics vulnerable to the periodontal inflammation.21
The present study supports previous several studies reporting a significant association between diabetes mellitus and tooth loss, implant treatment. Tooth loss was evaluated as an indicator and consequence of destructive periodontal disease in several studies. When the number of lost teeth due to periodontal disease was evaluated at the first dental exam, DM patients were more likely to have periodontal disease defined by tooth loss due to periodontitis. Tooth loss due to periodontal disease could be identified by asking patients about the cause of tooth extraction such as tooth mobility or gingival problem. The comparison of DM and control subjects at first dental examination allows us to observe that the level of periodontal disease and tooth loss were significantly higher in the DM group and also indicates that prevalence of periodontitis is higher in diabetic patients than in non-diabetics. In fact, those periodontitis patients with DM visited our periodontal clinic first with multiple tooth loss, which means there was insufficient awareness of diabetic mellitus as well as periodontal disease that may have resulted in severe periodontal destruction. It is re-emphasized that periodontal disease is a major universal health problem affecting the majority of the adult population after the age of 35-40 years22 and as periodontal disease is designated as the sixth complications of diabetes,23 prevalence and severity of periodontitis typically were increased in diabetic patients.
Age is a important confounding factor on the risk of periodontal disease,24 and the prevalence of periodontal disease increases with age. Studies of risk factors for periodontal disease point out age, smoker as patient-related factors.25 As people ages, the ability of host defense mechanism may decrease with increase in the influence of accumulated periodontal destruction resulting in gradual tooth loss. Another epidemiologic study also suggested that specific bacteria played an important role in older adults with periodontal disease.26 In both univariate and multivariate logistic regression analysis of this study, old age groups showed significantly higher odds ratios and higher tooth loss rate. The comparison between smokers and non-smokers did not show such result as expected. Possible explanation for this result is former smoker was not identified. As all subjects were classified into only smokers and non-smokers, a certain number of former smokers could belong to non-smoker group. Adjusted odds ratios about smokers was nearby one, cautiously suggesting that odds ratios could increase more after the effect of former smokers was offset in non-smokers group.
In this study, the duration and the age of onset of diabetes were not evaluated. Thorstensson and Hugoson27 analysed periodontal disease experience in 40- to 70-year old, sex-matched 83 insulin-dependent diabetics and 99 non-diabetics. They reported that the age of onset appears to be an important risk factor for future periodontal destruction. But, Soskolne concluded that for both insulin-dependent diabetes mellitus and non-insulindependent diabetes mellitus, there did not appear to be any correlation between the prevalence of the severity of periodontal disease and the duration of diabetes.28 As age and duration of diabetes may interact in periodontal disease, appropriate study model for evaluating the influence of the duration of diabetes are required.
Although the number of lost teeth during active periodontal treatement was slightly higher in diabetics than in non-diabetcs, the difference was not statistically significant. As most patients visit periodontal clinic to save or treat their teeth with moderate-severe periodontal destruction, the extraction of hopeless tooth during initial therapy was not ordinary and two groups did not show a significant difference. Though the evaluation of tooth extraction during supportive periodontal therapy was required, supportive periodontal therapy period was not sufficient enough to evaluate tooth loss rate. The relationship between periodontal health and diabetes has been described as interactive29 ; periodontitis have an adverse effect on glycemic control and diabetes also have an adverse effect on periodontal health30,31 and studies demonstrates that periodontal treatment in diabetics could improve metabolic state.32-34 Colonized gram-negative anaerobic microorganisms in severe periodontal lesions may disturb glycemic control in blood stream35 and these conditions trigger diabetic complications. Grossi et al. in their continuous studies reported that the elimination of periodontal infection improved the concentration of glycosylated hemoglobin (HbA1c) levels in response to periodontal therapy.36,37 Extension of our study to evaluate if active periodontal treatment and subsequent supportive periodontal therapy can improve glycemic state to some degree will also be a stimulating result.
The relationship between periodontitis and diabetes should be considered from another point of view. It is the long-term metabolic control of the diabetes. In our study, control status of the diabetic condition was not assessed although most patients have received periodontal treatment in our clinic under controlled glycemic state. As it is commonly believed that diabetic patients with poorly-controlled state have a higher prevalence and more aggressive periodontitis than well-controlled diabetics, this is one more important point.
In our study, as diabetics showed the higher tooth loss rate than non-diabetics, diabetics also had more implant restorations than non-diabetics. The number of fixed partial dentures did not show a significant difference. Proinfla-mmatory cytokines are essential to lead to bone loss and critical concentration of these cytokines such as IL-1,-6,-11,-17, TNFα spreads inflammation in the region adjacent bone.38 A mechanism of AGEs in hyperglycemic condition of diabetics is change in level of cytokines, free radicals, hormones.21 So, impaired osseointegration of implants and high risk of peri-implantitis in patients with diabetes mellitus were reported.39,40 But, invasive dental therapy including implant treatment is not contraindication in well-controlled diabetic patients and several articles reported that the clinical outcome of implants in such diabetics is favorable.41-43 In the present study, all patients were restored with implant-supported fixed prostheses and did not develop specific complications. Although only one patient of control group lost all maxillary teeth, multiple implant-supported fixed therapy was performed instead of removable denture. Generally, a consideration of proper angulation, position and bone quality is appreciated for implant-supported fixed restorations. Michaeli et al. stated bone type and quality, surgical protocol, duration of osseointegration, restoration type as rehabilitative factors in diabetics.44 They mentioned that a removable restoration may be preferred in diabetic patients in cases of difficulty of exact implant localization in the jaw bone. As diabetic patients are recognizing implant treatment as an accepted treatment choice, it is essential to identify whether implants or fixed or removable type can be used in diabetic patients, educate patient to understand their oral and systemic state before treatment and help maintain favorable state after treatment.
The tooth mortality implying periodontal disease and implant treatment rate were significantly higher in the DM group and in both univariate and multivariate logistic regression analyses, old age groups showed significantly higher odds ratios and higher tooth loss rate. As implant supported restoration is an alternative therapy, it is necessary to make periodontal patients with DM aware their oral and systemic state before implant treatment and to help them maintain favorable state after treatment.
Figures and Tables
References
1. Field EA, Longman LP, Bucknall R, Kaye SB, Higham SM, Edgar WM. The establishment of a xerostomia clinic: a prospective study. Br J Oral Maxillofac Surg. 1997. 35:96–103.
2. Kadir T, Pisiriciler R, Akyüz S, Yarat A, Emekli N, Ipbüker A. Mycological and cytological examination of oral candidal carriage in diabetic patients and non-diabetic control subjects: thorough analysis of local aetiologic and systemic factors. J Oral Rehabil. 2002. 29:452–457.
3. Petrou-Amerikanou C, Markopoulos AK, Belazi M, Karamitsos D, Papanayotou P. Prevalence of oral lichen planus in diabetes mellitus according to the type of diabetes. Oral Dis. 1998. 4:37–40.
4. Lorini R, Scaramuzza A, Vitali L, d'Annunzio G, Avanzini MA, De Giacomo C, Severi F. Clinical aspects of coeliac disease in children with insulin-dependent diabetes mellitus. J Pediatr Endocrinol Metab. 1996. 9:101–111.
5. Guggenheimer J, Moore PA, Rossie K, Myers D, Mongelluzzo MB, Block HM, Weyant R, Orchard T. Insulin-dependent diabetes mellitus and oral soft tissue pathologies: II. Prevalence and characteristics of Candida and Candidal lesions. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2000. 89:570–576.
6. Hill LV, Tan MH, Pereira LH, Embil JA. Association of oral candidiasis with diabetic control. J Clin Pathol. 1989. 42:502–505.
7. Horning GM, Hatch CL, Cohen ME. Risk indicators for periodontitis in a military treatment population. J Periodontol. 1992. 63:297–302.
8. Emrich LJ, Shlossman M, Genco RJ. Periodontal disease in non-insulin-dependent diabetes mellitus. J Periodontol. 1991. 62:123–131.
9. Campus G, Salem A, Uzzau S, Baldoni E, Tonolo G. Diabetes and periodontal disease: a case-control study. J Periodontol. 2005. 76:418–425.
10. Faggion CM Jr, Petersilka G, Lange DE, Gerss J, Flemmig TF. Prognostic model for tooth survival in patients treated for periodontitis. J Clin Periodontol. 2007. 34:226–231.
11. Bacić M, Plancak D, Granić M. CPITN assessment of periodontal disease in diabetic patients. J Periodontol. 1988. 59:816–822.
12. Tervonen T, Oliver RC. Long-term control of diabetes mellitus and periodontitis. J Clin Periodontol. 1993. 20:431–435.
13. Ebersole JL, Holt SC, Hansard R, Novak MJ. Microbiologic and immunologic characteristics of periodontal disease in Hispanic americans with type 2 diabetes. J Periodontol. 2008. 79:637–646.
14. Kim JB, Jung MH, Cho JY, Park JW, Suh JY, Lee JM. The influence of type 2 diabetes mellitus on the expression of inflammatory mediators and tissue inhibitor of metalloproteinases-2 in human chronic periodontitis. J Periodontal Implant Sci. 2011. 41:109–116.
15. Ryan ME, Carnu O, Kamer A. The influence of diabetes on the periodontal tissues. J Am Dent Assoc. 2003. 134:34S–40S.
16. Nishimura F, Iwamoto Y, Soga Y. The periodontal host response with diabetes. Periodontol 2000. 2007. 43:245–253.
17. McMullen JA, Van Dyke TE, Horoszewicz HU, Genco RJ. Neutrophil chemotaxis in individuals with advanced periodontal disease and a genetic predisposition to diabetes mellitus. J Periodontol. 1981. 52:167–173.
18. Tan JS, Anderson JL, Watanakunakorn C, Phair JP. Neutrophil dysfunction in diabetes mellitus. J Lab Clin Med. 1975. 85:26–33.
19. Um YJ, Jung UW, Kim CS, Bak EJ, Cha JH, Yoo YJ, Choi SH. The influence of diabetes mellitus on periodontal tissues: a pilot study. J Periodontal Implant Sci. 2010. 40:49–55.
20. Davies JE. Understanding peri-implant endosseous healing. J Dent Educ. 2003. 67:932–949.
21. Southerland JH, Taylor GW, Moss K, Beck JD, Offenbacher S. Commonality in chronic inflammatory diseases: periodontitis, diabetes, and coronary artery disease. Periodontol 2000. 2006. 40:130–143.
22. Scherp HW. Current concepts in periodontal disease research: epidemiological contributions. J Am Dent Assoc. 1964. 68:667–675.
23. Löe H. Periodontal disease. The sixth complication of diabetes mellitus. Diabetes Care. 1993. 16:329–334.
24. Genco RJ. Current view of risk factors for periodontal diseases. J Periodontol. 1996. 67:1041–1049.
25. Eickholz P, Kaltschmitt J, Berbig J, Reitmeir P, Pretzl B. Tooth loss after active periodontal therapy. 1: patient-related factors for risk, prognosis, and quality of outcome. J Clin Periodontol. 2008. 35:165–174.
26. Aitken S, Birek P, Kulkarni GV, Lee WL, McCulloch CA. Serial doxycycline and metronidazole in prevention of recurrent periodontitis in high-risk patients. J Periodontol. 1992. 63:87–92.
27. Thorstensson H, Hugoson A. Periodontal disease experience in adult long-duration insulin-dependent diabetics. J Clin Periodontol. 1993. 20:352–358.
28. Soskolne WA. Epidemiological and clinical aspects of periodontal diseases in diabetics. Ann Periodontol. 1998. 3:3–12.
29. Taylor GW. Bidirectional interrelationships between diabetes and periodontal diseases: an epidemiologic perspective. Ann Periodontol. 2001. 6:99–112.
30. Taylor GW, Borgnakke WS. Periodontal disease: associations with diabetes, glycemic control and complications. Oral Dis. 2008. 14:191–203.
31. Mealey BL, Ocampo GL. Diabetes mellitus and periodontal disease. Periodontol 2000. 2007. 44:127–153.
32. Grossi SG, Skrepcinski FB, DeCaro T, Robertson DC, Ho AW, Dunford RG, Genco RJ. Treatment of periodontal disease in diabetics reduces glycated hemoglobin. J Periodontol. 1997. 68:713–719.
33. Rodrigues DC, Taba MJ, Novaes AB, Souza SL, Grisi MF. Effect of non-surgical periodontal therapy on glycemic control in patients with type 2 diabetes mellitus. J Periodontol. 2003. 74:1361–1367.
34. Kiran M, Arpak N, Unsal E, Erdoğan MF. The effect of improved periodontal health on metabolic control in type 2 diabetes mellitus. J Clin Periodontol. 2005. 32:266–272.
35. Taylor GW, Burt BA, Becker MP, Genco RJ, Shlossman M, Knowler WC, Pettitt DJ. Severe periodontitis and risk for poor glycemic control in patients with non-insulin-dependent diabetes mellitus. J Periodontol. 1996. 67:1085–1093.
36. Grossi SG, Skrepcinski FB, DeCaro T, Zambon JJ, Cummins D, Genco RJ. Response to periodontal therapy in diabetics and smokers. J Periodontol. 1996. 67:1094–1102.
37. Grossi SG, Skrepcinski FB, DeCaro T, Robertson DC, Ho AW, Dunford RG, Genco RJ. Treatment of periodontal disease in diabetics reduces glycated hemoglobin. J Periodontol. 1997. 68:713–719.
38. Cochran DL. Inflammation and bone loss in periodontal disease. J Periodontol. 2008. 79:1569–1576.
39. Hasegawa H, Ozawa S, Hashimoto K, Takeichi T, Ogawa T. Type 2 diabetes impairs implant osseointegration capacity in rats. Int J Oral Maxillofac Implants. 2008. 23:237–246.
40. Ferreira SD, Silva GL, Cortelli JR, Costa JE, Costa FO. Prevalence and risk variables for peri-implant disease in Brazilian subjects. J Clin Periodontol. 2006. 33:929–935.
41. Olson JW, Shernoff AF, Tarlow JL, Colwell JA, Scheetz JP, Bingham SF. Dental endosseous implant assessments in a type 2 diabetic population: a prospective study. Int J Oral Maxillofac Implants. 2000. 15:811–818.
42. Peled M, Ardekian L, Tagger-Green N, Gutmacher Z, Machtei EE. Dental implants in patients with type 2 diabetes mellitus: a clinical study. Implant Dent. 2003. 12:116–122.
43. Tawil G, Younan R, Azar P, Sleilati G. Conventional and advanced implant treatment in the type II diabetic patient: surgical protocol and long-term clinical results. Int J Oral Maxillofac Implants. 2008. 23:744–752.
44. Michaeli E, Weinberg I, Nahlieli O. Dental implants in the diabetic patient: systemic and rehabilitative considerations. Quintessence Int. 2009. 40:639–645.




 PDF
PDF ePub
ePub Citation
Citation Print
Print





 XML Download
XML Download