Abstract
PURPOSE
Over the past years, the adhesion of fiber posts luted with simplified adhesive systems has been a matter of great interest. The aim of this study was to assess the post retentive potential of a self-adhesive resin cement using different adhesive systems to compare the push-out bond strengths of fiber posts.
MATERIALS AND METHODS
The post spaces of 56 mandibular premolar roots were prepared and divided into 4 experimental groups and further divided into 2 subgroups according to testing time (n=7). The fiber posts (Rely X Fiber Post) were luted with a self-adhesive resin cement (RelyX Unicem) and one of the following adhesive systems: no adhesive, a total-etch adhesive resin (Single Bond), a two-step self-etch adhesive resin (Clearfil SE Bond) and a one-step self-etch adhesive resin (Clearfil S3 Bond). Each root was cut horizontally, and 1.5 mm thick six root segments were prepared. Push-out tests were performed after one week or three months (0.5 mm/min). Statistical analysis were performed with three-way ANOVA (α=.05).
RESULTS
Cervical root segments showed higher bond strength values than middle segments. Adhesive application increased the bond strength. For one week group, the total-etch adhesive resin Single Bond showed higher bond strength than the self-adhesive resin cement RelyX Unicem applied without adhesive resin at middle region. For 3 months group, the two-step self-etch adhesive resin Clearfil SE Bond showed the highest bond strength for both regions. Regarding the time considered, Clearfil SE Bond 3 months group showed higher bond strength values than one week group.
Fiber posts, in combination with resin cements, have been widely used to restore endodontically treated teeth. Currently, all resin cements are based upon the use of an etch-and-rinse or self-etch adhesive along with a low viscosity resin composite. This multi-step application technique is complex and rather technique sensitive, and consequently may compromise bonding effectiveness.1 Self-adhesive resin cements have been marketed to simplify clinical procedures and overcome the technique sensitivity of multi-step systems. These luting agents do not require any pretreatment of the tooth surface and their application is accomplished through a single clinical step.2 The adhesive properties are claimed to be based upon acidic monomers that demineralize and infiltrate the tooth substrate, resulting in micromechanical retention. Secondary reactions have been suggested to provide chemical adhesion to hydroxyapatite.3 Although several studies have indicated that the bond-strength values of self-adhesive resin cements are comparable to, or even higher than, those of conventional luting strategies4,5 their limited etching capability in the presence of the compact smear layer created within the endodontic space is a matter of concern.6,7 The peculiar histological characteristics of the intraradicular dentin, and the presence of a thick endodontic smear layer, has prompted some researchers to recommend a preliminary etching step of the dowel space before bonding.8 Elevation or modification of smear layer before using self-adhesive resin cement to improve the bond strength remains questionable.
Bond strength evaluations are conventionally performed at 24 hours or longer after restorative procedures.6,9-11 As reported by several researchers, a significant decrease in bond strength after long-term usage may reduce the success rate of restorations, thereby leading to failure.
Over the past years, the adhesion of fiber posts luted with simplified adhesive systems has been a matter of great interest. Thus, the aim of this study was to compare one week and 3 months interfacial strength of fiber posts luted with no adhesive or different adhesive systems and a self-adhesive resin cement. The null hypotheses tested were: (a) there are no difference between cervical and middle third regions, (b) adhesive application prior to use self-adhesive resin cement do not improve the bond strength of fiber posts, (c) there are no difference between the different adhesive systems, (d) there are no differences in the interfacial strengths of root sections tested between one week and 3 months of storage.
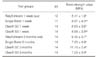
To evaluate different types of adhesive system and testing time that influenced bond strength, 3 different adhesive systems, a total-etch adhesive resin (Adper Single Bond 2), a two-step self-etch adhesive resin (Clearfil SE Bond) and a one-step self-etch adhesive resin (Clearfil S3 Bond) and a self-etch adhesive resin (RelyX Unicem) and 2 indicate as storage time (1 week or 3 months) were studied. Materials investigated in this study were shown in Table 1.
Fifty-six freshly extracted human mandibular premolar teeth with straight root canals, free of cracks, caries and fully developed apices were selected for this study. External debris was removed with a scaler and then stored in distilled water for no more than a month. Crown surfaces of each tooth were sectioned below cemento-enamel junction perpendicular to their long axis with a diamond bur (SS White Burs, NJ, USA) under water cooling, to achieve a uniform length of 16 mm. Cleaning and shaping was performed using a crown-down preparation technique employing nickel-titanium rotary instruments (Size S1, S2 and F3, Protaper; Dentsply Maillefer, Ballaigues, Switzerland) to size 30, 0.09 taper. During instrumentation, canals were irrigated with 1 mL of 2.5% NaOCl. Following the final irrigation, the canal spaces were completely dried with absorbent paper points (DenstplyDeTrey, Konstanz, Germany). The obturation was performed using AH26 (Dentsply DeTrey) and gutta-percha with cold lateral compaction. Cervical root canal openings were then filled with a provisional restorative material (Cavit-G, 3M ESPE) and the roots were stored in a humidor for 1 week at 37℃.
Coronal gutta-percha was removed using the heat transferring instrument of the System B (EIE-Analytic Technology, Orange, CA, USA) and then Gates Glidden drills (No. 2 and 3; Dentsply Maillefer) leaving 4 mm of material apically. Then the root canals of each sample were enlarged using the post system drill [RelyX Fiber Post drill (size 1)] provided by the manufacturer of the selected post. All specimens were prepared by one practitioner using a standardized procedure; the depth of the post space preparation was 12 mm. Following the post space preparations, the canals were rinsed with distilled water for 2 minutes and dried with paper points. A tapered glass fiber post (RelyX Fiber Post size 1) was inserted with a resin cement and four different adhesive resins.
Group 1: No adhesive was used.
Group 2: A total-etch adhesive resin (Adper Single Bond 2) was applied to the prepared post spaces. The root canals were etched for 15 seconds using 35% phosphoric acid gel, rinsed for 20 seconds and gently air-dried. Excess water was removed using paper points. Two coats of adhesive resin was applied to the post spaces using paper points. The root canals were gently dried, excess bond was removed using paper points and light-cured for 20 seconds, with the tip of the light unit (Hilux 550, Ankara, Turkey) directly in contact with the post space opening.
Group 3: A two-step self-etch adhesive resin (Clearfil SE Bond) was applied. The self-etching primer (Clearfil SE Bond Primer) was applied to the post spaces allowed to etch for 30 seconds and gently dried. Then adhesive (Clearfil SE Bond) was applied and excess bond was removed using paper points and light-cured for 20 seconds.
Group 4: A one-step self-etch adhesive resin (Clearfil S3 Bond) was applied to the post spaces using paper points and gently dried. Excess bond was removed and light-cured for 20 seconds.
The surfaces of the posts were cleaned with alcohol as recommended by the manufacturers. In all groups, self-adhesive resin cement (RelyX Unicem) was used for luting the posts. The cement was prepared by mixing the caps for 15 seconds and introduced in the canal by use of elongation tips and the post was then coated with cement, inserted in the canal to full depth by using finger pressure and light-cured for 40 seconds. After the cementation procedures, access cavities were completely covered with glass ionomer cement (Fuji IX, GC Corp., Tokyo, Japan). To evaluate the short and long term period of the push-out bond strength, each group was then equally divided into two subgroups. The first subgroup was stored for 1 week and second subgroup was stored for 3 months in distilled water at 37℃ before testing.
Push-out test was shown in Fig. 1. Each root was cut horizontally with a slow-speed diamond saw (Mecatome, T2001A, Pressi, France) to produce six 1.5 (± 0.05) mm-thick segments (2 apical, 2 middle, 2 cervical). The apical surfaces of the slices were marked with a indelible marker. The push-out test was performed on these slabs using an universal testing machine (Autograph AG-10kNIS, Shimadzu Co., Kyoto, Japan) connected to load cell, operating at a cross-head speed of 0.5 mm/min-1. The apical surface was placed facing the punch tip, ensuring that loading forces were introduced from an apical to coronal direction. Care was taken to center the push-out pin (diameter of 1.0 mm at cervical, 0.5 mm at middle, 0.25 mm at apical) on the center of the post surface, without stressing the surrounding post space walls. The peak of extrusion of the post segment from the slice was taken as point of bond failure and the value was recorded in Newton (N). Push-out strength data were converted to Mega Pascal (MPa) by dividing the load in Newton by the surface area (SL) in mm2. SL calculated as the lateral surface area of a truncated cone using the formula: SL = π(R + r) [(h2 + (R - r)2]0.5 where R is the coronal post-radius, r the apical post-radius and h the thickness of the slice. The wider and narrowest diameters of the post and the thickness of the slice were individually measured using a digital caliper with 0.01 accuracy.
Statistical analysis were performed with three-way analysis of variance (ANOVA) followed by a one-way ANOVA and Tukey's HSD comparisons (α=.05). The analysis of the apical root segments were not evaluated. Subsequently, each specimen was observed using a stereomicroscope (Olympus S 240, Tokyo, Japan) at ×40 magnification to determine the failure modes.
Failure was considered; adhesive in dentin - if cement was totally seperated from dentin; adhesive in post-if cement was totally seperated from post; mixed - when occured a mixture of adhesive in dentin and post failure; and cohesive - if the fracture occured only in post or dentin.12 The failure photographs of each group was given in Fig. 2. Bond failure sites were not statistically analyzed.
Results of the three-way ANOVA were given in Table 2 and mean push-out bond strength values of the tested groups were given in Table 3. For all test groups, cervical root segments showed higher bond strengths than middle root segments. There was a significant difference between the groups for both cervical and middle regions (Table 4 and Table 5). Adhesive application increased the bond strength. For 1 week group, there was not a significant difference between the groups at cervical region. However, there was a significant difference between the groups at middle region. Adper Single Bond 2 showed higher bond strength than RelyX Unicem without adhesive. The difference was not important between the adhesive applied groups. For 3 months groups, there was a significant diffrence between the groups. The highest bond strength values were obtained from Clearfil SE Bond at cervical region. There was not a significant difference between the other groups. The bond strength values of Clearfil SE Bond was higher than Rely X Unicem without adhesive and Clearfil S3 Bond at middle region. There was not a significant difference between Adper Single Bond 2 and the other groups. When considering time, only Clearfil SE Bond showed significant difference. Clearfil SE Bond 3 months showed higher bond strength values than Clearfil SE Bond one week group.
The bond strength between pretreated root canal dentin and fiber-reinforced posts were evaluated using a push-out test. The push-out test provides a better estimation of the bonding strength than the conventional shear test because with the push-out test the fracture occurs in parallel to the dentin-bonding interface. Additionally, the push-out test has been considered more dependable than the microtensile test for bonded posts.13
In this study, it was not possible to evaluate the bond strengths of the apical root segments because of the deformation of thin push-out pin, then analysis of apical segments of the specimens were omitted. The first hypothesis was rejected, because significant differences in bond strength values were observed among the different root canal segments. The push-out bond strength for the cervical segments was higher compared to the middle segments, in agreement with Ohlmann et al.14 and Mallmann et al.15 The bond strengths in different post space dentin regions seemed to be influenced by tubule density and the area of dentin.16 Tubule density and diameter of the tubules decrease in the apical direction, which may influence the micromechanical bonding mechanism of the adhesive systems.17 Moreover, it has been reported that the root canal dentin walls after post space preparation are covered with remnants of gutta-percha and sealer, rough debris, and a thick smear layer which is higher in the apical direction that could not be perfectly removed.18
In the current study, lowest bond strength values were obtained from self-adhesive resin cement without adhesive application, which opposes the second hypothesis. Adhesive application prior to the use of self-adhesive resin cement RelyX Unicem improved the bond strength of fiber posts. De Munck et al.19 stated that although the pH of the mixed RelyX Unicem was very low (<2 during the first minute, data supplied by 3M ESPE), nearly no demineralization of the dentin surface was noticed. The metacrylated phosphoric esters in the adhesive cannot penetrate adequately through the retained partly dissolved smear layer on the root canal walls, resulting in interfacial gaps and lower bond strengths in vitro.20,21 In addition to this, relatively high viscosity of the material and the limited penetration/interaction time (the material was light cured directly after application) might influence bonding. Etching and/or priming the dentin before using self-adhesive cement might enhance micromechanical bonding by demineralizing dentin, by removing or modifying smear layer.
In the present study, different adhesive systems influenced the push-out bond strength of fiber posts, which opposes the third hypothesis. Push-out bond strength results are similar at cervical region in one week group. At middle region Single Bond showed higher bond strength than RelyX Unicem without adhesive. It is well known that a wet-bonding technique is essential for a total-etching system to achieve optimal bond strength.22 Although control of surface wetness is difficult to achieve in the deep and narrow post spaces within a root canal, the middle region does not seem to be influenced. The bond strengths of Clearfil S3 Bond and Clearfil SE Bond were not different from Adper Single Bond 2 and RelyX Unicem without adhesive. Additionally, Clearfil SE Bond showed higher bond strength results at both cervical region and middle region in 3 months group. It has been reported that bond strengths to root canal dentin of self-etching systems are not affected by the depth of the post-space region.16,23,24
When considering time, mean bond strengths of Clearfil SE bond increased by time. De Munck et al.25 found that two-step self-etch adhesives exhibited not only among the highest bond strengths at baseline but also after one year water storage, the highest bond strengths were recorded in this group. It was stated that the adhesive contained the functional monomer 10-MDP, which affectively interacts chemically with HAP with a reasonable time, and the calcium salt of which hardly soluble showed no signs of degradation in bond strength and interfacial ultrastructure.26 Presence of 10 MDP functional monomers and filler particles in Clearfil SE Bond and formation of a relatively thick layer that serves as an elastic buffer zone during polymerization of resin composite ensure bond durability.27 Miguez et al.28 stated that the post-curing of the adhesive resin and more specifically of the oxygen inhibited layer may have occurred owing to the 37℃ heat storage condition during the long period of time. The enhanced polymerization of a thicker oxygen-inhibited layer might be responsible for the significant increase in bond strengths for Clearfil SE Bond. Fourth hypothesis was then rejected.
The retention of fiber posts in roots is dependent upon the adhesion between the resin cement and the dentin, as well as on the adhesion between the resin cement and posts. However, the adhesion between resin and dentin is considered to be a weak point in luting a fiber post.29,30 The fracture types observed in the analyzed samples were adhesive in dentin, adhesive in post, mixed and cohesive. Generally mixed failures were observed from each group. Only in Clearfil SE Bond 3 months group, percentage of adhesive post failure was similar to mixed type. This finding supported the highest bond strength results of Clearfil SE Bond.
Within the limitations of this study, dentin bond strength of the total-etch adhesive resin Single Bond, the one-step self-etch adhesive resin Clearfil S3 Bond, the self-adhesive resin cement RelyX Unicem remained stable and the bond strengths of the two-step self-etch adhesive resin Clearfil SE Bond increased with time.
Figures and Tables
 | Fig. 2The failure photographs of each group. (A) Adhesive in dentin, (B) Adhesive in post, (C) Mixed, (D) Cohesive. |
 | Fig. 3Predominating type of fracture occurred in each group (%).
*U: RelyXUnicem without adhesive, SB: Single Bond, CSE: Clearfil SE Bond, CS3: Clearfil S3 Bond, (c): cervical root segment, (m): middle root segment.
|
References
1. Mak YF, Lai SC, Cheung GS, Chan AW, Tay FR, Pashley DH. Micro-tensile bond testing of resin cements to dentin and an indirect resin composite. Dent Mater. 2002; 18:609–621.
2. Mazzitelli C, Monticelli F, Osorio R, Casucci A, Toledano M, Ferrari M. Effect of simulated pulpal pressure on self-adhesive cements bonding to dentin. Dent Mater. 2008; 24:1156–1163.
3. Bitter K, Paris S, Pfuertner C, Neumann K, Kielbassa AM. Morphological and bond strength evaluation of different resin cements to root dentin. Eur J Oral Sci. 2009; 117:326–333.
4. Radovic I, Monticelli F, Goracci C, Vulicevic ZR, Ferrari M. Self-adhesive resin cements: a literature review. J Adhes Dent. 2008; 10:251–258.
5. Bitter K, Kielbassa AM. Post-endodontic restorations with adhesively luted fiber-reinforced composite post systems: a review. Am J Dent. 2007; 20:353–360.
6. Sirimai S, Riis DN, Morgano SM. An in vitro study of the fracture resistance and the incidence ofvertical root fracture of pulpless teeth restored with six post-and-coresystems. J Prosthet Dent. 1999; 81:262–269.
7. Sadek FT, Goracci C, Monticelli F, Grandini S, Cury AH, Tay F, Ferrari M. Immediate and 24-hour evaluation of the interfacial strengths of fiber posts. J Endod. 2006; 32:1174–1177.
8. Zhang L, Huang L, Xiong Y, Fang M, Chen JH, Ferrari M. Effect of post-space treatment on retention of fiber posts in different root regions using two self-etching systems. Eur J Oral Sci. 2008; 116:280–286.
9. Bouillaguet S, Troesch S, Wataha JC, Krejci I, Meyer JM, Pashley DH. Microtensile bond strength between adhesive cements and root canal dentin. Dent Mater. 2003; 19:199–205.
10. Goracci C, Fabianelli A, Sadek FT, Papacchini F, Tay FR, Ferrari M. The contribution of friction to the dislocation resistance of bonded fiber posts. J Endod. 2005; 31:608–612.
11. Sahafi A, Peutzfeld A, Asmussen E, Gotfredsen K. Effect of surface treatment of prefabricated posts on bonding of resin cement. Oper Dent. 2004; 29:60–68.
12. Teixeira CS, Pasternak-Junior B, Borges AH, Paulino SM, Sousa-Neto MD. Influence of endodontic sealers on the bond strength of carbon fiber posts. J Biomed Mater Res B Appl Biomater. 2008; 84:430–435.
13. Perdigão J, Gomes G, Lee IK. The effect of silane on the bond strengths of fiber posts. Dent Mater. 2006; 22:752–758.
14. Ohlmann B, Fickenscher F, Dreyhaupt J, Rammelsberg P, Gabbert O, Schmitter M. The effect of two luting agents, pretreatment of the post, and pretreatment of the canal dentin on the retention of fiber-reinforced composite posts. J Dent. 2008; 36:87–92.
15. Mallmann A, Jacques LB, Valandro LF, Mathias P, Muench A. Microtensile bond strength of light- and self-cured adhesive systems to intraradicular dentin using a translucent fiber post. Oper Dent. 2005; 30:500–506.
16. Akgungor G, Akkayan B. Influence of dentin bonding agents and polymerization modes on the bond strength between translucent fiber posts and three dentin regions within a post space. J Prosthet Dent. 2006; 95:368–378.
17. Ferrari M, Mannocci F, Vichi A, Cagidiaco MC, Mjör IA. Bonding to root canal: structural characteristics of the substrate. Am J Dent. 2000; 13:255–260.
18. Serafino C, Gallina G, Cumbo E, Ferrari M. Surface debris of canal walls after post space preparation in endodontically treated teeth: a scanning electron microscopic study. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2004; 97:381–387.
19. de Munck J, Vargas M, van Landuyt K, Hikita K, Lambrechts P, van Meerbeek B. Bonding of an auto-adhesive luting material to enamel and dentin. Dent Mater. 2004; 20:963–971.
20. Goracci C, Tavares AU, Fabianelli A, Monticelli F, Raffaelli O, Cardoso PC, Tay F, Ferrari M. The adhesion between fiber posts and root canal walls: comparison between microtensile and push-out bond strength measurements. Eur J Oral Sci. 2004; 112:353–361.
21. Goracci C, Sadek FT, Fabianelli A, Tay FR, Ferrari M. Evaluation of the adhesion of fiber posts to intraradicular dentin. Oper Dent. 2005; 30:627–635.
22. Tay FR, Gwinnett AJ, Wei SH. The overwet phenomenon: a transmission electron microscopic study of surface moisture in the acid-conditioned, resin-dentin interface. Am J Dent. 1996; 9:161–166.
23. Foxton RM, Nakajima M, Tagami J, Miura H. Bonding of photo and dual-cure adhesives to root canal dentin. Oper Dent. 2003; 28:543–551.
24. Giannini M, Carvalho RM, Martins LR, Dias CT, Pashley DH. The influence of tubule density and area of solid dentin on bond strength of two adhesive systems to dentin. J Adhes Dent. 2001; 3:315–324.
25. de Munck J, Mine A, Vivan Cardoso M, de Almeida Neves A, van Landuyt KL, Poitevin A, van Meerbeek B. Effect of dentin location and long-term water storage on bonding effectiveness of dentin adhesives. Dent Mater J. 2011; 30:7–13.
26. Shirai K, de Munck J, Yoshida Y, Inoue S, Lambrechts P, Suzuki K, Shintani H, van Meerbeek B. Effect of cavity configuration and aging on the bonding effectiveness of six adhesives to dentin. Dent Mater. 2005; 21:110–124.
27. Inoue S, Koshiro K, Yoshida Y, De Munck J, Nagakane K, Suzuki K, Sano H, Van Meerbeek B. Hydrolytic stability of self-etch adhesives bonded to dentin. J Dent Res. 2005; 84:1160–1164.
28. Miguez PA, Pereira MP, Swift EJ Jr. One-year tensile bond strengths of two self-etching primers to bovine enamel. J Esthet Restor Dent. 2004; 16:243–248.
29. Boschian Pest L, Cavalli G, Bertani P, Gagliani M. Adhesive post-endodontic restorations with fiber posts: push-out tests and SEM observations. Dent Mater. 2002; 18:596–602.
30. Sahafi A, Peutzfeldt A, Asmussen E, Gotfredsen K. Retention and failure morphology of prefabricated posts. Int J Prosthodont. 2004; 17:307–312.




 PDF
PDF ePub
ePub Citation
Citation Print
Print








 XML Download
XML Download