Abstract
PURPOSE
The purpose of this study was to investigate the effect of resin cements and primer on the retentive force of zirconia copings bonded to zirconia abutments with insufficient retention.
MATERIALS AND METHODS
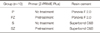
Zirconia blocks (Lava, 3M ESPE, St. Paul, MN, USA) were obtained and forty sets of zirconia abutments and copings were fabricated using CAD/CAM technology. They were grouped into 4 categories as follows, depending on the types of resin cements used, and whether the primer is applied or not:Panavia F2.0 (P), Panavia F2.0 using Primer (PRIME Plus, Bisco Inc, Schaumburg, IL, USA) (PZ), Superbond C&B (S), and Superbond C&B using Primer (SZ). For each of the groups, the cementation was conducted. The specimens were kept in sterilized water (37℃) for 24 hours. Retentive forces were tested and measured, and a statistical analysis was carried out. The nature of failure was recorded.
RESULTS
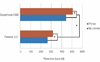
The means and standard deviations of retentive force in Newton for each group were 265.15 ± 35.04 N (P), 318.21 ± 22.24 N (PZ), 445.13 ± 78.54 N (S) and 508.21 ± 79.48 N (SZ). Superbond C&B groups (S & SZ) showed significantly higher retentive force than Panavia F2.0 groups (P & PZ). In Panavia F2.0 groups, the use of primer was found to contribute to the increase of retentive force. On the other hand, in Superbond C&B groups, the use of primer did not influence the retention forces. Adhesive failure was observed in all groups.
Prosthetic restoration by using maxillary anterior implants is becoming more popular as implant treatments become more common. All-ceramic crowns are used more often than metal crowns in maxillary anterior implants to enhance esthetic effects.1,2 The materials used in all-ceramic crowns can be broadly classified into silica-based (feldspathic porcelains, leucite-reinforced ceramics, lithium disilicate ceramics) and nonsilica-based (zirconia or Y-TZP, alumina). Of these, zirconia is characterized by its high flexibility, high fracture toughness, biocompatibility and excellent esthetics.3,4 Due to these advantages and the introduction of CAD/CAM technology, zirconia is increasingly used in prosthetic restorations. Zirconia abutments enhance the esthetic effect, especially in the case of maxillary anterior implants, since they do not allow metal to be shown.5
On the other hand, the bonding strength of zirconia is weaker than that of other dental ceramics, so various mechanical and chemical surface treatment methods have been investigated to increase it. In terms of mechanical surface treatment, sandblasting with alumina increases bonding strength.6 However, other reports claim that such treatments can weaken the material's physical properties and cause cracks.7,8 The use of a tribochemical silica coating inside the prosthesis as a mechanochemical method has been reported to increase the bonding strength for overlong periods.9 However, the simultaneous application of sandblasting and tribochemical silica coating treatments in zirconia abutments and within the zirconia in clinical practice is inconvenient. Furthermore, the application process can damage both the gingival tissues and the body of the implant.
A few studies have stated that the use of primer or resin cements containing 4-methacryloyloxyethyl trimellitate anhydride (4-META) or 10-methacryloxydecyldihydrogen-phosphate (MDP) monomer as chemical bonding methods affords a higher bond strength since it enables chemical bonding with zirconia.3,10,11 These methods are more convenient in clinical practice than the previously mentioned methods and have the advantage of not damaging the implant surface.
Meanwhile, it is often difficult to secure the ideal prosthesis implant angle in the anterior region of the maxilla after tooth extraction due to buccal bone resorption. The use of angled abutments and cement-retained prostheses are preferred for this reason. However, the use of angled abutments is thought to create greater angles and retentiveness because the palatal side of the abutment must be removed to secure the space between the buccal abutment screw and the antagonist tooth. A previous study experimented with the impact on retentive force after differentiating the removal of screw entry lining at the rate of 1/3 to the titanium abutment with 15° of abutment angle and blocking the screw entry partially or entirely. The investigators noted a significant impact on the retentive force.12 In this study, additional palatal removal was performed to simulate a more feasible clinical practice procedure.
This study aimed to examine the effects of resin cements and primers containing special functional materials on the retentive force by using maxillary anterior experiment models with zirconia abutments and zirconia copings that are expected to have less retentiveness.
Table 1 lists the materials used in this study. Zirconia (Lava, 3M ESPE, St. Paul, MN, USA) was used as a sample and the resin cement containing MDP (Panavia F 2.0 Kuraray Medical Inc., Okayama, Japan) and that containing 4-META (Superbond C&B SunMedical, Moriyama, Japan) were used. Surface treatments were performed using the primer comprising organophosphate and carboxylic acid monomer (Z-PRIME Plus Bisco Inc., Schaumburg, IL, USA).
Zirconia block (Lava 3M ESPE) was fabricated using CAD/CAM to create 40 zirconia abutments and 40 zirconia copings with the following specifications: 17° angle entry for the buccal side screw, 4.0 mm diameter 0.6 mm marginal thickness and 5 mm height abutment made by drilling from the palatal side. The base was added for the bottom part of an Instron 3366 (Instron Corp, Canton, MA, USA) to make an all-in-one system. The zirconia copings were fabricated to match each abutment and a hole was made on the upper part of the occlusal surface of each coping to allow it to be pulled by a wire from the upper part of the Instron (Fig. 1).
The 40 zirconia abutments and copings were classified into 4 groups according to resin cement type and primer use. Table 2 shows the experimental groups.
The 40 zirconia abutments and 40 zirconia copings were ultrasonically cleaned for 3 min and dried in a compressed air system after marginal adaptability testing. The groups with the primer (Z-PRIME Plus Bisco Inc.) were dried for 5 seconds in a compressed air system as instructed by the manufacturer. Finger pressure was then applied to cement the sample and any excessive cement was removed in the usual manner as instructed by the manufacturer.
All of the samples were stored in normal saline at 37℃ for 24 hours once they were polymerized.
The upper portion of the samples cohered to the Instron 3366 universal testing machine was fixed to the upper jig with wires, while the bottom portion of the sample was fixed vertical (Fig. 2). The upper jig was run at 1.0 mm/min crosshead speed until failure and the N value (Newtons) was recorded.
The fracture failure modes were evaluated by observing the zirconia copings that failed to adhere to the zirconia surface before and after primer application.
A paired t-test was used for the comparison according to primer application status for each resin cement, while an independent t-test was used to compare the individual resin cements. Statistical significance was set at P≤.05.
The mean ± SD retentive force in Newton for each group was 265.15 ± 35.04 N (P), 318.21 ± 22.24 N (PZ), 445.13 ± 78.54 N (S), 508.21 ± 79.48 N (SZ). Fig. 3 shows the evaluation of the primer application and individual cement. There was a significant difference in retentive force when primer was used with Panavia F 2.0 (P=.007) but no significant difference in retentive force when primer was used with Superbond C&B, according to the paired t-tests.
Moreover, independent t-tests showed that Superbond C&B group had significantly higher retentive forces than Panavia Panavia F 2.0 (P<.001).
Fig. 4 shows the surface of the zirconia before and after primer application. A relatively even film formation is visible on the zirconia surface after use of the primer. All of the fracture failure modes demonstrated adhesive failure (Fig. 5). Some of cement remained in 1/3 of the cervical area of the zirconia abutments, while the rest remained within the zirconia copings.
The use of all-ceramic prostheses with zirconia copings is becoming increasingly popular owing to the several advantages of zirconia. However, the adhesive bonding ability of zirconia is significantly lower than that of other dental ceramics. Silica-based ceramics are usually processed with hydrofluoric acid gel (FH) and silanization treatment, but zirconia cannot be treated with hydrofluoric acid because it is a non-silica-based ceramic.11,13
In clinical practice, ceramic primer is applied after sandblasting zirconia ceramics with 50 µm of alumina or silane primer is applied after tribochemical silica coating is applied inside the prosthesis to achieve higher zirconia ceramicbond strength. These methods are safe to use inside the prosthesis as long as the teeth themselves act as abutments, but zirconia abutments can be damaged in the process.
For this reason, chemical methods using resin cements and primer were tested in the current study in an effort to achieve higher bond strength. A number of studies have been conducted to increase the bond strength of resin cement, while Bis-GMA, MDP monomer, and 4-META are commonly used to cement zirconia. Of these, Bis-GMA resin cement has lower bond strength,14 and it has been reported that the bonding strength decreases even further after treatment within a thermal cycling system.6,11
In recent years, it has been acknowledged that resin cements containing MDP monomer used with sandblasting have excellent bond strength15,16 this is thought to be a result of the interaction between the hydroxyl group (OH) of the MDP monomer and the hydroxyl group of the zirconia surface.17 Some studies have reported that this method is also effective over the long term.3,6,11 One of these studies experimented with tensile bonding strength and reported that the phosphate of MDP chemically bound with the zirconia.18 Based on these results and considering long-term safety, the use of resin cements containing the MDP monomer is recommended to maximize zirconia adhesion.
On the other hand, a number of researchers have also reported that Superbond C&B, the resin cement containing 4-META (an acidic monomer), has higher bond strength than resin cements containing the MDP monomer.10,19,20 These studies suggested that the anhydride of the4-META was strongly bound to zirconia because Superbond C&B did not contain a filler that enabled good flow but that the4-META facilitated monomer diffusion and had high bond strength.21 No definite evidence supports this strong chemical binding.
Metal primers are sometimes used with other metallic materials along with resin cement to produce the same effect. In a study, metal and ceramic primers were applied and cemented with RelyX Unicem (3M, ESPE, St. Paul, MN, USA) to zirconia and stored in water for 180 days, and the results showed that only the bond strengths of the samples that used metal primer were not significantly reduced.22 The primer used in this study, Z-PRME Plus, contains an organophosphate and a carboxylic acid monomer. One study of the effects of this primer on the shear bond strength of zirconia and resin cement showed that samples treated with primer had significantly higher shear bond strength than those treated with sandblasting only, and it was thought that the phosphates were bound to the oxides on the zirconia surface.23
On the basis of this evidence, Panavia F 2.0, the resin cement containing MDP, and Superbond C&B, the resin cement with the stronger bond strength and containing 4-META, were investigated. The maxillary anterior zirconia implant, which was expected to have less retentiveness, was chosen in this study to evaluate the retentiveness of all ceramic angle abutments and copings. Furthermore, the retentiveness of more feasible primer types in clinical practice was also evaluated for challenging cases such as applying sandblasting or silica coating to zirconia abutments. The results showed that the retentive force was significantly increased after the use of resin cements or primers containing MDP (P=.007). This result supports those of earlier studies claiming that the use of primers increased the shear bond strength.24 In addition, primer use did not significantly increase the retentive force of Superbond C&B containing 4-META (P=.191), but it did increase the retentive force of Panavia F 2.0 (P<.001) compared to earlier research results.10,19,20
The retentive forces of cements are generally affected by axial angles, surface areas, abutment heights, surface roughness, and cement type.25-29 Moreover, the retentive forces of implant prostheses can differ from those of natural teeth.28-30 It has also been reported that internal thickness also significantly affects the retentiveness of zirconia copings and titanium abutments.31 In this study, other factors were standardized to examine the effects of the different cements and primers on retentive force. However, in reality, the internal thicknesses of the zirconia abutments and zirconia copings were not even, which might have affected the experimental results.
Furthermore, long-term safety was not determined in this study. The study conducted thermal cycling treatment (×10,000) of different resin cement types on zirconia, including Superbond C&B and Panavia, and showed that Pavavia 21 had significantly higher shear bond strength than Superbond C&B (P<.05).14 In the same experiment, the shear bond strength of Superbond C&B was significantly reduced after the thermal cycling treatment. The finger pressure method without standard equipment was also expected to increase the standard deviation. Therefore, further studies with better control over these factors will be required in the future.
Standard zirconia surface treatments to obtain secure bond strength have not yet been established.32,33 Moreover, most studies of the cementation of zirconia and resin cements focus on shear bond strength and tensile bond strength. As such, further research involving pull-out tests with well-controlled influential factors in a delicately simulated oral environment will be required. Research to identify the influential factors affecting long-term durability and actual clinical research should also be conducted more actively.
The application of Z PRIME Plus increased the retentive force of Panavial F2.0 containing MDP (P=.007) significantly, and increased the retentive force of Superbond C&B containing 4-META, but the difference was not statistically significant. The retentive force of Superbond C&B was significantly higher than Panavia F2.0 with or without the use of Z PRIME Plus (P<.05). All of the experiment samples showed adhesive failure.
References
1. Anusavice KJ. Recent developments in restorative dental ceramics. J Am Dent Assoc. 1993; 124:72–74. 76–78. 80–84.
2. Kelly JR, Nishimura I, Campbell SD. Ceramics in dentistry: historical roots and current perspectives. J Prosthet Dent. 1996; 75:18–32.
3. Blatz MB, Chiche G, Holst S, Sadan A. Influence of surface treatment and simulated aging on bond strengths of luting agents to zirconia. Quintessence Int. 2007; 38:745–753.
4. Luthardt RG, Holzhüter M, Sandkuhl O, Herold V, Schnapp JD, Kuhlisch E, Walter M. Reliability and properties of ground Y-TZP-zirconia ceramics. J Dent Res. 2002; 81:487–491.
5. Yildirim M, Edelhoff D, Hanisch O, Spiekermann H. Ceramic abutments-a new era in achieving optimal esthetics in implant dentistry. Int J Periodontics Restorative Dent. 2000; 20:81–91.
6. Ozcan M, Vallittu PK. Effect of surface conditioning methods on the bond strength of luting cement to ceramics. Dent Mater. 2003; 19:725–731.
7. Zhang Y, Lawn BR, Malament KA, Van Thompson P, Rekow ED. Damage accumulation and fatigue life of particle-abraded ceramics. Int J Prosthodont. 2006; 19:442–448.
8. Zhang Y, Lawn BR, Rekow ED, Thompson VP. Effect of sandblasting on the long-term performance of dental ceramics. J Biomed Mater Res B Appl Biomater. 2004; 71:381–386.
9. Bottino MA, Valandro LF, Scotti R, Buso L. Effect of surface treatments on the resin bond to zirconium-based ceramic. Int J Prosthodont. 2005; 18:60–65.
10. Dérand P, Dérand T. Bond strength of luting cements to zirconium oxide ceramics. Int J Prosthodont. 2000; 13:131–135.
11. Kern M, Wegner SM. Bonding to zirconia ceramic: adhesion methods and their durability. Dent Mater. 1998; 14:64–71.
12. Emms M, Tredwin CJ, Setchell DJ, Moles DR. The effects of abutment wall height, platform size, and screw access channel filling method on resistance to dislodgement of cement-retained, implant-supported restorations. J Prosthodont. 2007; 16:3–9.
13. Janda R, Roulet JF, Wulf M, Tiller HJ. A new adhesive technology for all-ceramics. Dent Mater. 2003; 19:567–573.
14. Lüthy H, Loeffel O, Hammerle CH. Effect of thermocycling on bond strength of luting cements to zirconia ceramic. Dent Mater. 2006; 22:195–200.
15. Blatz MB, Sadan A, Martin J, Lang B. In vitro evaluation of shear bond strengths of resin to densely-sintered high-purity zirconium-oxide ceramic after long-term storage and thermal cycling. J Prosthet Dent. 2004; 91:356–362.
16. Atsu SS, Kilicarslan MA, Kucukesmen HC, Aka PS. Effect of zirconium-oxide ceramic surface treatments on the bond strength to adhesive resin. J Prosthet Dent. 2006; 95:430–436.
17. Ozcan M, Nijhuis H, Valandro LF. Effect of various surface conditioning methods on the adhesion of dual-cure resin cement with MDP functional monomer to zirconia after thermal aging. Dent Mater J. 2008; 27:99–104.
18. Wegner SM, Kern M. Long-term resin bond strength to zirconia ceramic. J Adhes Dent. 2000; 2:139–147.
19. Ernst CP, Cohnen U, Stender E, Willershausen B. In vitro retentive strength of zirconium oxide ceramic crowns using different luting agents. J Prosthet Dent. 2005; 93:551–558.
20. Lee HJ, Ryu JJ, Shin SW, Suh KW. Effect of surface treatment methods on the shear bond strength of resin cement to zirconia ceramic. J Korean Acad Prosthodont. 2007; 45:743–752.
21. Kim CH, Jeon YC, Jeong CM, Lim JS. Effect of surface treatments of zirconia ceramic on the bond strength of resin cements. J Korean Acad Prosthodont. 2004; 42:386–396.
22. Lindgren J, Smeds J, Sjögren G. Effect of surface treatments and aging in water on bond strength to zirconia. Oper Dent. 2008; 33:675–681.
23. Lee JH, Kim HS, Pae AR, Woo YH. Influence of sandblasting and primer on shear bond strength of resin cement to zirconia. J Korean Acad Prosthodont. 2011; 49:49–56.
24. Magne P, Paranhos MP, Burnett LH Jr. New zirconia primer improves bond strength of resin-based cements. Dent Mater. 2010; 26:345–352.
25. Michalakis KX, Hirayama H, Garefis PD. Cement-retained versus screw-retained implant restorations: a critical review. Int J Oral Maxillofac Implants. 2003; 18:719–728.
26. Abbo B, Razzoog ME, Vivas J, Sierraalta M. Resistance to dislodgement of zirconia copings cemented onto titanium abutments of different heights. J Prosthet Dent. 2008; 99:25–29.
27. Ramp MH, Dixon DL, Ramp LC, Breeding LC, Barber LL. Tensile bond strengths of provisional luting agents used with an implant system. J Prosthet Dent. 1999; 81:510–514.
28. Covey DA, Kent DK, St Germain HA Jr, Koka S. Effects of abutment size and luting cement type on the uniaxial retention force of implant-supported crowns. J Prosthet Dent. 2000; 83:344–348.
29. Squier RS, Agar JR, Duncan JP, Taylor TD. Retentiveness of dental cements used with metallic implant components. Int J Oral Maxillofac Implants. 2001; 16:793–798.
30. Mansour A, Ercoli C, Graser G, Tallents R, Moss M. Comparative evaluation of casting retention using the ITI solid abutment with six cements. Clin Oral Implants Res. 2002; 13:343–348.
31. Ebert A, Hedderich J, Kern M. Retention of zirconia ceramic copings bonded to titanium abutments. Int J Oral Maxillofac Implants. 2007; 22:921–927.
32. Thompson JY, Stoner BR, Piascik JR, Smith R. Adhesion/cementation to zirconia and other non-silicate ceramics: where are we now? Dent Mater. 2011; 27:71–82.
33. Behr M, Proff P, Kolbeck C, Langrieger S, Kunze J, Handel G, Rosentritt M. The bond strength of the resin-to-zirconia interface using different bonding concepts. J Mech Behav Biomed Mater. 2011; 4:2–8.




 PDF
PDF ePub
ePub Citation
Citation Print
Print







 XML Download
XML Download