Abstract
PURPOSE
Few studies have investigated the marginal accuracy of 3-unit zirconia fixed partial dentures (FPDs) fabricated by computer-aided design/computer-aided manufacturing (CAD/CAM) system. The purpose of this study was to compare the marginal fit of zirconia FPDs made using two CAD/CAM systems with that of metal-ceramic FPDs.
MATERIALS AND METHODS
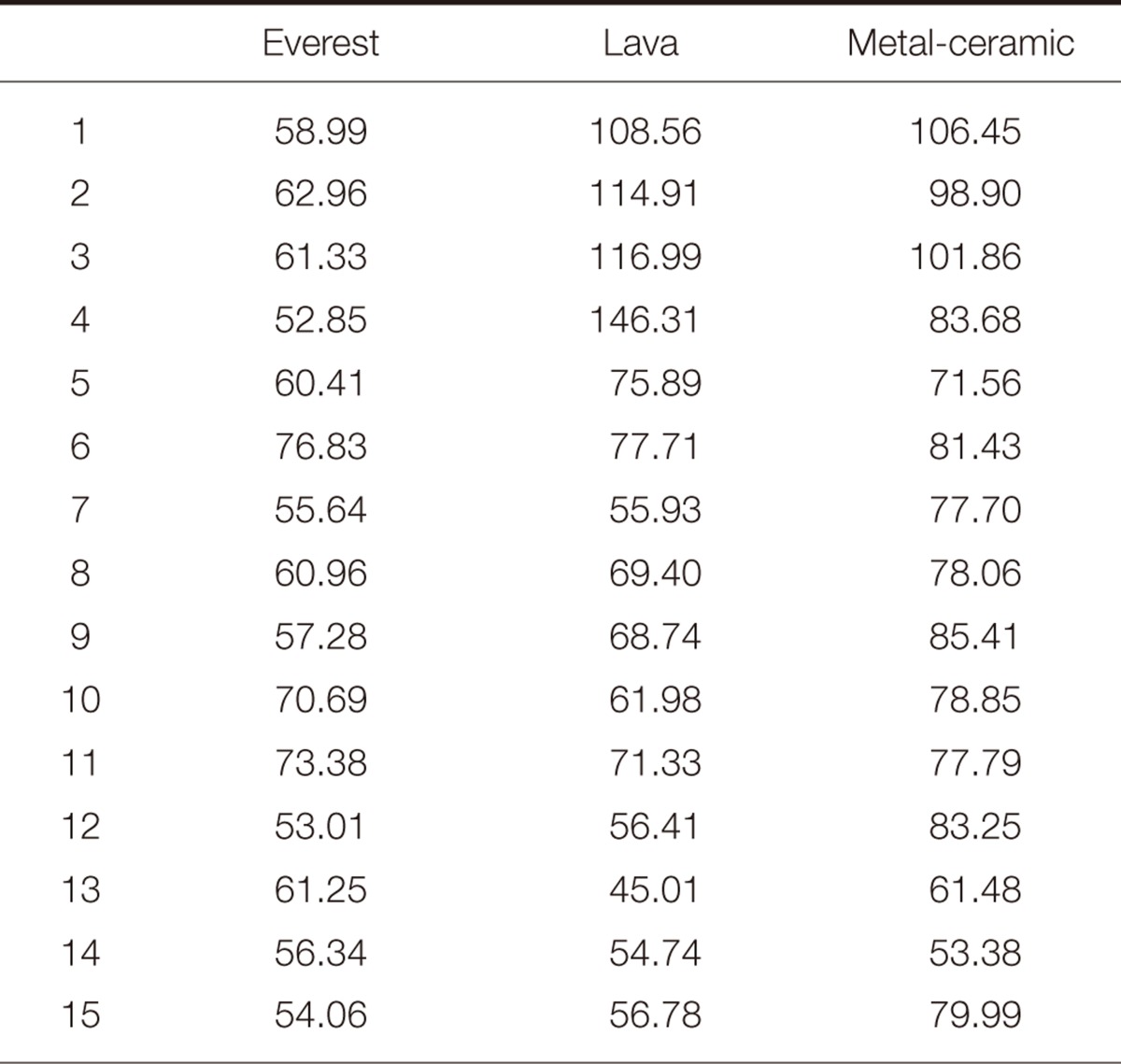
Artificial resin maxillary central and lateral incisors were prepared for 3-unit FPDs and fixed in yellow stone. This model was duplicated to epoxy resin die. On the resin die, 15 three-unit FPDs were fabricated per group (45 in total): Group A, zirconia 3-unit FPDs made with the Everest system; Group B, zirconia 3-unit FPDs made with the Lava system; and Group C, metal-ceramic 3-unit FPDs. They were cemented to resin dies with resin cement. After removal of pontic, each retainer was separated and observed under a microscope (Presize 440C). Marginal gaps of experimental groups were analyzed using one-way ANOVA and Duncan test.
RESULTS
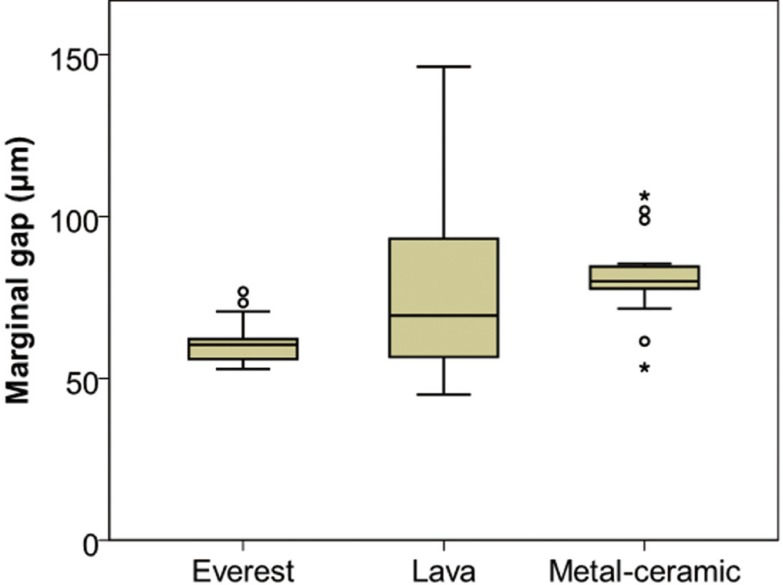
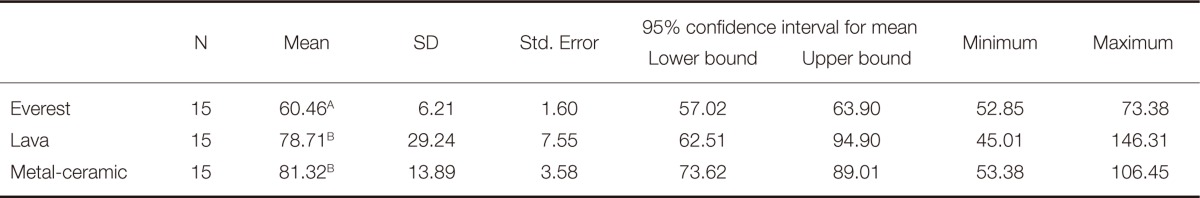
Mean marginal gaps of 3-unit FPDs were 60.46 µm for the Everest group, 78.71 µm for the Lava group, and 81.32 µm for the metal-ceramic group. The Everest group demonstrated significantly smaller marginal gap than the Lava and the metal-ceramic groups (P<.05). The marginal gap did not significantly differ between the Lava and the metal-ceramic groups (P>.05).
Marginal fit is an important characteristic that can contribute to the clinical performance of a fixed restoration. Inaccurate margins allow plaque accumulation or marginal leakage, which can lead to periodontal disease, bone loss, or secondary dental caries.1,2 The introduction of high-strength oxide ceramic has resulted in the widespread use of all-ceramic restorations in dentistry. However, marginal fit remains critical to ensure long-term success of metal-free fixed prosthodontic restorations.
When computer-aided design/computer-aided manufacturing (CAD/CAM) technology is used to make all-ceramic restorations, the fit can be set for each abutment tooth with software that customizes the marginal gap for the clinical situation. The ability of CAD/CAM technology to implement the predetermined fit depends on the accuracy of the entire system including the scanning device, milling material, and milling unit. It also relies on exact dimensional prediction to compensate for sintering shrinkage. The CAD/CAM technique is an economical and reproducible method which has been demonstrated to improve marginal fit.3-5
The clinically acceptable limit for marginal gaps has been reported to range from 100 to 120 µm.6,7 Several studies have demonstrated that high precision can be achieved with CAD/CAM-generated zirconia restorations.8-11 Nevertheless, in a previous clinical long-term study, many zirconia restorations exhibited defective margins, often due to inadequate marginal integrity.12 Such poor margins were reported to indicate a higher failure rate of restorations.12,13 Although the accuracy of fit has a considerable effect on the clinical success of the restorations, only a few studies related with this aspect of zirconium oxide ceramics generated with CAD/CAM have been published.8-11 In addition, the effects of CAD/CAM systems and materials on the size of the marginal discrepancy have not been thoroughly investigated.
The lost wax technique for the cast metal framework of metal-ceramic restoration is well established and, when properly used, leads to clinically acceptable fit on the abutment teeth. Therefore, the marginal accuracy of metalceramic restorations frequently serves as the "gold-standard" in testing the precision of a new technique.14 Since a CAD/CAM-based technique has to compete with a conventional casting method, the quality of CAD/CAM-manufactured restorations needs to be compared with that of metal-ceramic restorations. This study was designed to assess the marginal fits of 3-unit anterior fixed partial dentures (FPDs) made of metal-ceramics by casting, and of zirconia using two different CAD/CAM systems.
A resin maxillary right central incisor and a maxillary left lateral incisor analogue (Nissin Dental Products Inc., Kyoto, Japan) were fixed in yellow stone (Neo Plumstone, Mutsumi Chemical Industries Co., Ltd., Mutsumi, Japan) with their axes parallel to each other and vertical to the earth. The distance between the 2 teeth was as wide as a maxillary central incisor (Fig. 1A). These resin teeth were prepared for an all-ceramic FPD. Following a standardized preparation protocol, the abutment teeth were prepared using a high-speed angled handpiece and diamond rotary cutting instruments under water cooling. Incisal and axial reduction were performed. The analogues were finished by milling (Cruise; Silfradent, Sofia, Italy), which resulted in 1 mm shoulder margin with 12° tapered angle and an approximate height of 8 mm (central incisor) and 7 mm (lateral incisor).
Forty-five silicone impressions were made according to the manufacturer's directions. Putty (Aquasil Soft Putty-Regular Set; Dentsply DeTrey GmbH, Konstanz, Germany) was used to load an impression tray, and light-bodied silicone impression material (Aquasil Ultra XLV; Dentsply Caulk, Milford, USA) was syringed around the abutments. Epoxy die material (Polyurock; Metalor Dental GmbH, Stuttgart, Germany) was used to pour the impressions following the manufacturer's instructions, after which 45 epoxy resin dies were fabricated (Fig. 1B). To verify the dimensions of the epoxy resin dies, metal copings of central and lateral incisors were connected with pattern resin. This metal coping jig was used to confirm that the duplicated die had the same sizes 3-dimensionally (Fig. 1C). The metal coping accurately fitted all the duplicated dies. These epoxy dies served as the respective master dies.
A total of 45 three-unit FPDs were fabricated, comprising 3 groups of 15 specimens each. Group A consisted of 15 three-unit FPDs fabricated by the Everest system (Kavo Dental GmbH, Biberach, Germany). In the Everest system, optical scanned data of epoxy dies (active triangulation and stripe pattern projection; Everest Scan Pro; Kavo Dental GmbH) formed the basis for the CAD design of the FPDs (Energy CAD; Kavo Dental GmbH). The pre-sintered, enlarged frameworks (ZS-Blanks [ZS]; Kavo Dental GmbH) in a 5-axis milling machine (Everest Engine; Kavo Dental GmbH) were sintered to their original size in a furnace (Everest Therm; Kavo Dental GmbH).15 IPS e.max Ceram layering ceramic (Ivoclar Vivadent AG, Schann, Liechtenstein) was used (Fig. 1D).
Group B consisted of 15 three-unit FPDs fabricated by the Lava™ system (3M ESPE, Seefeld, Germany). Fifteen epoxy resin dies were digitized by an optical scanner (Lava™ Scan ST; 3M ESPE), and the frameworks were designed (Lava™ CAD; 3M ESPE). A computer-aided machine (Lava™ Form; 3M ESPE) milled a partially sintered block, producing a framework, which was enlarged to compensate for sintering shrinkage. Blocks were then sintered to their final dimensions in a sintering oven (Lava™ Therm; 3M ESPE). Lava™ Ceram layering ceramic (3M ESPE) was used (Fig. 1E). Group C consisted of 15 three-unit metal-ceramic FPDs made using the traditional lost-wax technique. The frameworks were made of Ni-Cr-Mo alloy (VeraBond®; Aalba Dent Inc., Fairfield, CA, USA) using a centrifugal casting machine. Porcelain build-up was carried out with feldspathic porcelain powder (Noritake EX-3; Noritake Dental Supply Co., Ltd., Aichi, Japan) (Fig. 1F).
Experienced dental technicians who were accustomed to the specific systems fabricated each group of FPDs. All FPDs were fabricated according to their respective manufacturer's recommendations. The overall contour and thickness of FPDs was checked with a prepared index and metal gauge. In order to prevent scratches and distortion of the resin master dies, every FPD was adapted to a spare resin die. When necessary, fitting adjustments were made by removing interference. After adjustment, the completed FPDs were adapted on the respective master dies.
All FPDs were placed onto their original dies with self-adhesive resin cement (RelyX Unicem; 3M ESPE) after the prepared resin dies were cleaned. As in clinical procedure, finger pressure was applied at the incisal tip of the pontic area during the cementing procedure. After light curing for 2 seconds, while the cement was in the gel state, excess cement was removed with an explorer, and it was then allowed to self-cure for 5 minutes from the start of mixing. These dies were left at room temperature. After 24 hours, the pontics were removed using a diamond disk, and then epoxy dies were separated at the middle area. Consequently, 45 central incisor specimens and 45 lateral incisor specimens were acquired.
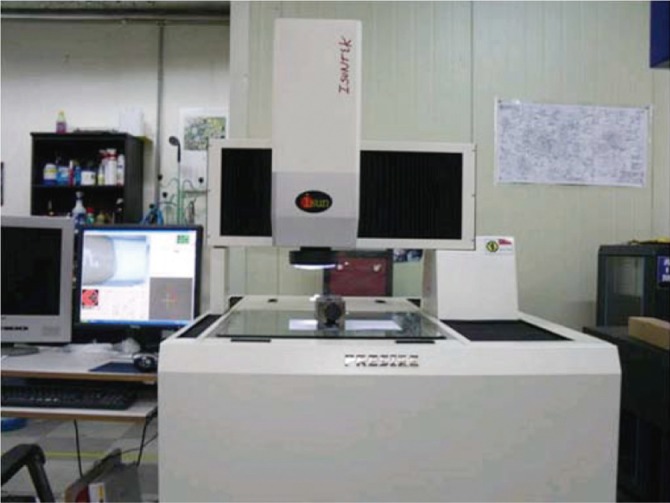
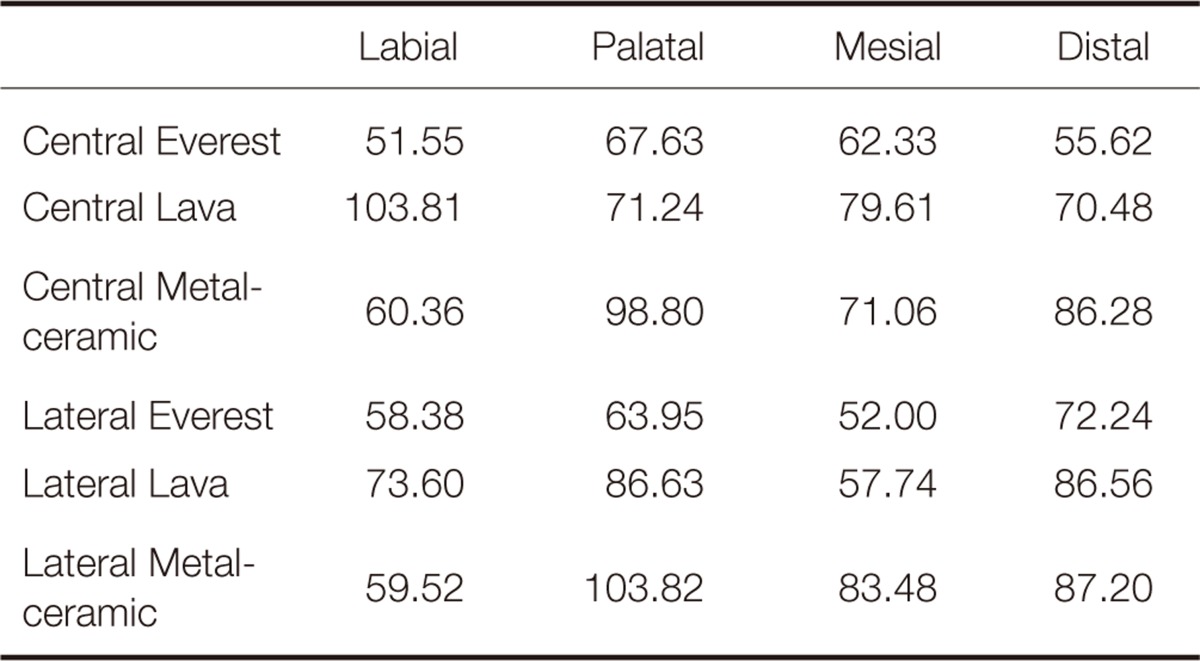
The marginal fit was evaluated by measuring the gap between the edge of the crown and the prepared tooth margin. All the prepared single tooth specimens were observed under a measuring machine with image processing software (Presize 440C; Isuntek Co., Ltd., New Taipei, Taiwan) at an original magnification of ×145 (Fig. 2). The resolution of the microscope was 0.5 µm. For the marginal gap measurement, along with vertical planes, 4 landmarks at the central and lateral incisors (mesial, distal, labial, and palatal) were defined. All measurements were performed by the same technician to avoid statistical variance as much as possible.
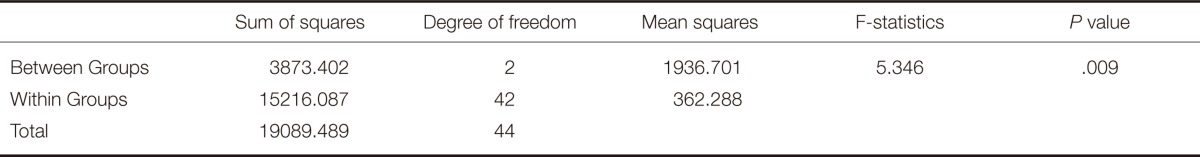
Means and standard deviations of the 8 landmarks were calculated for each of the 3 groups. One-way ANOVA test and a post-hoc test (Duncan test) were used to find any statistical significance among the groups at the .05 level of significance.
The marginal fits measured under measuring machine are shown in Table 1 and Table 2. Typical appearances of external margins are shown in Fig. 3. The means and standard deviations of gap dimensions were 60.46 ± 6.21 µm for the Everest group, 78.71 ± 29.24 µm for the Lava group, and 81.32 ± 13.89 µm for the metal-ceramic group (Table 3). The distributions of gap dimensions for the 3 groups are shown in Fig. 4. The means and standard deviations of the average gap dimensions of each group were statistically analyzed with one-way ANOVA (Table 4) and Duncan test (Table 3). The Everest group demonstrated a significantly smaller marginal gap than the other groups (P<.05). Marginal gap did not significantly differ between the Lava and metal-ceramic groups (P>.05). Considering 120 µm as the limit of clinical acceptability,6 the mean marginal gaps of each group were found to be clinically acceptable.
The marginal fit of CAD/CAM-fabricated zirconia restorations is influenced by several factors. CAD/CAM techniques include scanning, software-based design, and milling; each procedure could have an effect on the overall fit of a restoration. Therefore, different CAD/CAM systems may significantly affect the quality of marginal fit. For example, a large internal gap would result from an internal cutting bur larger than some parts of the tooth preparation according to manufacturing techniques and tools.16 Zirconia material itself may also affect the marginal fit. Frameworks of fully sintered zirconia show significantly more precise marginal fit than those of pre-sintered zirconium oxide.17
Simplifying fabrication procedures by eliminating several steps like waxing and investing enhances accuracy in the CAD/CAM technology. In this study, 2 different CAD/CAM systems were compared with the conventional method. The mean marginal gap of the 2 different CAD/CAM systems used in this study was in accordance with or smaller than that of the metal-ceramic restorations.
The marginal accuracy of Lava 3-unit FPDs was similar to that of the metal-ceramic group, which is in accordance with the results of previous studies on Lava and metal-ceramic restorations.10,11,18 Gonzalo et al.18 analyzed marginal fit in metal-ceramic and zirconia posterior 3-unit bridges with an image analysis program and scanning electron microscope. In that study, the Lava and metal-ceramic groups showed similar discrepancies with image analysis (71 ± 45 µm and 76 ± 29 µm, respectively) while scanning electron microscopy revealed lower values for the metal-ceramic group (65 ± 26 µm) compared with the Lava group (76 ± 37 µm), but with no significant difference observed between groups. In a previous in vivo study, Reich et al.11 evaluated the marginal and internal fit of Lava 3-unit FPDs by replica technique with a light-bodied polyvinylsiloxane stabilized by heavy-bodied one. In that study, the mean marginal gap of Lava FPDs was 65 µm, similar to those of metal-ceramic restoration. Beuer et al.10 also reported that the accuracy of the Lava system is clinically satisfactory.
The Everest system demonstrated decreased marginal gap compared to the metal-ceramic group. The measured marginal gaps of the Everest system were in the same range as values reported in a previous study by Vigolo and Fonzi, who microscopically analyzed marginal fit in zirconia 4-unit FPDs at ×50 magnification.19 In that study, the mean marginal gap of the Everest system was 65.49 µm.19 In contrast, Kohorst et al. reported that the mean marginal gap of the Everest system was 112.8 µm, and in Abduo's review article, the average value of the absolute marginal discrepancy for zirconia FPDs made with Everest systems was 148.8 µm.16,20 These results are not in agreement with the present findings, which can be explained by the variation in the method used to analyze marginal accuracy. The results in this study were obtained under experimental conditions with standardized dies, and the measurements were performed directly on the casts, where the frameworks were created. In the study by Kohorst et al., a replica technique was used.20 Another study using 4-unit FPDs indicated too short margins of the Everest framework despite the satisfactory horizontal marginal fit.15
In this study, the Everest group demonstrated significantly smaller (P<.05) marginal gaps than the Lava group. While the CAD/CAM systems are similar to each other in fabricating zirconia restorations, there are differences in the fabrication process between the systems. Differences in the efficiency of CAD software compensating for the sintering shrinkage, the constant quality of green bodies, and the sintering stability may make the Everest system more precise in marginal accuracy. Processing devices also influence marginal fit. In the case of the Lava, a 3-axis device was used, while a 5-axis milling device was used for the Everest system. This difference may be another factor contributing to the results. However, Beuer et al. stated that restoration quality does not necessarily improve as the number of processing axes increases.21 Additionally, quality results in large part from the digitization, data processing, and production process.
Another possibility is that larger internal misfit may have caused low marginal gap measurement. In general, the framework was tested on the master model, and the internal surface was adjusted until the marginal gap was maximally well adapted. Such an effort in marginal adaptation also affects marginal opening. In this study, different dental laboratories fabricated Everest and Lava FPDs, and thus different adaptation processes may have been performed. In this adaptation stage, manual skills and the experience of the dental technician have a definite influence on both the marginal and internal fit.22
The internal and marginal accuracy are important for the longevity of a restoration. Gap widths usually increase from the margin to the occlusal surface of the crown, where the gap is the widest. Small marginal openings have been shown to correlate with larger internal gap values of 100-200 µm in vitro.23 Misfits in the axial wall area and occlusal plateau can reduce the fracture resistance of all-ceramic restorations.24 One limitation of this experimental study is that only the marginal fit was evaluated to assess the precision of restorations; the internal fit of the restorations was not considered. Belles et al. reported that the internal marginal fits were generally poorer than the external facial marginal fit,25 and several authors have studied the internal fit of restorations.26-28 Further investigations are needed to measure both the marginal and internal fits.
In this study, all specimens were cemented to their respective resin dies. For the measurement of interproximal pontic area, the pontic was removed with diamond disk. The measurement of marginal gaps without cementation is possible, but this method is inaccurate because the fixation of the specimen is unstable. It is well known that the marginal discrepancy generally increases after cementation, which occurs clinically. Thus, to correctly determine the marginal discrepancy, its evaluation after cementation was necessary.
Okutan et al.17 demonstrated that marginal openings were significantly higher after cementation in the Everest system. In this study, finger pressure was used for definitive placement of the restorations. Although this procedure simulates a clinical procedure, it should be considered as a limitation of this study, as finger pressure is variable, and the pressure load cannot be standardized.29 According to Rosentritt et al., zirconia FPDs demonstrated adequate marginal integrity when a cementing medium was Panavia/ED, Compolute/EBS, or RelyX Unicem.30 In this study, RelyX Unicem was used for cementation because of easy handling.
McLean and von Fraunhofer proposed that a successful restoration was possible if restorations could be constructed so that marginal gaps and cement films of less than 120 µm were achieved.6 Many studies have used this criterion for the evaluation although debates still exist regarding a clinically acceptable margin.31-33 Therefore, the value of 120 µm was used as the maximum clinically acceptable marginal opening in the present investigation. The marginal gaps recorded were all within this clinically acceptable standard. The marginal gaps of anterior 3-unit zirconia FPD show differences according to CAD/CAM systems, but still show clinically acceptable ranges in comparison with the conventional metal-ceramic restoration.
In this study, the investigated FPDs experienced no artificial aging process. Artificial aging was previously shown to influence the marginal integrity of all-ceramic FPDs.34 However, Att et al. found no significant change in the marginal fit of zirconia FPDs after masticatory and thermal stimulation.29 Although aging has not been proven to cause marginal deterioration of zirconia prostheses, more investigations are needed on the effects of the aging process.
While in vitro studies offer standard conditions with respect to preparation design, impression technique, and experimental performance, clinical evaluations include various real conditions that deviate from such controlled situations. Thus, further investigations are needed to measure both the marginal and internal fits in vivo and to evaluate the influence of clinical aging on marginal distortion. Nevertheless, the present study supports the good performance of CAD/CAM design in three-unit zirconia FPD while also highlighting the effect of different CAD/CAM systems on FPD fabrication.
References
1. Sorensen JA. A rationale for comparison of plaque-retaining properties of crown systems. J Prosthet Dent. 1989; 62:264–269. PMID: 2681694.

2. Sorensen SE, Larsen IB, Jörgensen KD. Gingival and alveolar bone reaction to marginal fit of subgingival crown margins. Scand J Dent Res. 1986; 94:109–114. PMID: 3518035.

3. Abbate MF, Tjan AH, Fox WM. Comparison of the marginal fit of various ceramic crown systems. J Prosthet Dent. 1989; 61:527–531. PMID: 2664137.

4. Yeo IS, Yang JH, Lee JB. In vitro marginal fit of three all-ceramic crown systems. J Prosthet Dent. 2003; 90:459–464. PMID: 14586310.

5. Gonzalo E, Suárez MJ, Serrano B, Lozano JF. A comparison of the marginal vertical discrepancies of zirconium and metal ceramic posterior fixed dental prostheses before and after cementation. J Prosthet Dent. 2009; 102:378–384. PMID: 19961996.

6. McLean JW, von Fraunhofer JA. The estimation of cement film thickness by an in vivo technique. Br Dent J. 1971; 131:107–111. PMID: 5283545.

7. Belser UC, MacEntee MI, Richter WA. Fit of three porcelain-fused-to-metal marginal designs in vivo: a scanning electron microscope study. J Prosthet Dent. 1985; 53:24–29. PMID: 3882944.

8. Coli P, Karlsson S. Precision of a CAD/CAM technique for the production of zirconium dioxide copings. Int J Prosthodont. 2004; 17:577–580. PMID: 15543914.

9. Tinschert J, Natt G, Mautsch W, Spiekermann H, Anusavice KJ. Marginal fit of alumina-and zirconia-based fixed partial dentures produced by a CAD/CAM system. Oper Dent. 2001; 26:367–374. PMID: 11504436.
10. Beuer F, Naumann M, Gernet W, Sorensen JA. Precision of fit: zirconia three-unit fixed dental prostheses. Clin Oral Investig. 2009; 13:343–349.

11. Reich S, Wichmann M, Nkenke E, Proeschel P. Clinical fit of all-ceramic three-unit fixed partial dentures, generated with three different CAD/CAM systems. Eur J Oral Sci. 2005; 113:174–179. PMID: 15819826.

12. Sailer I, Fehér A, Filser F, Gauckler LJ, Lüthy H, Hämmerle CH. Five-year clinical results of zirconia frameworks for posterior fixed partial dentures. Int J Prosthodont. 2007; 20:383–388. PMID: 17695869.
13. Sailer I, Fehér A, Filser F, Lüthy H, Gauckler LJ, Schärer P, Franz Hämmerle CH. Prospective clinical study of zirconia posterior fixed partial dentures: 3-year follow-up. Quintessence Int. 2006; 37:685–693. PMID: 17017630.
14. Wettstein F, Sailer I, Roos M, Hämmerle CH. Clinical study of the internal gaps of zirconia and metal frameworks for fixed partial dentures. Eur J Oral Sci. 2008; 116:272–279. PMID: 18471247.

15. Kohorst P, Brinkmann H, Li J, Borchers L, Stiesch M. Marginal accuracy of four-unit zirconia fixed dental prostheses fabricated using different computer-aided design/computer-aided manufacturing systems. Eur J Oral Sci. 2009; 117:319–325. PMID: 19583762.

16. Abduo J, Lyons K, Swain M. Fit of zirconia fixed partial denture: a systematic review. J Oral Rehabil. 2010; 37:866–876. PMID: 20557435.

17. Okutan M, Heydecke G, Butz F, Strub JR. Fracture load and marginal fit of shrinkage-free ZrSiO4 all-ceramic crowns after chewing simulation. J Oral Rehabil. 2006; 33:827–832. PMID: 17002742.
18. Gonzalo E, Suárez MJ, Serrano B, Lozano JF. Comparative analysis of two measurement methods for marginal fit in metal-ceramic and zirconia posterior FPDs. Int J Prosthodont. 2009; 22:374–377. PMID: 19639075.
19. Vigolo P, Fonzi F. An in vitro evaluation of fit of zirconium-oxide-based ceramic four-unit fixed partial dentures, generated with three different CAD/CAM systems, before and after porcelain firing cycles and after glaze cycles. J Prosthodont. 2008; 17:621–626. PMID: 18798783.

20. Kohorst P, Brinkmann H, Dittmer MP, Borchers L, Stiesch M. Influence of the veneering process on the marginal fit of zirconia fixed dental prostheses. J Oral Rehabil. 2010; 37:283–291. PMID: 20059649.

21. Beuer F, Schweiger J, Edelhoff D. Digital dentistry: an overview of recent developments for CAD/CAM generated restorations. Br Dent J. 2008; 204:505–511. PMID: 18469768.

22. Witkowski S, Komine F, Gerds T. Marginal accuracy of titanium copings fabricated by casting and CAD/CAM techniques. J Prosthet Dent. 2006; 96:47–52. PMID: 16872930.

23. Bindl A, Mörmann WH. Marginal and internal fit of all-ceramic CAD/CAM crown-copings on chamfer preparations. J Oral Rehabil. 2005; 32:441–447. PMID: 15899023.

24. Tuntiprawon M, Wilson PR. The effect of cement thickness on the fracture strength of all-ceramic crowns. Aust Dent J. 1995; 40:17–21. PMID: 7710410.

25. Belles DM, Cronin RJ Jr, Duke ES. Effect of metal design and technique on the marginal characteristics of the collarless metal ceramic restoration. J Prosthet Dent. 1991; 65:611–619. PMID: 2051380.

26. Yoon JW, Yang JH, Han JS, Lee JB. A study on the marginal fit of collarless metal ceramic fixed partial dentures. J Korean Acad Prosthodont. 2005; 43:707–716.
27. Bindl A, Mörmann WH. Fit of all-ceramic posterior fixed partial denture frameworks in vitro. Int J Periodontics Restorative Dent. 2007; 27:567–575. PMID: 18092451.
28. Beuer F, Aggstaller H, Richter J, Edelhoff D, Gernet W. Influence of preparation angle on marginal and internal fit of CAD/CAM-fabricated zirconia crown copings. Quintessence Int. 2009; 40:243–250. PMID: 19417888.
29. Att W, Komine F, Gerds T, Strub JR. Marginal adaptation of three different zirconium dioxide three-unit fixed dental prostheses. J Prosthet Dent. 2009; 101:239–247. PMID: 19328277.

30. Rosentritt M, Behr M, Kolbeck C, Handel G. Marginal integrity of CAD/CAM fixed partial dentures. Eur J Dent. 2007; 1:25–30. PMID: 19212494.
31. May KB, Russell MM, Razzoog ME, Lang BR. Precision of fit: the Procera AllCeram crown. J Prosthet Dent. 1998; 80:394–404. PMID: 9791784.

32. Leong D, Chai J, Lautenschlager E, Gilbert J. Marginal fit of machine-milled titanium and cast titanium single crowns. Int J Prosthodont. 1994; 7:440–447. PMID: 7802912.
33. Sulaiman F, Chai J, Jameson LM, Wozniak WT. A comparison of the marginal fit of In-Ceram, IPS Empress, and Procera crowns. Int J Prosthodont. 1997; 10:478–484. PMID: 9495168.
34. Stappert CF, Dai M, Chitmongkolsuk S, Gerds T, Strub JR. Marginal adaptation of three-unit fixed partial dentures constructed from pressed ceramic systems. Br Dent J. 2004; 196:766–770. PMID: 15220983.

Fig. 1
(A) Prepared resin teeth, (B) Epoxy resin die for final restoration, (C) Metal coping jig, (D) Three-unit zirconia anterior fixed partial denture fabricated using the Everest system, (E) Three-unit zirconia anterior fixed partial denture fabricated using the Lava system, (F) Three-unit metal-ceramic FPD.
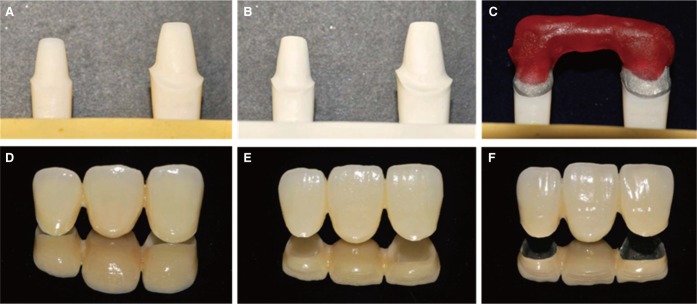
Fig. 3
Photographs of labial surface marginal gap using Presize 440C (×145 magnification). (A) Everest system, (B) Lava system, (C) Metal-ceramic (The luting cement showed black color because of the shadow of the metal framework).
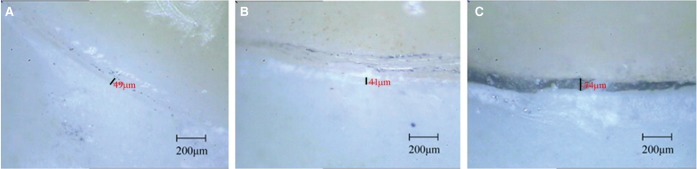
Fig. 4
Boxplot of marginal gaps for the 3 experimental groups. The Everest group demonstrated significantly smaller values than the Lava and metal-ceramic groups. The small circles and stars stand for the mild and severe outliers, respectively.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download