Abstract
PURPOSE
Adequate passive-fitting of one-piece cast 3-element implant-supported frameworks is hard to achieve. This short communication aims to present an alternative method for section of one-piece cast frameworks and for casting implant-supported frameworks.
MATERIALS AND METHODS
Three-unit implant-supported nickel-chromium (Ni-Cr) frameworks were tested for vertical misfit (n = 6). The frameworks were cast as one-piece (Group A) and later transversally sectioned through a diagonal axis (Group B) and compared to frameworks that were cast diagonally separated (Group C). All separated frameworks were laser welded. Only one side of the frameworks was screwed.
RESULTS
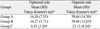
The results on the tightened side were significantly lower in Group C (6.43 ± 3.24 µm) when compared to Groups A (16.50 ± 7.55 µm) and B (16.27 ± 1.71 µm) (P<.05). On the opposite side, the diagonal section of the one-piece castings for laser welding showed significant improvement in the levels of misfit of the frameworks (Group A, 58.66±14.30 µm; Group B, 39.48±12.03 µm; Group C, 23.13±8.24 µm) (P<.05).
Complete passive fitting of one-piece cast implant supported frameworks has been hard to achieve according to reports from the last three decades.1 In addition to load bearing capacity, marginal accuracy and clinically acceptable levels of misfit are crucial factors influencing the clinical long-term reliability of fixed partial dentures (FPDs).2 Misfit levels of up to 100 µm were once stated as clinically acceptable.3 Laser welding has been used to correct ill-fitting implant-supported frameworks4 and may decrease the strains transferred to the implant-bone interface.5 Previous studies found that laser welding of implant-supported frameworks is capable of reducing the prosthetic misfit.4,6-8 The diagonal section of one-piece castings for laser welding reduces the misfit levels of implant-supported frameworks.9,10 Laser welding is also able to concentrate the laser energy near the welded surface, thus minimizing distortion of heat-sensitive materials.11
This study aims to evaluate the vertical misfit of three-unit implant-supported frameworks, cast as one-piece and later sectioned in its diagonal axis in the attempt to lower the misfit levels of the one-piece cast frameworks compared to cast diagonally separated.10 The tested null hypothesis was that no differences would be found between casting one-piece frameworks and sectioning the one-piece cast frameworks for laser welding. The misfit levels found for the frameworks that were cast diagonally separated were used as a parameter for the improvement in the levels of misfit for the first two groups.
This study followed previously described methodology4,12 and used a machined metal matrix with two internal hex cylinder threaded implants embedded parallel to each other (ø3.75 mm × 11 mm, Titamax II Plus, Neodent, Curitiba, PR, Brazil). Prosthetic abutments (Mini conical abutments II Plus, Neodent, Curitiba, PR, Brazil) were screwed to each implant and tightened to 20 Ncm.12 All specimens were made using the aforementioned model, which also served as an index for measuring the accuracy of the casting and soldering procedures.
Plastic cylinders (Mini conical abutment cylinder, Neodent, Curitiba, PR, Brazil) were screw-retained to each implant and the cylinders were bonded using acrylic resin (Pattern Resin LS, GC America Inc., Costa Mesa, CA, USA). A 3-unit implant-supported FPD framework was then waxed. The first waxed framework was used as a pattern for the two groups that were formed (n = 6) and cast in Ni-Cr alloy (VeraBond II, Aalba Dent. Inc., Cordelia, CA, USA). Group A was formed by one-piece castings (control group); Group B used one-piece castings from Group A that were later transversely sectioned in a diagonal direction in the pontic area9; and Group C, with the waxed frameworks transversely sectioned (0.3 mm apart) with surgical blades in a diagonal direction in the pontic area before casting10 (Fig. 1). One-piece frameworks from group A were sectioned in the pontic with a 0.18 mm thick diamond disk (Diamond disk #940, Komet USA, Rock Hill, SC, USA) (Groups B). The two parts of each framework from groups B and C were laser-welded (Fig. 2) (Desktop Laser, Dentaurum, Ispringen, Germany) according to settings of previous study (300 V, pulse duration of 9.0 ms and welding spot diameter of 0.78 mm).10
Specimens were tested for passive fit by tightening the screws to 10 Ncm.12 The first measurement of the misfit levels between the implant abutment and the FPD framework was made with one screw tightened. The reading was made on both tightened and opposite sides. The screw location was changed for the second reading.4,12 Three measurements were performed in an optical microscope (Nikon Corp., Tokyo, Japan) at 15× magnification at buccal, lingual, and proximal aspects, totalizing 12 points for each cylinder/condition 12 so as to sample all proximal aspects of the cylinder circle.
After all reading procedures, the specimens were coronally sectioned and submitted to scanning electron microscopy (SEM) to check the quality of the diagonal welding technique.
ANOVA was applied for one criteria (frameworks' separation) and the Tukey-Kramer test was used for the comparisons between the groups (P<.05) when significant differences were found (JMP 6.0, SAS Institute, Cary, NC, USA).
Table 1 and Fig. 3 present means, standard deviations and Tukey-Kramer's test results found in this study. With one screw tightened and on the tightened side, Group C showed significantly better results (P<.05). On the opposite side, laser welded Groups B and C, when compared to Group A, showed significantly better passive fitting (P<.05).
Coronally sectioning the diagonally welded frameworks and submitting to SEM at 50× magnification found a sufficiently welded surface (Fig. 4).
This study found that casting frameworks separately using a diagonal section, presented lower misfit values among groups, though it was not statistically significant in some cases. Diagonally sectioning one-piece cast frameworks can promote better fitting results. Complete passivity however cannot be reported. This finding is consistent with the results found in previous studies examining the lack of complete passivity with frameworks, as seen in the results showed in the one-screw test.4,12
This study focused in the experimental diagonal section for framework casting and for sectioning one-piece castings for laser welding. The groups were divided aiming to compare whether the misfit found for the one-piece castings could be corrected using the diagonal section. Also, a group cast with the diagonal section was formed (Group C) so as to provide information whether it would be better to cast diagonally sectioned frameworks and whether the diagonal section could be used to improve the passive fitting of one-piece castings.
The need for a lesser amount of material added to the welded region for laser welding reduces the volume of metal that is going to suffer from cooling contraction, thus leading to less distortions of the welded frameworks.10 The diagonal section of the implant-supported frameworks is expected to provide a better overlap between the sectioned regions; this feature could allow for an easier welding procedure, contributing for the reduction of molten alloy between the welded surfaces. For conventional dental soldering, the parent alloys are soldered with different types of alloy solder, thus reducing the strength of the soldered joints and accounting for the failure at the joints of soldered restorations.13 A significant lower misfit level for the welded frameworks was found in the analysis of data from the opposite side to the tightened side. Earlier studies found varying misfit from 10 to 160 µm,4,14,15 thus validating the casting and sectioning procedures used in this study. The levels of misfit that were found in this study were within clinically acceptable ranges (under 100 µm).16
The diagonal section of the frameworks allowed for a smaller joint thickness than that occurring in conventional transversal welding, minimizing horizontal and vertical distortions in the framework position.9 These results are in accordance with another previously published study.10 In a study using two different joint types,17 beveled-edged specimens presented smaller deformation than square-edged surfaces. Laser irradiation also reached deeper penetration in the beveled-edged specimens.17 It has been suggested that the 'I' design (perpendicularly to the long axis) or transversal section of joints is not the best section for large diameters, because of the limited power supply of the dental welding machines.18 Conversely, the 'X' design,19 may lead to better laser-welded joints. In such design, the center is maintained juxtaposed to the sections with thin diameters, permitting deep laser-beam penetration.
Some distortion of the implant-supported frameworks may occur after the firing cycles required for porcelain application. Some studies have found that the contributing factors could be contamination of porcelain to the inner surface of metal coping and reduction in resilience of metal,20 the degassing stage and the final glaze stage of the porcelain firing cycle.21 However, other studies found that porcelain application had no effect on casting distortion.22-24 No differences were found for the horizontal fit after porcelain firings between as-cast and after soldering specimens.25-27
Further studies are necessary to evaluate whether the diagonally welded frameworks are capable of providing sufficient strength to withstand the occlusal forces that the frameworks are subjected during chewing.
This study presented a way to minimize framework misfit and its associated problems by transversely sectioning in a diagonal section through the framework before casting and after one-piece castings. This procedure increased the accuracy of fit and passivity of the frameworks, thus helping to create a successful prosthetic rehabilitation.
Figures and Tables
ACKNOWLEDGEMENTS
The authors thank Neodent (Curitiba, PR, Brazil) for providing the implants and implant components.
The authors declare that they have no conflict of interest.
References
1. Sahin S, Cehreli MC. The significance of passive framework fit in implant prosthodontics: current status. Implant Dent. 2001. 10:85–92.
2. Kohorst P, Brinkmann H, Li J, Borchers L, Stiesch M. Marginal accuracy of four-unit zirconia fixed dental prostheses fabricated using different computer-aided design/computer-aided manufacturing systems. Eur J Oral Sci. 2009. 117:319–325.
3. Jemt T. Failures and complications in 391 consecutively inserted fixed prostheses supported by Brånemark implants in edentulous jaws: a study of treatment from the time of prosthesis placement to the first annual checkup. Int J Oral Maxillofac Implants. 1991. 6:270–276.
4. Tiossi R, Rodrigues RC, de Mattos Mda G, Ribeiro RF. Comparative analysis of the fit of 3-unit implant-supported frameworks cast in nickel-chromium and cobalt-chromium alloys and commercially pure titanium after casting, laser welding, and simulated porcelain firings. Int J Prosthodont. 2008. 21:121–123.
5. Clelland NL, Carr AB, Gilat A. Comparison of strains transferred to a bone simulant between as-cast and postsoldered implant frameworks for a five-implant-supported fixed prosthesis. J Prosthodont. 1996. 5:193–200.
6. Koke U, Wolf A, Lenz P, Gilde H. In vitro investigation of marginal accuracy of implant-supported screw-retained partial dentures. J Oral Rehabil. 2004. 31:477–482.
7. Silva TB, De Arruda Nobilo MA, Pessanha Henriques GE, Mesquita MF, Guimaraes MB. Influence of laser-welding and electroerosion on passive fit of implant-supported prosthesis. Stomatologija. 2008. 10:96–100.
8. de Sousa SA, de Arruda Nobilo MA, Henriques GE, Mesquita MF. Passive fit of frameworks in titanium and palladium-silver alloy submitted the laser welding. J Oral Rehabil. 2008. 35:123–127.
9. Tiossi R, Falcão-Filho H, Aguiar Júnior FA, Rodrigues RC, Mattos Mda G, Ribeiro RF. Modified section method for laser-welding of ill-fitting cp Ti and Ni-Cr alloy one-piece cast implant-supported frameworks. J Oral Rehabil. 2010. 37:359–363.
10. de Aguiar FA Jr, Tiossi R, Rodrigues RC, Mattos Mde G, Ribeiro RF. An alternative section method for casting and posterior laser welding of metallic frameworks for an implantsupported prosthesis. J Prosthodont. 2009. 18:230–234.
11. Kikuchi H, Kurotani T, Kaketani M, Hiraguchi H, Hirose H, Yoneyama T. Effect of laser irradiation conditions on the laser welding strength of cobalt-chromium and gold alloys. J Oral Sci. 2011. 53:301–305.
12. Sartori IA, Ribeiro RF, Francischone CE, de Mattos Mda G. In vitro comparative analysis of the fit of gold alloy or commercially pure titanium implant-supported prostheses before and after electroerosion. J Prosthet Dent. 2004. 92:132–138.
13. Watanabe I, Watanabe E, Atsuta M, Okabe T. Tensile strength of soldered gold alloy joints. J Prosthet Dent. 1997. 78:260–266.
14. Fonseca JC, Henriques GE, Sobrinho LC, de Góes MF. Stress-relieving and porcelain firing cycle influence on marginal fit of commercially pure titanium and titanium-aluminum-vanadium copings. Dent Mater. 2003. 19:686–691.
15. Wettstein F, Sailer I, Roos M, Hämmerle CH. Clinical study of the internal gaps of zirconia and metal frameworks for fixed partial dentures. Eur J Oral Sci. 2008. 116:272–279.
16. Jemt T, Book K. Prosthesis misfit and marginal bone loss in edentulous implant patients. Int J Oral Maxillofac Implants. 1996. 11:620–625.
17. Shimakura M, Yamada S, Takeuchi M, Miura K, Ikeyama J. Influence of irradiation conditions on the deformation of pure titanium frames in laser welding. Dent Mater J. 2009. 28:243–247.
18. Nuñez-Pantoja JM, Vaz LG, Nóbilo MA, Henriques GE, Mesquita MF. Effects of laser-weld joint opening size on fatigue strength of Ti-6Al-4V structures with several diameters. J Oral Rehabil. 2011. 38:196–201.
19. Zupancic R, Legat A, Funduk N. Tensile strength and corrosion resistance of brazed and laser-welded cobalt-chromium alloy joints. J Prosthet Dent. 2006. 96:273–282.
20. Gemalmaz D, Berksun S, Alkumru HN, Kasapoglu C. Thermal cycling distortion of porcelain fused to metal fixed partial dentures. J Prosthet Dent. 1998. 80:654–660.
21. Bridger DV, Nicholls JI. Distortion of ceramometal fixed partial dentures during the firing cycle. J Prosthet Dent. 1981. 45:507–514.
22. Campbell SD, Pelletier LB. Thermal cycling distortion of metal ceramics: Part I-Metal collar width. J Prosthet Dent. 1992. 67:603–608.
23. Campbell SD, Sirakian A, Pelletier LB, Giordano RA. Effects of firing cycle and surface finishing on distortion of metal ceramic castings. J Prosthet Dent. 1995. 74:476–481.
24. Twiggs SW, Searle JR, Ringle RD, Fairhurst CW. A rapid heating and cooling rate dilatometer for measuring thermal expansion in dental porcelain. J Dent Res. 1989. 68:1316–1318.
25. Bryant RA, Nicholls JI. Measurement of distortions in fixed partial dentures resulting from degassing. J Prosthet Dent. 1979. 42:515–520.
26. Ziebert GJ, Hurtado A, Glapa C, Schiffleger BE. Accuracy of one-piece castings, preceramic and postceramic soldering. J Prosthet Dent. 1986. 55:312–317.
27. Zervas PJ, Papazoglou E, Beck FM, Carr AB. Distortion of three-unit implant frameworks during casting, soldering, and simulated porcelain firings. J Prosthodont. 1999. 8:171–179.




 PDF
PDF ePub
ePub Citation
Citation Print
Print





 XML Download
XML Download