Abstract
PURPOSE
This study investigated the effect of laser parameters and air-abrasion on the peel strength of silicon-based soft denture liner to different denture resins.
MATERIALS AND METHODS
Specimens (N=180) were prepared out of three different denture base resins (Rodex, cross-linked denture base acrylic resin; Paladent, heat-cured acrylic resin; Deflex, Polyamide resin) (75 mm × 25 mm × 3 mm). A silicon-based soft denture liner (Molloplast B) was applied to the denture resins after the following conditioning methods: a) Air-abrasion (50 µm), b) Er,Cr:YSGG laser (Waterlase MD Turbo, Biolase Technology) at 2 W-20 Hz, c) Er,Cr:YSGG laser at 2 W-30 Hz, d) Er,Cr:YSGG laser at 3 W-20 Hz, e) Er,Cr:YSGG laser at 3 W-30 Hz. Non-conditioned group acted as the control group. Peel test was performed in a universal testing machine. Failure modes were evaluated visually. Data were analyzed using two-way ANOVA and Tukey's test (α=.05).
RESULTS
Denture liner tested showed increased peel strength after laser treatment with different parameters (3.9±0.4 - 5.58±0.6 MPa) compared to the control (3.64±0.5 - 4.58±0.5 MPa) and air-abraded groups (3.1±0.6 - 4.46±0.3 MPa), but the results were not statistically significant except for Paladent, with the pretreatment of Er,Cr:YSGG laser at 3 W-20 Hz. Polyamide resin after air-abrasion showed significantly lower peel strength than those of other groups (3.1±0.6 MPa).
In dentistry, dentists take the advantage of using soft denture liners due to the viscoelastic properties.1-3 These liners act as shock absorbers in order to minimize and distribute the pressure on denture-bearing tissues, as well as to improve the intaglio denture surface.2,4-11 The use of soft lining material may be beneficial in promoting the success of complete dentures by enabling the dentures to withstand masticatory stress where the denture bearing tissues are comparatively intolerated.10,12-14 However, the use of soft denture liners is said to have several problems, among the most serious of which is adhesion failure between the soft denture and the denture base.2,9,11,12,15 It is also a potential surface for bacterial growth, plaque and calculus formation is mainly caused by bond failure. Therefore, frequent clinical evaluations and periodic replacement of soft denture liners are required.16 Thus, more laboratory time and extra costs are needed so as to construct dentures with permanent soft lining related to the equipment and materials used. Hence, an adequate bond between the denture base and the soft lining material is necessary.4,6,7,17,18 Previous studies17,19,20 have showed that Molloplast-B soft lining material (Detax, Karl Huber GmbH and Co., KG, Ettlingen, Germany) is one of the preferred materials for long-term clinical use because of its low water absorption and solubility.
Having particularly different molecular structures, polymethyl methacrylate (PMMA) denture base resin and silicone-based lining materials cannot be chemically bonded.9,21 Bonding the denture base resin and silicone-based lining material depends completely on an interfacial adhesive.9,21 Adhesion to polymeric materials usually requires some surface pretreatments to help improve the wettability characteristics of these materials.4,22 Several studies have investigated different methods to improve bond strength between liners and acrylic base resins. While some studies have investigated the effect of roughening by airborne-particle abrasion on the bond strength of soft liners to acrylic base resins,4,11,18,23-26 other studies were interested in the use of chemicals, including acrylic resin monomers,9,23,27 and their combinations,28-31 on the bond strength of soft liners with denture resins. However, controversial results have been reported. Despite the studies reporting that an improvement of interface strength was achieved by making the surface denture base roughness prior to the application of the lining material,4,25,32 others1,11,26 have not shown any negative effects on the roughening process of the bonding two materials.
Progress in laser technology has shown a quick adoption for being used by many in the field of dentistry due to the development of the first working laser by Maiman in 1960.11,24,33 Recently, lasers have been found to be effective in altering the surface of materials.4,11,24 However, few studies1,4,11,18,24 have used different types of lasers for the surface pretreatment of denture base resins before applying soft liner materials to improve the bond strength of these materials. The use of an Er,Cr:YSGG laser (Waterlase MD Turbo, Biolase Technology) to strengthen the bond between denture base resin and soft liner is taken into consideration by earlier studies published in limited editions, while using the Er,Cr:YSGG laser in a suitable condition, as well as setting, regarding air and water, the temperature rise of the target hard tissue has been reduced.33-35 The Er,Cr: YSGG laser has a high affinity for water.33-35 The singularity of this system lies in the presence of an air/water spray, which has a dual role: to support the cutting and to serve as a coolant to preserve the surface temperature low and to omit any potential detrimental thermal side-effects.33-35 As an alternative method to conventional ones, this gentle treatment on the tissue stands quite attractive.
Several types of tests have been used to assess the bond strength of soft lining materials to denture base resin.4,6,8,11,36 The three most commonly used are lap shear, tensile tests and peeling tests.36,37 The usefulness of these methods has been discussed. Peel testing is regarded as the best model of the clinical environment to test soft denture liners concerning the failure of soft lining materials.8,11,35,37
Currently, thermo-injectable, semi-rigid, high-impact polyamide resins are thought to be a valid alternative to the conventional acrylic resins due to their superior esthetic and functional characteristics and physicochemical qualities.38,39 Unfortunately, there is very limited knowledge about their clinical performance. The efficiency of the relining procedures for these materials has yet to be well studied.
The aim of the present study was to evaluate the effect of air-abrasion and laser treatment with different parameters on the bond strength of a silicone-based soft denture liner (Molloplast-B) to three different commonly used denture resins [a polyamide based high impact thermo-injection molded denture material (Deflex; Nuxen SRL, Ayacucho 1053 3-A, Cap. Fed. Buenos Aires, Argentina), a heat-cured cross-linked acrylic resin (Rodex; Rodont, Srl Milan, Italy Rodex) and a conventional heat-cured acrylic resin (Paladent; HeraeusKulzer GmbH, Wehrheim, Germany)] using the peel test. The null hypothesis was that the airabrasion and laser treatment with different pulse frequencies and power levels would not improve the peel bond strengths of silicone-based soft denture liner to different denture resins.
base acrylic resin (Rodex), a heat-cured acrylic resin (Paladent) and a polyamide resin (Deflex), as well as a heat-polymerized silicone-based resilient liner (Molloplast-B) were used in this study. The brand names, types and manufacturers of the materials used in this study are presented in Table 1.
So as to prepare the peel test materials, a mold of (75 mm × 25 mm × 3 mm) (ASTM D1876) was prepared from aluminum sheet and with the help of which specimens were produced from three plates of pink wax. For each test material, 66 wax specimens were produced (11 for each group) in which 198 wax specimens came out. The heat-cured samples were prepared in stone molds in denture flasks and were cured in a manner which is similar to that used in conventional denture construction.
After polymerization, the cured denture base resin plate was removed from the flask and trimmed, and the surface to be bonded was smoothed on 240 grit silicon carbide papers, cleaned and dried. The polyamide resin base was also prepared according to manufacturer's instructions. A total of 198 test specimens consisting of 66 Paladent, 66 Rodex and 66 Deflex specimens were prepared using these techniques. The specimens were placed in covered denture caps and stored in distilled water at 37℃ until the surface treatment simulated typical denture storage. Before surface treatments, the specimens were allowed to air dry for 24 hours. Six samples of each material were selected randomly to be investigated by scanning electron microscope (SEM; EVO L10, Carl Zeiss, Oberkochen, Germany) for differences in surface morphology after pretreatments. To create a space for the soft liner material, the acrylic specimens were reflasked using fresh pink wax material. After the removal of the wax, flasks with each acrylic specimen were randomly divided into six subgroups. There was not any pretreatment in the control group. Other test groups were either sandblasted with 50 µm Al2O3 particles or lased with different parameters.
The bonding surfaces of the test specimens received surface treatments as follows:
In Group 2, specimens were treated by alumina-abrasion with an abrasive blaster system and carbide-lined micro-pencil (Silfradent, S. Sofia-Forli, Italy). The nozzle (1.0 mm diameter) was held in light contact with each specimen and moved across the PMMA specimen for approximately 30 seconds with 50 µm aluminum oxide particles as the sandblasting medium at a pressure of 2 bar.
As a preliminary study, laser device was applied on the surface of the samples until we are satisfied with the roughness of the surface and the application time was calculated as 10 minutes. After that, we used this laser device in the same manner for all of the samples. The laser etching procedures (Group 3, 4, 5 and 6) were performed with an Er,Cr: YSGG laser system (Waterlase MD; Biolase Technology, San Clemente, CA) operating at a wavelength of 2,780 nm, a pulse duration of 140-200 µs, and repetition rates of 20 Hz (20 pulses per second) or 30 Hz (30 pulses per second). The power output was set at 2 W or 3 W according to the test protocols. Air and water sprays from the handpiece were adjusted to a level of 85% air and 85% water for 2 W (100 mJ/Pulse) and 3 W (150 mJ/Pulse) power outputs to prevent the acrylic surface from overheating. Laser energy was delivered through a fiber optic system to a sapphire tip terminal 600 µm in diameter and 6 mm long. The focused laser beam was aligned to the polymerized acrylic surface perpendicularly at 1 mm, and the area to be bonded with soft liner was treated manually in a sweeping fashion in accordance with the manufacturer's instructions for etching. Visual comparisons of the treated samples were examined by SEM at magnification ×100.
After surface treatment, the specimens were secured in gypsum molds (Moldbaster S; HeraeusKulzer GmbH, Hanau, Germany). Soft lining material should be bonded over 25 mm of acrylic specimen and separated over the remaining 50 mm.3,17 The surface of the specimen that was to remain unbonded (50 mm × 25 mm) was covered with a piece of tin foil. Primo adhesive of Molloplast-B was applied uniformly onto the adherent surfaces of the specimens (25 mm × 25 mm) and allowed to dry for 60 minutes. The soft material was then mixed and packed over the acrylic blanks. After polymerization the specimens were removed and trimmed with scissors and a sharp blade. Specimens were then stored in distilled water at 37℃ for one week.18
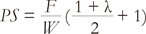
A universal testing machine (Instron Corp., Canton, MA, USA) was used to peel the soft lining materials at an angle of 180 degrees and a constant cross-head speed of 10 mm/min. The force needed to cause failure and the modes of failure were recorded. Peel bond strength (N/mm = MPa) was calculated as follows:17
where the F is the maximum force recorded (N), W is the width of the specimens (mm), and λ is the extension ratio of the liner (the ratio of the stretched to the unstretched length). The denture base material/soft lining material interface was visually analyzed and the failure modes were characterized as cohesive, adhesive, or mixed depending on whether the fracture surface was in the soft liner only, at the denture base-soft liner interface only, or in both, respectively.6,7
The results were recorded and analyzed using the statistical package (SPSS for Windows 15.0 SPSS Inc., Chicago, IL, USA). A two-way ANOVA and Fischer's LSD test were used for comparing the groups and acrylic materials at a confidence interval of 95%.
The mean and standard deviation of peel bond strength values of the test specimens are shown in Table 2. The peel bond strength values were significantly influenced by the test protocols and tested materials. Different test protocols influenced the peel bond strengths of different test materials.
Peel bond strength values ranged from 3.16 ± 0.64 MPa to 4.74 ± 0.74 MPa in the Paladent group. The highest values were observed in Group 5 (lased 3 W, 20 Hz), while the lowest values were recorded in Group 2 (sandblasted with Al2O3). According to the comparisons of groups, in the Paladent group, the values obtained were as follows: Group 5 > Group 3 > Group 4 > Group 6 > Group 1 > Group 2. Significantly lower values were observed in Group 2 compared to Group 5 (P<.05). A significant difference was found between Group 5 and Group 6.
In the Rodex group, the values obtained were as follows: Group 6 > Group 4 > Group 2 > Group 5 > Group 3 > Group 1 (P>.05). The highest peel bond strength (4.81 ± 1.32 MPa) was observed in group 6 (lased 3 W, 30 Hz), while the lowest peel bond strength (3.89 ± 0.48 MPa) was recorded in Group 1 (untreated). No significant differences were found among these subgroups in the Rodex group.
In the Deflex group, the values observed were as follows: Group 3 > Group 4 > Group 5 > Group 6 > Group 1 > Group 2. The highest peel bond strength (5.58 ± 0.66 MPa) was observed in Group 3 (lased 2 W, 20 Hz), while lowest peel bond strength (3.10 ± 0.55 MPa) was recorded in Group 2 (sandblasted with Al2O3). Significantly lower values were obtained in Group 2 compared to the other groups (P<.05).
According to the acrylic material comparisons, in Group 1, the Deflex specimens exhibited higher values compared to the Rodex and Paladent specimens. No significant differences were found between the Rodex and Paladent specimens. In Group 2, significantly higher values were observed in the Rodex specimens compared to the Paladent and Deflex specimens. No significant differences were found between the Paladent and Deflex specimens. In Group 3, the Deflex specimens exhibited higher values compared to the Paladent and Rodex specimens. No significant differences were found between the Paladent and Rodex specimens. In Group 4, the Deflex specimens showed higher values compared to the Rodex and Paladent specimens. No significant differences were found between the Rodex and Paladent specimens. In Group 5, the Deflex specimens exhibited higher values compared to the Paladent and Rodex specimens. No significant differences were found between the Paladent and Rodex specimens. In Group 6, the Rodex specimens exhibited higher values compared to the Deflex and Paladent specimens.
Surface evaluations of the samples were performed with SEM after pretreatment (Fig. 1, 2, 3, 4, 5, 6). Surface morphology was changed after the surface pretreatments. In sandblasting groups, residual of the Al2O3 particles were seen in the samples (Fig. 6). Er,Cr:YSGG laser treatment at 3 W-20 Hz irradiation has more effect on the PMMA, which results more homogeny irregularities on their surfaces than the other pretreatments (Fig. 3C, Fig. 4C and Fig. 5C). According to the SEM results for Deflex, it appears that laser resulted in the formation of numerous very smaller holes, distributed irregularly (Fig. 3).
Modes of failure in each group of the specimens are shown in Table 3. Group 5 demonstrated a tendency of cohesive failure for Deflex and Paladent, while Rodex showed mixed type of failure. Adhesive types of failure were observed typically in all of the sandblasting groups except the Rodex group. Group 4 and 6 for Deflex, the tendency was equally shared among cohesive and mixed failures.
Different techniques have been used to increase the bond strength between the acrylic resin denture and the soft lining material. However, there have not been enough published articles investigating the effect of laser surface treatments on peel bond strength of soft lining material to acrylic denture resin. The present study compared the effect of air-abrasion and Er,Cr:YSGG laser treatment with different parameters on the peel strength of silicone-based soft denture liner to three different resins. The null hypothesis that the air-abrasion and laser treatment with different pulse frequencies and power levels would not improve the peel bond strengths of silicone-based soft denture liner to different denture resins was partially rejected in terms of the pretreatment technique.
In order to examine the bond strength of soft liners to denture base materials, it is possible to find many various types of laboratory tests.4,6,8,11,36,40 There are earlier study results with conclusion that bond strength characteristics can diversify consistent with the test method applied.38,39 The peel, tensile and shear tests are considered the most frequently used ones to date.6,36,37 Scientifically, the peel test has multiple advantages. It's been reported that the peel test is a more significant one regarding foreseeing the ability of a material to bond in a clinical setting since debonding normally initiates at the exposed edge of the lining through an apparent peeling process.8 The peel test is a unique method in which failure proceeds at a controlled stage, and the peel force is a direct measure of the work of detachment.8,11,36 In addition, the nature of the stresses exerted on the edges of the union is considered to be more closely represented by a peel test.8,11,36 However, the results gained from peel tests were insufficient due to a higher probability of cohesive failure in the soft materials used, the results in question are influenced by the compliance together with the thickness of the materials.37,40,41 In this study, the peel bond strength test method has been used.
The results of the present study showed that Er, Cr:YSGG laser irradiation increased the bond strength of the acrylic denture base resin to the silicone relining material. Heat-cured acrylic resin with laser pretreatment at 3 W, 20 Hz showed significantly increased bond strengths to the Molloplast-B compared to the other pretreatment groups. Homogenous pore structure was detected by the SEM evaluation in Group 5 (Fig. 3C, Fig. 4C and Fig. 5C). The bond strength of the soft relining materials might be improved by flowing into these micro porosities.
Increased peel bond strength values for Group 5 (3 W, 20 Hz) implied better adhesion and supported the SEM results. Different pulse frequencies and power levels caused different peel bond strength values. However, sandblasting the denture base resin with Al2O3 significantly decreased the bond strength of the acrylic denture base resin to the silicone relining material. The different results of this study may be caused by the different chemical structures of the resins and their surface characteristics after the pretreatment procedures.
Jacobsen et al.11 examined the effect of lasing and sandblasting in a similar fashion to the current study, but it came out that changing the PMMA surface by sandblasting with 250 µm Al2O3 particles or lasing with a CO2 laser reduced the peel strength values in comparison with the untreated surface test samples.In their study, Usumez et al.4 compared the bond strength and adhesion of denture liner (Molloplast-B) to alumina-abraded or lased heat-cured polymethyl methacrylate denture base resin. It's been discovered that lasing and alumina-abrasion of the PMMA before resilient-material application concluded in higher mean tensile bond strengths than those of control samples, but this growth was not statistically of importance. Jacobsen et al.11 reported that surface treatment with a CO2 laser was ineffective in reducing adhesive failure of soft-lined prostheses in a clinical situation. In their study, Akın et al.24 investigated the effect of different surface treatments of PMMA acrylic denture base resin on the tensile bond strength of a silicone-based soft denture liner. It has been discovered that treating the polymethyl methacrylate surface by Er:YAG laser importantly increased the bond strengths of soft-liner to denture base; however, sandblasting before applying a lining material had a weakening impact on the bond.24 In their study, surface treatments with Nd:YAG and KTP lasers were found to be ineffective with regard to the increase of the strength of the bond and generated different bond values, yet the differences in question were not statistically significant.24 They explained the difference between the Er:YAG laser bond strength and that generated by the Nd:YAG and KTP lasers by the high energy of the Er:YAG laser.24 These controversial results may be explained by the type of lasers, differences in the applied energy and different structures of denture base resins. One possible explanation for the different effects between lasers might be the different absorption capacity of resin materials.
The different behaviors of the denture base acrylic resins may be related to their chemical properties depending on the type of solvent used.14,42 It has also been reported that the bonding between resilient lining materials and denture base materials is affected by the nature of the denture base material.41-43 Three base polymers with different chemical compositions were used in the present study. The Deflex group had greater bond strengths with Molloplast-B than the Paladent and Rodex groups. The relatively high scores of the Deflex group can also be explained by the material's compatibility with (or affinity for) Molloplast-B.
Laser application may cause some chemical changes on the acrylic surface because of the thermal degradation.1,42,43 However, the Er,Cr:YSGG laser serves a coolant to keep the surface temperature low and eliminate any potential detrimental side-effects.34,35 These events were believed to be responsible for the observed increases in the bond strength values of the acrylic specimens treated with Er,Cr:YSGG laser. This can be explained by the high energy of the Er,Cr:YSGG laser. The energy produced by the Er,Cr: YSGG laser might be in interaction with the water droplets at the tissue surface in order to create water molecule excitation causing the water droplet microexpansion and propulsion.33-35 An increased surface area may be formed by this expansion which causes the surrounding material to ablate.24,33-35 Increased surface and mechanical interlocking may be related with the bond strength. It is known that the surface roughness may be increased and the contact angle between PMMA and their control liquids may be decreased, which may help the penetration of the soft liner into the irregularities on the acrylic surface, by the laser application.22
Due to the fact that the force required to produce peeling depends upon the adhesive surface energy, the one between the denture base material and the resilient denture lining material should be explained precisely.7 The surface energy is affected by the surface treatment, and the energy depends on the surface geometries.8,11 The peel energies required on flat surfaces and curved surfaces are quite different. 7 Roughening of the surfaces of the acrylic denture resin is also believed to affect the bond strength with soft lining material in a positive way.32 Storer25 reported that sandblasting the acrylic resin surface prior to placing a resilient liner improved the strength of the bond, with the slightly surface maintaining mechanical locking for the soft material. Adversely, Amin et al.26 declared that roughening the acrylic resin base by alumina-abrasion before applying a lining material had a weakening impact on the bond. Similar to Jacobsen et al.11 and Amin et al.,26 in the present study, it was found that sandblasting the denture base resin with Al2O3 significantly decreased the bond strength of the polyamide resin to the silicone relining material. In the heat-cured and cross-linked resin groups, there were no significant differences after sandblasting. In the literature, authors have different comments about the decrease in the bond strengths with acrylic resin and soft liners. According to Usumez et al.4 the size of the irregularities created by the alumina-abrasion medium might not be sufficient enough to enable the resilient lining material to flow on it. Amin et al.26 suggested that lower bond strengths were due to the pressure which occurred at the interface of the acrylic resin/soft liner junction. Bolayır et al.1 claimed that surface roughening might have stopped the structure of high bond strength since there exists a stress concentration deriving from the discontinuities on the surface. Jacobsen et al.11 was also content with the idea that the capability of the soft lining material to be absorbed into the irrregularities of the acrylic resin is significant for adhesion. Increasing the fluidity of the springy materials for a given contact angle and surface tension decreases the penetration of a material into the irregularities on the acrylic resin surface because the penetration function is reciprocally contingent on viscosity.11 This could explain the lower bond strengths of sandblasted specimens observed in our study. In our opinion, a possible explanation for the controversial results might also be the remnants of the Al2O3 particles. SEM evaluation of the samples showed that roughening methods may improve bonding strengths because of mechanical interlocking, but if the surface of the resin material has debris from the resin material or Al2O3 after the pretreatment, it may decrease the bonding of the two materials chemically. The affinity of Al2O3 for the resin materials and soft liners might be different from that of the tested materials.
Previous studies showed that different repetition rate and power output conditions of laser affect the strength of the bond.18,35 Different energy levels have been used by researchers18 with different lasers, but different pulse frequencies have not been investigated for the Er,Cr:YSGG laser in the surface treatments of acrylic resins. In this present study, irradiation with the Er,Cr:YSGG laser with different pulse frequencies and energy levels resulted in different bond strengths, results similar to those reported by Tugut et al.18 although they used an Er:YAG laser. Moreover, they reported that altering the surface of the acrylic resin by laser significantly increased the bond strength to the silicone lining material, results similar to our study. They found that laser surface irradiation at different energy levels effectively increased the strength of the bond to the soft liner. In this study, we found that different pulse frequencies and different power outputs resulted in different bond strengths to the soft liner.
It has been claimed that in vitro studies may be helpful to foresee the outcome of clinical applications despite the arguments claiming that the results cannot be generalized into vivo conditions.
Kulak-Ozkan et al.44 analysed the thermocycling impact on the tensile bond strength of six silicone-based resilient denture liners and revealed that the tensile bond strength of Parmaflex lessened after thermocycling. However, this reduction was not regarded as statistically significant. Elias et al.42 studied on the effect of thermocycling on the tensile and shear bond strengths of soft liner materials to a denture base acrylic resin. They showed that all soft lining materials tested in their study showed a visible reduction in bond strength on acrylic denture base resin after thermocycling, but all the soft liners tested had higher bond strengths to the denture base than those reported as acceptable for clinical use. Aging of the denture is also an important parameter for the survival of these restorations;42,44,45 the effect of the aging method usually decreases the bond strength, but the amount of this decrease is much more material dependent. Adding the aging factor might add complexity to the understanding of the primary adhesive relationship between the materials.
In further studies, the effect of thermocycling on the bond strength of resin base materials and soft liners after laser and sandblasting pretreatment may also be studied and compared to the current knowledge base on base-liner bonding.
Within the limitations of this study, it can be concluded that heat-cured acrylic resin, PMMA, may benefit from Er,Cr:YSGG laser treatment at 3 W-20 Hz irradiation. Airabrasion of polyamide resins should be avoided not to impair their peel bond strengths to silicon-based soft denture liners.
Figures and Tables
 | Fig. 3SEM images of the laser treated groups for Deflex at (A) 2 W 20 Hz, (B) 2 W 30 Hz, (C) 3 W 20 Hz, (D) 3 W 30 Hz. Note the surface irregularities after laser applications in all groups. |
 | Fig. 4SEM images of the laser treated groups for Paladent at (A) 2 W 20 Hz, (B) 2 W 30 Hz, (C) 3 W 20 Hz, (D) 3 W 30 Hz. Note the surface irregularities in all groups. |
 | Fig. 5SEM images of the laser treated groups for Rodex at (A) 2 W 20 Hz, (B) 2 W 30 Hz, (C) 3 W 20 Hz, (D) 3 W 30 Hz. Note the surface irregularities in all groups. |
Table 2
The results of peel bond strength values (MPa)

*Superscript capital letters indicate significant differences (P<.05) whereas same capital letters indicate no significant differences among the groups in each acrylic material (P>.05). Superscript lower case letters indicate significant differences (P<.05) whereas same lower case letters indicate no significant differences among the acrylic materials in each groups (P>.05).
ACKNOWLEDGMENTS
The authors thank to Dr. Tamer Tuzuner for his assistance in the preparation of this manuscript and evaluating the statistical analysis.
References
1. Bolayır G, Turgut M, Hubbezoğluİ , Doğan OM, Keskin S, Doğan A, Bek B. Evaluation of laser treatment on relinebase composites. J Adhesion. 2007; 83:117–127.
2. Sertgöz A, Kulak Y, Gedik H, Taskonak B. The effect of thermocycling on peel strength of six soft lining materials. J Oral Rehabil. 2002; 29:583–587.
3. Hatamleh MM, Watts DC. Bonding of maxillofacial silicone elastomers to an acrylic substrate. Dent Mater. 2010; 26:387–395.
4. Usumez A, Inan O, Aykent F. Bond strength of a silicone lining material to alumina-abraded and lased denture resin. J Biomed Mater Res B Appl Biomater. 2004; 71:196–200.
5. Haselden CA, Hobkirk JA, Pearson GJ, Davies EH. A comparison between the wear resistance of three types of denture resin to three different dentifrices. J Oral Rehabil. 1998; 25:335–339.
6. Al-Athel M, Jagger R, Jagger D. Effect of ageing on the bond strength of a permanent denture soft lining material. J Oral Rehabil. 2002; 29:992–996.
7. Tanimoto Y, Saeki H, Kimoto S, Nishiwaki T, Nishiyama N. Evaluation of adhesive properties of three resilient denture liners by the modified peel test method. Acta Biomater. 2009; 5:764–769.
8. Machado AL, Breeding LC, Puckett AD. Effect of microwave disinfection on the hardness and adhesion of two resilient liners. J Prosthet Dent. 2005; 94:183–189.
9. Sarac D, Sarac YS, Basoglu T, Yapici O, Yuzbasioglu E. The evaluation of microleakage and bond strength of a silicone-based resilient liner following denture base surface pretreatment. J Prosthet Dent. 2006; 95:143–151.
10. Kawano F, Ohguri T, Koran A III, Matsumoto N, Ichikawa T. Influence of lining design of three processed soft denture liners on cushioning effect. J Oral Rehabil. 1999; 26:962–968.
11. Jacobsen NL, Mitchell DL, Johnson DL, Holt RA. Lased and sandblasted denture base surface preparations affecting resilient liner bonding. J Prosthet Dent. 1997; 78:153–158.
12. Pinto JR, Mesquita MF, Henriques GE, de Arruda Nóbilo MA. Effect of thermocycling on bond strength and elasticity of 4 long-term soft denture liners. J Prosthet Dent. 2002; 88:516–521.
13. Aydin AK, Terzioğlu H, Akinay AE, Ulubayram K, Hasirci N. Bond strength and failure analysis of lining materials to denture resin. Dent Mater. 1999; 15:211–218.
14. McCabe JF, Carrick TE, Kamohara H. Adhesive bond strength and compliance for denture soft lining materials. Biomaterials. 2002; 23:1347–1352.
15. Pisani MX, Silva-Lovato CH, Malheiros-Segundo Ade L, Macedo AP, Paranhos HF. Bond strength and degree of infiltration between acrylic resin denture liner after immersion in effervescent denture cleanser. J Prosthodont. 2009; 18:123–129.
16. Kawano F, Dootz ER, Koran A 3rd, Craig RG. Comparison of bond strength of six soft denture liners to denture base resin. J Prosthet Dent. 1992; 68:368–371.
17. Waters MG, Jagger RG. Mechanical properties of an experimental denture soft lining material. J Dent. 1999; 27:197–202.
18. Tugut F, Akin H, Mutaf B, Akin GE, Ozdemir AK. Strength of the bond between a silicone lining material and denture resin after Er:YAG laser treatments with different pulse durations and levels of energy. Lasers Med Sci. 2012; 27:281–285.
19. Baysan A, Parker S, Wright PS. Adhesion and tear energy of a long-term soft lining material activated by rapid microwave energy. J Prosthet Dent. 1998; 79:182–187.
20. Braden M, Wright PS, Parker S. Soft lining materials-a review. Eur J Prosthodont Restor Dent. 1995; 3:163–174.
21. Anusavice KJ, Phillips RW. Phillip's science of dental materials. 11th ed. St. Louis: Elsevier;2003. p. 751–753.
22. Lawrence J, Li L. Modification of the wettability characteristics of polymethyl methacrylate (PMMA) by means of CO2, Nd:YAG, excimer and high power diode laser radiation. Mater SciEng A. 2001; 303:142–149.
23. Saraç YS, Başoğlu T, Ceylan GK, Saraç D, Yapici O. Effect of denture base surface pretreatment on microleakage of a silicone-based resilient liner. J Prosthet Dent. 2004; 92:283–287.
24. Akin H, Tugut F, Mutaf B, Akin G, Ozdemir AK. Effect of different surface treatments on tensile bond strength of silicone-based soft denture liner. Lasers Med Sci. 2011; 26:783–788.
25. Storer R. Resilient denture base materials. Part 1. Introduction and laboratory evaluation. Br Dent J. 1962; 113:195–203.
26. Amin WM, Fletcher AM, Ritchie GM. The nature of the interface between polymethyl methacrylate denture base materials and soft lining materials. J Dent. 1981; 9:336–346.
27. Akin H, Tugut F, Guney U, Kirmali O, Akar T. Tensile bond strength of silicone-based soft denture liner to two chemically different denture base resins after various surface treatments. Lasers Med Sci. 2013; 28:119–123.
28. Zhang H, Fang J, Hu Z, Ma J, Han Y, Bian J. Effect of oxygen plasma treatment on the bonding of a soft liner to an acrylic resin denture material. Dent Mater J. 2010; 29:398–402.
29. Minami H, Suzuki S, Ohashi H, Kurashige H, Tanaka T. Effect of surface treatment on the bonding of an autopolymerizing soft denture liner to a denture base resin. Int J Prosthodont. 2004; 17:297–301.
30. Yanikoglu N, Denizoglu S. The effect of different solutions on the bond strength of soft lining materials to acrylic resin. Dent Mater J. 2006; 25:39–44.
31. Shimizu H, Ikuyama T, Hayakawa E, Tsue F, Takahashi Y. Effect of surface preparation using ethyl acetate on the repair strength of denture base resin. Acta Odontol Scand. 2006; 64:159–163.
32. Craig RG, Gibbons P. Properties of resilient denture liners. J Am Dent Assoc. 1961; 63:382–390.
33. Baygin O, Korkmaz FM, Tüzüner T, Tanriver M. The effect of different enamel surface treatments on the microleakage of fissure sealants. Lasers Med Sci. 2012; 27:153–160.
34. Botta SB, da Ana PA, Zezell DM, Powers JM, Matos AB. Adhesion after erbium, chromium:yttrium-scandium-galliumgarnetlaser application at three different irradiation conditions. Lasers Med Sci. 2009; 24:67–73.
35. Başaran EG, Ayna E, Başaran G, Beydemir K. Influence of different power outputs of erbium, chromium:yttrium-scandium-gallium-garnet laser and acid etching on shear bond strengths of a dual-cure resin cement to enamel. Lasers Med Sci. 2011; 26:13–19.
36. Wright PS. Characterization of the adhesion of soft lining materials to poly(methyl methacrylate). J Dent Res. 1982; 61:1002–1005.
37. Mutluay MM, Ruyter IE. Evaluation of bond strength of soft relining materials to denture base polymers. Dent Mater. 2007; 23:1373–1381.
38. Ucar Y, Akova T, Aysan I. Mechanical properties of polyamide versus different PMMA denture base materials. J Prosthodont. 2012; 21:173–176.
39. Yunus N, Rashid AA, Azmi LL, Abu-Hassan MI. Some flexural properties of a nylon denture base polymer. J Oral Rehabil. 2005; 32:65–71.
40. al-Athel MS, Jagger RG. Effect of test method on the bond strength of a silicone resilient denture lining material. J Prosthet Dent. 1996; 76:535–540.
41. Kutay O. Comparison of tensile and peel bond strengths of resilient liners. J Prosthet Dent. 1994; 71:525–531.
42. Elias CN, Henriques FQ. Effect of thermocycling on the tensile and shear bond strengths of three soft liners to a denture base resin. J Appl Oral Sci. 2007; 15:18–23.
43. Süske E, Scharf T, Schaaf P, Panchenko E, Nelke D, Buback M, Kijewski H, Krebs HU. Variation of mechanical properties of pulsed laser deposited PMMA films during annealing. Appl Phys A. 2004; 79:1295–1297.
44. Kulak-Ozkan Y, Sertgoz A, Gedik H. Effect of thermocycling on tensile bond strength of six silicone-based, resilient denture liners. J Prosthet Dent. 2003; 89:303–310.
45. Oguz S, Mutluay MM, Dogan OM, Bek B. Effect of thermocycling on tensile strength and tear resistance of four soft denture liners. Dent Mater J. 2007; 26:296–302.




 PDF
PDF ePub
ePub Citation
Citation Print
Print







 XML Download
XML Download