Abstract
This clinical report presents the reconstruction of a maxillary arch with a cement retained implant supported fixed prosthesis using a monolithic zirconia generated by CAD/CAM system on eight osseointegrated implants. The prosthesis was copy milled from an interim prosthesis minimizing occlusal adjustments on the definitive prosthesis at the time of delivery. Monolithic zirconia provides high esthetics and reduces the number of metal alloys used in the oral cavity.
Full mouth reconstruction of an edentulous patient using osseointegrated implants is a well accepted treatment in dentistry. The treatment challenges prosthodontists when vertical and horizontal tissue resorption limits the desired implant position and prosthesis type. Although some of the lost tissue may be reestablished, challenges still exist. To reestablish function, esthetics, and gingival architecture, different material combinations have been employed including metal alloy-acrylic, metal alloy-composite, metal alloy-ceramic, and zirconia-ceramic.1-5
A variety of clinical problems have been reported with metal alloy-acrylic implant supported prostheses. This includes mechanical problems such as fractured or debonded acrylic resin teeth, a lack of biologic color especially at the prosthetic gingival architecture, and wear of the opposing surfaces in long term. As a result, high maintenance of the prosthesis, replacement of acrylic teeth, and unpleasing gingival architecture are common clinical complications.1,2,6,7
The limited number of literature on metal alloy-composite implant supported prosthesis for edentulous patients. However, in vitro studies have shown higher wear resistance for composite resin compared to acrylic resin.6,8 Pink colored composite resins also offer the advantage of creating esthetic gingival architecture in combination with different materials.9-11 Although the shape, shade, and the texture of the tissue can be controlled with pink colored composite, the resin can change shade over time and may require frequent repair and maintenance.9,12
Metal alloy-porcelain implant supported prostheses, on the other hand, offer an esthetically pleasing prosthesis with high wear resistance. Unfortunately, porcelain chipping, difficulty in shade matching of pink porcelain and bimetallism are disadvantages of this type of prosthesis.12-18
Although the use of zirconia-ceramic prostheses have been reported veneer layer chipping and zirconia framework breakage as clinical complications, tetragonal zirconia polycrystal (TZP) displays high biocompatibility with reduced bacterial adhesion and high flexural strength which renders it as an excellent material for implant supported prosthesis.3,19-22 Using computer-aided design/computer-aided manufacturing (CAD/CAM) technology, it is possible to mill a monolithic prosthesis from presintered homogeneous blocks of TZP to overcome these problems.
This clinical report describes a reconstruction of the maxillary arch utilizing cement retained implant supported monolithic zirconia prosthesis. The occlusal surfaces and incisal edges of the prostheses were fabricated of monolithic zirconia (Prettau zirconia, Zirkonzahn GmbH, Gais, Italy) to minimize the possible fracture and chipping of layering porcelain. The protocol uses a CAD/CAM system to create a copy milled definitive prosthesis from an interim prosthesis. This significantly reduces the need for occlusal and gingival adjustments which may induce inadvertent damage to zirconia.
A 60 years old Caucasian female was referred to the postdoctoral prosthodontic clinic of the University of Alabama at Birmingham School of Dentistry for comprehensive dental care. The patient's medical history was noncontributory, and there were no contraindications for dental treatment. Although she reported radiation for breast cancer 5.5 years ago, she was cancer free at the time of treatment. Clinical and radiographic findings (Fig. 1) contributory to the definitive treatment were: debilitated dentition due to secondary caries under fixed partial denture (FPD) #3-11 with 4 to 8 mm probing depth around existing maxillary teeth, non-cleansable implant supported FPDs #12-14 and #29-31, the absence of keratinized tissue on the facial of implants #12-14, an uneven mandibular occlusal plane, class II amalgam restoration on #22 and 28 with a marginal gap discrepancy, noncarious cervical lesions on #24-26, probing depth ≥ 5 mm around #18 and 19 with class II furcation involvement on the facial #19, and class III furcation involvement and g rade III mobility on #18. Temporomandibular joint and mandibular range of motion were within normal limits and asymptomatic. To develop a treatment plan, diagnostic impressions were made with irreversible hydrocolid (Jeltrate Alginate, DENTSPLY International Inc., York, PA, USA), and centric relation was recorded using bimanual manipulation. An arbitrary hinge axis was used to transfer casts to a semiadjustable articulator (Whip Mix Corporation, Louisville, KY, USA). A diagnostic wax up was exercised on duplicated and cross mounted casts. Before the final treatment plan was initiated, the patient was seen at an emergency appointment and FPD #3-11 was were sectioned and teeth #3, 5 and 7 were extracted and socket grafted.
The patient was classified as a Class II Devision II malocclusion23 with low smile line. Based on the clinical and radiographic examination, the maxillary dentition was diagnosed as non-restorable. An uneven mandibular occlusal plane was diagnosed as a supraeruption in conjunction with a superiorly directed segmental alveolar growth at #23-27 area.24 Mandibular arch treatment options were: an orthodontic intrusion of the mandibular incisors, or restoring the occlusal plane with replacing full coverage restorations on the posterior teeth, fabricating veneers on the anterior teeth, and recontouring the incisal edges. Removable and fixed implant supported prostheses were reviewed as treatment options with the patient.
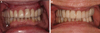
Based on the patient's request and the diagnostic findings, fixed implant supported prosthesis was selected for the reconstruction of the maxillary arch. However, the patient did not want orthodontic intrusion of the mandibular incisors, thus the combination prosthetic treatment was chosen for the mandibular arch. The decision was made to maintain teeth #6, 9, 10 and 11 temporarily as abutments for the interim prosthesis during surgical procedures. Pretreatment pictures were taken after the extraction teeth #3, 5 and 7 (Fig. 2A to 2D).
After elective root canal therapy on tooth #6, it was restored with a prefabricated fiber post (D.T. Ligh-Post, BISCO, Inc., Schaumburg, IL, USA) and composite resin core (Z100, 3M ESPE, St. Paul, MN, USA). After the restoration of the active caries, an interim FPD #5-11 was fabricated using a self polymerizing acrylic resin (Jet Acrylic, Lang Dental Manufacturing Co., Inc., IL, USA). Following the diagnostic wax up (Fig. 3), the decision was made to finalize the mandibular prosthetic treatment during the maxillary surgical procedures and the healing phase.
Extraction and socket conversion of #18 in conjunction with osseous surgery at the furcation of #19 were performed. During the surgical procedures and healing phase of the maxillary arch, the mandibular occlusal plane was restored with an implant supported FPD #29-31, full coverage crowns on #20 and 21, veneers on #22 and 27, a direct composite resin veneer on #28, and recontouring of the incisal edges of #23-26. At the end of the treatment, the patient requested veneers for #23 and 24 and a crown on #28 for esthetic improvement.
Surgical procedures for the maxillary arch included: soft tissue grafting at the buccal area of the implant supported FPD #12-14 with recontouring of the FPD for cleansability, sinus grafting of the maxillary right sinus, and 6 month later, implant placement of #3, 4 and 5 (Tapered Internal Hexed, BioHorizons, Birmingham, AL, USA). After the second stage of surgery on the posterior implants, teeth #6 and 11 were extracted with immediate placement of implants at the sites. After 6 months, the second stage of dental implant surgery was performed to uncover implants #6 and 11 in conjunction with extraction of teeth #9 and 10.
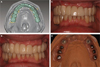
The maxillary arch was restored with three full arch maxillary interim prostheses during the surgical procedure. The first interim prosthesis was fabricated 6 months after healing of implants #3, 4 and 5. A tooth-implant supported interim prosthesis was fabricated which was screw retained on the existing osseointegrated maxillary implants and cement retained on tooth abutments #9 and 10. The interim prosthesis was fabricated by obtaining an impression of the exact location of the implants and abutting teeth using a maxillary custom tray (Triad TruTray, DENTSPLY International Inc., York, PA, USA), open tray implant posts (Direct Pick-up Coping, Hexed, BioHorizons, Birmingham, AL, USA), and polyvinylsiloxane impression material (Monophase Aquasil, DENTSPLY Caulk, Milford, DE, USA). The vertical dimension of occlusion (VDO), centric relation (CR), and facebow were transferred to a semiadjustable articulator (Whip Mix Corporation, Louisville, KY, USA) using an occlusal rim. The interim prosthesis was delivered immediately after extracting teeth #6 and 11 and placement of implants at these positions (Fig. 4A).
The second interim prosthesis was fabricated after the second stage of implant surgery on implants #6 and 11. During the second stage of surgery, teeth #9 and 10 were extracted. The interim prosthesis was fabricated using a direct technique following the diagnostic wax up (Fig. 4B). Titanium prefabricated abutments (3inOne Abutment, BioHorizons, Birmingham, AL, USA) were used as abutments on the implants. Self polymerizing acrylic resin (Jet Acrylic, Lang Dental Manufacturing Co., Inc., IL, USA) was used to fabricate the interim FPDs #3-5, #6-11 and #12-14 with a clear matrix formed from the diagnostic wax up. At the time of delivery, tissues at the #7 and 8 pontic areas were formed using a ball shaped diamond bur for an ovate shaped pontic.25,26 VDO was verified and the occlusion was adjusted at CR. The access openings on the titanium prefabricated abutments were covered with an interim restorative material (Telio CS Onlay, Ivoclar Vivadent Inc., Amherst, NY, USA) before the FPDs were cemented with temporary cement (Integrity TempGrip, DENTSPLY Caulk, Milford, DE, USA).
Two months after the second stage of implant surgery on # 6 and 11, the interim prosthesis was assessed for VDO, CR, phonetics, and esthetics. At this phase, the mandibular treatment was finalized and the occlusal plane on the mandible was established. Irreversible hydrocolloid impressions (Jeltrate Alginate, DENTSPLY International Inc., York, PA, USA) were made from the existing maxillary interim prosthesis and mandibular definitive restorations. The interocclusal records and facebow were recorded. An open tray, implant level, definitive impression was made with a silicone impression material (Aquasil, DENTSPLY Caulk, Milford, DE, USA) using a custom tray (Triad TruTray, DENTSPLY International Inc., York, PA, USA) and open tray titanium impression posts (Direct Pick-up Coping, Hexed, BioHorizons, Birmingham, AL, USA). VDO, CR were recorded with dental wax (ALUWAX, Aluwax Dental Products Co. Allendale, Michigan, USA) using healing abutments (Healing Abutment, BioHorizons, Birmingham, AL, USA) and segmented interim FPDs. Implant analogs (Implant Analog, BioHorizons, Birmingham, AL, USA) were placed on the impression posts and soft tissue was reproduced using polyvinylsiloxane (Gingival Mask HP, Henry Schien Inc. Melville, NY, USA). All impressions were poured with type III gypsum (Microstone, Whip Mix Corporation, Louisville, KY, USA). Casts were transferred and cross mounted on a semi-adjustable articulator (Whip Mix Corporation, Louisville, KY, USA) (Fig. 5A and 5B).
The accuracy of the maxillary definitive cast was verified with an interlocking jig. A vacuum formed clear matrix was made (Biostar, Great Lakes Orthodontics, Ltd. Tonawanda, NY, USA) from the maxillary cast duplicate from the cement retained interim prosthesis. A clear matrix and light polymerizing resin (Triad TruTray, DENTSPLY International Inc., York, PA, USA) were used to create a solid matrix for the fabrication of the custom abutments for the definitive cast (Fig. 5C). The solid matrix and the definitive cast were sent to a milling center (Astra Tech Inc. Waltham, MA, USA) for fabrication. Gold plated titanium abutments were used for the posterior implants and Zirconia abutments for implants #6 and 11. The milling center was asked to create the same path of insertion for the splinting abutments (Fig. 5D).
Upon delivery of the custom abutments, the definitive cast with custom abutments, the maxillary cast recorded from the existing interim prosthesis and mandibular cast were sent to a milling center (ZirkonZahn USA lab, Atlanta, GA, USA) where the assemblies were scanned for milling a new maxillary interim prosthesis. The maxillary cast duplicated from the interim prosthesis and the definitive cast with the custom abutments were superimposed for milling of the maxillary milled interim prosthesis (Fig. 6A). The milled interim prosthesis was milled from a resin blank (5-TEC A2, ZirkonZahn GmbH, Gais, Italy) to fit the custom abutments on the definitive cast.
Upon delivery of the interim prosthesis, the custom abutments were tightened to 30 Ncm and the milled interim prosthesis was evaluated intraorally for VDO, CR, esthetics, and phonetics. VDO was verified and the occlusion was adjusted at CR (Fig. 6B). Crowns and pontics #6-11 were modified for esthetics. Pontics #7-10 were modified for cleansability, esthetics, and phonetics. The modifications were made by sandblasting the milled interim prosthesis and with the addition of a self polymerizing acrylic resin (Lang Dental Manufacturing Co., Inc., Wheeling, IL, USA). Then, the interim prosthesis was polished and cemented with temporary cement (Integrity TempGrip, DENTSPLY Caulk, Milford, DE, USA) (Fig. 6C). The patient was asked to report any difficulties and returned to the clinic 2 weeks later.
When the patient was satisfied with the esthetic and functional parameters, the milled interim prosthesis and custom abutments were removed and the patient's previous interim FPDs were delivered. The intalgio surface of the pontics and embrasures of the milled interim prosthesis were recaptured on the definitive cast using polyvinylsiloxan (Gingival Mask HP, Henry Schien Inc., Melville, NY, USA) (Fig. 6D).
The definitive cast, custom abutments, and the milled interim prosthesis were returned to the milling center (Zirkonzahn USA lab, Atlanta, GA, USA). The milled interim prosthesis was scanned and copy milled (CAD/CAM System S-TEC, Zirkonzahn GmbH, Gais, Italy) from a presintered Zirconia blank (Prettau zirconia, Zirkonzahn GmbH, Gais, Italy, 22 mm in height). The final prosthesis was made into 3 FPDs, #3-5, #6-11 and #12-14. The labial surfaces of #6-11 were cut back for veneering porcelain. The milled frameworks were color modified as appropriate (Color liquid, Zirkonzahn GmbH, Gais, Italy), dried under an infrared lamp for an hour (Zirkonlamp 250, Zirkonzahn GmbH, Gais, Italy), and sintered at 1,600℃ (Sintering Furnace 600/V3, Zirkonzahn GmbH, Gais, Italy). The labial surfaces of #6-11 were laminate with veneering porcelain (ICE Ceramik, Zirkonzahn GmbH, Gais, Italy) and were fired at 820℃.
Upon delivery, the FPDs were adjusted at the embrasure as needed using a diamond disc (KOMET USA, Rock Hill, SC, USA) and under water spray. There was no need for occlusal adjustment. All adjusted areas were polished with porcelain polishing wheels (Brasseler USA, Savanah, GA, USA) and diamond filled polishing paste (Temrex Diamond, Temrex Corp. Freeport, NY, USA). The custom abutments were tightened to 30 Ncm twice at 10 minute intervals and screw accesses were covered with cotton pellets and interim restorative material (Telio CS Onlay, Ivoclar Vivadent Inc. Amherst, NY, USA) following manufacturer's instruction. The fit of the FPDs with the abutments were evaluated. A visual evaluation under ×2.5 magnifications and using an explorer showed a clinically acceptable fit. The fit was also verified with periapical radiographs. Then, the FPDs were cemented using a resin modified glass ionomer (RelyX Luting Plus, 3M ESPE, St. Paul, MN, USA) and the occlusion was verified again. At the follow up appointment the patient requested a crown on tooth #28 and porcelain veneers on #23 and 24 for esthetic improvement. The final restorations were documented in intraoral and extraoral photographs (Fig. 7A to 7F) and a panoramic radiograph (Fig. 8).
The post treatment instruction was given to the patient. This included twice per day brushing and flossing, and daily use of a mouthwash. The patient was monitored on 3-month recall appointments.
Despite technical advances, complex clinical situations require thorough treatment planning and multiple interim prostheses. The design of a definitive prosthesis must meet basic restorative requirements, such as function, phonetics, esthetics, and consideration of material properties.
Monolithic TZP provides a high standard of esthetics and reduces the number of metals used in the oral cavity. Additionally, when vertical and horizontal resorption of tissue requires pink esthetic replacement, pink colored zirconia can provide a stable and natural pink substructure to replace the lost tissue. This patient report presents an alternative method for the rehabilitation of a maxillary edentulous arch with a cement retained implant supported monolithic zirconia prosthesis. The patient was satisfied with the outcome of the treatment in terms of function, esthetics, and phonetics.
Mechanical properties such as young's modulous, flexural strength, and hardness of TZP has been reported to be higher than Ti alloy, stainless steel, Co-Cr alloy.27 It can be used on ceramic bridges, as long as the connector is appropriately designed to lower the maximum tensile stress applied on the connector.28,29 Additionally, the density of zirconia is about 6.1 g/cm3 which is 2 to 3 times lower than noble dental casting alloy. As a result, the final prosthesis fabricated from zirconia is lighter than the one made of metal alloy-porcelain.30 Ti alloy has a density of 4.5 g/cm3 which is lower than zirconia,30 but it has been reported that Ti alloy-acrylic prostheses require significant maintenance including the replacement of acrylic teeth and gingival architecture.1,2,6,7
Surface roughness (Ra) of the dental material has an important role in stain accumulation and adhesion/retention of bacteria. The rougher the surface, the more bacterial adherence occurs.31-35 While the surface roughness (Ra) value for acrylic resins range between 0.03 µm and 1.2 µm,36,37 glazed veneering porcelain ranges between 0.08 µm and 0.33 µm.38-43 Commercially pure Ti surface roughness (Ra) ranges between 0.008 µm and 0.02 µm,27 and the surface roughness of milled and processed TZP has been recorded to range between 0.08 µm and 0.1 µm.43,44 This indicates that TZP is a suitable prosthetic material in term of its capacity to reduce bacterial colonization.45,46 Surface roughness also directly impacts antagonist wear. Though, in vitro data has shown that TZP causes less wear on antagonist teeth as compared to feldspatic porcelain.43,47-49
Fracture of the veneering porcelain3,50 and fracture of the zirconia framework in cantilevered FPDs20,21 have been clinically reported in porcelain veneered zirconia prosthesis. In a literature review of 15 studies on zirconia prosthesis, Denry and Kelly50 found that fracture of zirconia framework was an uncommon phenomenon; however, chipping of the porcelain veneer was noted in all studies. In this patient report, the fabrication from a monolithic zirconia block decreases framework breakage due to the high thickness of connectors, and it reduces the probability of porcelain chipping.
Because of the advantages of monolithic zirconia, this treatment option may become more prevalent. Further research will be necessary comparing traditional metal alloy-ceramic versus monolithic zirconia in the rehabilitation of edentulous patients with fixed implant supported restorations. The combination of CAD/CAM technology and modern materials offer promising perspectives for future treatment options.
The major benefits of CAD/CAM milled monolithic zirconia prostheses are homogenous high strength, accuracy, elimination or reduced veneering porcelain, and minimal adjustments. This technology also offers different treatment options including screws, cement, and combination screw/cement retained prostheses to restore osseointegrated implants. Providing the milled interim prosthesis significantly reduces the need for occlusal adjustment in the final definitive prosthesis as the prosthesis is duplicated directly from the milled and adjusted interim prosthesis.
The outcome of the presented cement retained implant supported prosthesis was a success in terms of function, esthetics, and phonetics and the patient was highly satisfied. Although there have been numerous in vitro studies, there are few clinical reports supporting the use of monolithic TZP for definitive prostheses. Long term clinical studies will be required to further evaluate this material and technique for continued use in implant restorations.
Figures and Tables
 | Fig. 2A: Preoperative frontal view at maximum intercuspal position, B: Preoperative frontal view at protrusive movement, C: Preoperative maxillary occlusal view, D: Preoperative mandibular occlusal view. |
 | Fig. 4A: Implant-tooth retained interim prosthesis, two weeks after implant placement #6, 11, B: mplant retained interim prosthesis, two weeks after extraction of teeth #9 and 10. |
 | Fig. 5A: Maxillary interim prosthesis cast against mandibular definitive prosthesis cast, B: Maxillary definitive cast cross mounted on mandibular cast, C: Solid resin matrix on definitive cast, D: Zirconia and gold platted titanium custom abutments on definitive cast. |
 | Fig. 6A: Superimposed scan on definitive cast, B: Milled interim prosthesis before modification, C: Milled interim prosthesis after chair side modifications, D: Replicate of intaglio surface of the milled interim prosthesis on the definitive cast. |
References
1. Bergendal B, Palmqvist S. Laser-welded titanium frameworks for implant-supported fixed prostheses: a 5-year report. Int J Oral Maxillofac Implants. 1999; 14:69–71.
2. Bozini T, Petridis H, Garefis K, Garefis P. A meta-analysis of prosthodontic complication rates of implant-supported fixed dental prostheses in edentulous patients after an observation period of at least 5 years. Int J Oral Maxillofac Implants. 2011; 26:304–318.
3. Larsson C, Vult von Steyern P, Nilner K. A prospective study of implant-supported full-arch yttria-stabilized tetragonal zirconia polycrystal mandibular fixed dental prostheses: three-year results. Int J Prosthodont. 2010; 23:364–369.
4. Papaspyridakos P, Lal K. Complete arch implant rehabilitation using subtractive rapid prototyping and porcelain fused to zirconia prosthesis: a clinical report. J Prosthet Dent. 2008; 100:165–172.
5. Hassel AJ, Shahin R, Kreuter A, Rammelsberg P. Rehabilitation of an edentulous mandible with an implant-supported fixed prosthesis using an all-ceramic framework: a case report. Quintessence Int. 2008; 39:421–426.
6. Ghazal M, Hedderich J, Kern M. Wear of feldspathic ceramic, nano-filled composite resin and acrylic resin artificial teeth when opposed to different antagonists. Eur J Oral Sci. 2008; 116:585–592.
7. Jemt T. Failures and complications in 391 consecutively inserted fixed prostheses supported by Brånemark implants in edentulous jaws: a study of treatment from the time of prosthesis placement to the first annual checkup. Int J Oral Maxillofac Implants. 1991; 6:270–276.
8. Suzuki S. In vitro wear of nano-composite denture teeth. J Prosthodont. 2004; 13:238–243.
9. Coachman C, Salama M, Garber D, Calamita M, Salama H, Cabral G. Prosthetic gingival reconstruction in fixed partial restorations. Part 3: laboratory procedures and maintenance. Int J Periodontics Restorative Dent. 2010; 30:19–29.
10. Bencharit S, Schardt-Sacco D, Border MB, Barbaro CP. Full mouth rehabilitation with implant-supported prostheses for severe periodontitis: a case report. Open Dent J. 2010; 4:165–171.
11. Hagiwara Y, Nakajima K, Tsuge T, McGlumphy EA. The use of customized implant frameworks with gingiva-colored composite resin to restore deficient gingival architecture. J Prosthet Dent. 2007; 97:112–117.
12. Alani A, Maglad A, Nohl F. The prosthetic management of gingival aesthetics. Br Dent J. 2011; 210:63–69.
13. Linkevicius T, Vladimirovas E, Grybauskas S, Puisys A, Rutkunas V. Veneer fracture in implant-supported metal-ceramic restorations. Part I: Overall success rate and impact of occlusal guidance. Stomatologija. 2008; 10:133–139.
14. Roberts DH. The failure of retainers in bridge prostheses. An analysis of 2,000 retainers. Br Dent J. 1970; 128:117–124.
15. Jacobi R, Shillingburg HT Jr, Duncanson MG Jr. Effect of abutment mobility, site, and angle of impact on retention of fixed partial dentures. J Prosthet Dent. 1985; 54:178–183.
16. Reuter JE, Brose MO. Failures in full crown retained dental bridges. Br Dent J. 1984; 157:61–63.
17. Llobell A, Nicholls JI, Kois JC, Daly CH. Fatigue life of porcelain repair systems. Int J Prosthodont. 1992; 5:205–213.
18. Ehrenkranz H, Langer B, Marotta L. Complete-arch maxillary rehabilitation using a custom-designed and manufactured titanium framework: a clinical report. J Prosthet Dent. 2008; 99:8–13.
19. Stefan H, Michael B, Enrico S, Markus BB, Manfred W. The Application of Zirconium Oxide Frameworks for Implant Superstructures. Quintessence Dent Tech. 2006; 29:103–112.
20. Ohlmann B, Marienburg K, Gabbert O, Hassel A, Gilde H, Rammelsberg P. Fracture-load values of all-ceramic cantilevered FPDs with different framework designs. Int J Prosthodont. 2009; 22:49–52.
21. Al-Amleh B, Lyons K, Swain M. Clinical trials in zirconia: a systematic review. J Oral Rehabil. 2010; 37:641–652.
22. Heintze SD, Rousson V. Survival of zirconia- and metal-supported fixed dental prostheses: a systematic review. Int J Prosthodont. 2010; 23:493–502.
23. Angle EH. Classification of malocclusion. Dental Cosmos. 1899; 41:248–264.
24. Kaplan P. Drifting, tipping, supraeruption, and segmental alveolar bone growth. J Prosthet Dent. 1985; 54:280–283.
25. Del Castillo R, Ercoli C, Delgado JC, Alcaraz J. An alternative multiple pontic design for a fixed implant-supported prosthesis. J Prosthet Dent. 2011; 106:198–203.
26. Edelhoff D, Spiekermann H, Yildirim M. A review of esthetic pontic design options. Quintessence Int. 2002; 33:736–746.
27. Piconi C, Maccauro G. Zirconia as a ceramic biomaterial. Biomaterials. 1999; 20:1–25.
28. Studart AR, Filser F, Kocher P, Gauckler LJ. Fatigue of zirconia under cyclic loading in water and its implications for the design of dental bridges. Dent Mater. 2007; 23:106–114.
29. Lüthy H, Filser F, Loeffel O, Schumacher M, Gauckler LJ, Hammerle CH. Strength and reliability of four-unit all-ceramic posterior bridges. Dent Mater. 2005; 21:930–937.
30. Ronald LS, John MP. Evolve resources for Craig's restorative dental materials. 12th ed. Mosby;2006.
31. Quirynen M, Bollen CM, Willems G, van Steenberghe D. Comparison of surface characteristics of six commercially pure titanium abutments. Int J Oral Maxillofac Implants. 1994; 9:71–76.
32. Teughels W, Van Assche N, Sliepen I, Quirynen M. Effect of material characteristics and/or surface topography on biofilm development. Clin Oral Implants Res. 2006; 17:68–81.
33. Bollen CM, Lambrechts P, Quirynen M. Comparison of surface roughness of oral hard materials to the threshold surface roughness for bacterial plaque retention: a review of the literature. Dent Mater. 1997; 13:258–269.
34. Sardin S, Morrier JJ, Benay G, Barsotti O. In vitro streptococcal adherence on prosthetic and implant materials. Interactions with physicochemical surface properties. J Oral Rehabil. 2004; 31:140–148.
35. Johannsen G, Redmalm G, Rydén H. Surface changes on dental materials. II. The influence of two different dentifrices on surface roughness measured by laser reflexion and profilometer techniques. Swed Dent J. 1992; 16:13–20.
36. Busscher HJ, van Pelt AWJ, de Boer P, de Jong HP, Arends J. The effect of surface roughening of polymers on measured contact angles of liquids. Colloid Surf. 1984; 9:319–331.
37. Heath JR, Wilson HJ. Surface roughness of restorations. Br Dent J. 1976; 140:131–137.
38. Rosenstiel SF, Baiker MA, Johnston WM. Comparison of glazed and polished dental porcelain. Int J Prosthodont. 1989; 2:524–529.
39. Ward MT, Tate WH, Powers JM. Surface roughness of opalescent porcelains after polishing. Oper Dent. 1995; 20:106–110.
40. Al-Wahadni A. An in vitro investigation into the surface roughness of 2 glazed, unglazed, and refinished ceramic materials. Quintessence Int. 2006; 37:311–317.
41. Klausner LH, Cartwright CB, Charbeneau GT. Polished versus autoglazed porcelain surfaces. J Prosthet Dent. 1982; 47:157–162.
42. Sasahara RM, Ribeiro Fda C, Cesar PF, Yoshimura HN. Influence of the finishing technique on surface roughness of dental porcelains with different microstructures. Oper Dent. 2006; 31:577–583.
43. Rosentritt M, Preis V, Behr M, Hahnel S, Handel G, Kolbeck C. Two-body wear of dental porcelain and substructure oxide ceramics. Clin Oral Investig. 2012; 16:935–943.
44. Vigolo P, Motterle M. An in vitro evaluation of zirconia surface roughness caused by different scaling methods. J Prosthet Dent. 2010; 103:283–287.
45. Rimondini L, Cerroni L, Carrassi A, Torricelli P. Bacterial colonization of zirconia ceramic surfaces: an in vitro and in vivo study. Int J Oral Maxillofac Implants. 2002; 17:793–798.
46. Scarano A, Piattelli M, Caputi S, Favero GA, Piattelli A. Bacterial adhesion on commercially pure titanium and zirconium oxide disks: an in vivo human study. J Periodontol. 2004; 75:292–296.
47. Jung YS, Lee JW, Choi YJ, Ahn JS, Shin SW, Huh JB. A study on the in-vitro wear of the natural tooth structure by opposing zirconia or dental porcelain. J Adv Prosthodont. 2010; 2:111–115.
48. Preis V, Behr M, Handel G, Schneider-Feyrer S, Hahnel S, Rosentritt M. Wear performance of dental ceramics after grinding and polishing treatments. J Mech Behav Biomed Mater. 2012; 10:13–22.
49. Preis V, Behr M, Kolbeck C, Hahnel S, Handel G, Rosentritt M. Wear performance of substructure ceramics and veneering porcelains. Dent Mater. 2011; 27:796–804.
50. Denry I, Kelly JR. State of the art of zirconia for dental applications. Dent Mater. 2008; 24:299–307.




 PDF
PDF ePub
ePub Citation
Citation Print
Print






 XML Download
XML Download