Abstract
Implant-supported overdenture is a reliable treatment option for the patients with edentulous mandible when they have difficulty in using complete dentures. Several options have been used for implant-supported overdenture attachments. Among these, bar attachment system has greater retention and better maintainability than others. SFI-Bar® is prefabricated and can be adjustable at chairside. Therefore, laboratory procedures such as soldering and welding are unnecessary, which leads to fewer errors and lower costs. A 67-year-old female patient presented, complaining of mobility of lower anterior teeth with old denture. She had been wearing complete denture in the maxilla and removable partial denture in the mandible with severe bone loss. After extracting the teeth, two implants were placed in front of mental foramen, and SFI-Bar® was connected. A tube bar was seated to two adapters through large ball joints and fixation screws, connecting each implant. The length of the tube bar was adjusted according to inter-implant distance. Then, a female part was attached to the bar beneath the new denture. This clinical report describes two-implant-supported overdenture using the SFI-Bar® system in a mandibular edentulous patient.
Most edentulous patients have used complete dentures from dentistry in early days. Patients are provided with functional recovery and esthetical satisfaction at a lower cost.1 However, severe alveolar bone loss can be observed in patients who have worn complete dentures for a long time and inferior alveolar nerve may be near the alveolar ridge due to that process. This may lead to denture instability and soreness at sharpened alveolar ridge, especially in the mandible. To solve this problem, two to four implants can be placed into the mandibular anterior region to support overdenture. Ball attachments, magnetic attachments, bar attachment systems, and telescopic crowns have been used to anchor the overdenture. Among these systems, bar attachment system has the greatest retention.2,3 On the other hand, increased chair time and high cost of fabrication are problems in that system. In addition, for appropriate adaptation of the bar, soldering or laser welding procedure is often necessary to compensate the dimensional change due to the errors arising from some procedures such as impression making and laboratory process.
The recently developed SFI-Bar® (Cendres + Métaux, Biel/Bienne, Switzerland) can overcome these weak points. According to manufacturer, SFI-Bar® aims to reduce chair time to practitioner and mechanical stress to implant. The SFI-Bar® system consists of two or four implant adapters which are mounted on the implants. Two or four large ball joints are secured on the adapters by fixation screws and tube bar then connects the two ball joints. The length of tube bar can be adjustable according to the inter-implant distance, between 10 and 26 mm. The inter-implant distance is measured with a tube bar gauge, and subsequently the tube bar is shortened to adjust the bar to the ball joints. In addition, the adaptor is allowed to have 30 degree of implant angulation in order to compensate a range of the angular difference between the implants. This system is a "chairside" system, as all preparations can be inserted into the patient's mouth after the implants have been put into place. It is also possible to make this system on the master model at the dental laboratory during fabrication of new denture. Customization of the bar components may be done directly at the dental chair with existing denture or indirectly at the dental laboratory with new denture.
This clinical report describes two-implant-supported overdenture using the SFI-Bar® system in a mandibular edentulous patient.
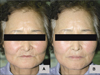
A 67-year-old woman was presented at the department of prosthodontics, Ajou university hospital, complaining of mobility in mandibular anterior teeth. She had been wearing removable partial denture (RPD) on the mandible and complete denture (CD) on the maxilla. Severe bone loss was observed in the mandible (Fig. 1).
The results of radiographs and clinical evaluation showed that the mobility and periapical pathosis of the mandibular anterior teeth were so severe that extraction was decided. She had adverse drug reaction from non-steroidal anti-inflammatory drug (NSAID) and was referred to the department of allergy. Extractions were performed in the department of oral surgery after drug allergy tests to find drugs caused no allergy. After extraction, alginate impressions (Aroma Fine DF II, GC, Tokyo, Japan) were made for provisionalization. Wax rim was then made on the working model. During try in, occlusal plane of the wax rim was set with reference to the interpupillary line and camper plane. After vertical dimension (VD) was determined by using physiological rest position and Willis method,4 facial appearance were assessed. Centric relation (CR) bite was taken by bilateral manipulation guidance with vinyl polysiloxane bite registration paste (Blumousse, Parkell, NY, USA), then transferred to semi-adjustable articulator (Hanau, Waterpik, NY, USA) with face-bow transfer. Wax denture try-in for the maxilla and mandible were done and the patient was satisfied with her appearance. Provisional CDs were delivered and relined with Coe-Soft™ (GC America, Alsip, IL, USA). Periodic recall examination was done.
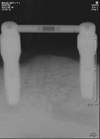
Six months after extraction, radiographic stent was made using existing provisional denture and was switched to surgical stent after taking of computerized tomography (CT) scan. Following the analysis of CT, 13 mm-length implants were determined in the area of mandibular left canine and mandibular right canine. 4.0×13 mm US II implants (Osstem, Busan, Korea) were installed at both mandibular canine regions5 and cover screw was connected to each implant.
Three months later, secondary surgery was performed and 4 mm-height healing abutments were connected (Osstem, Busan, Korea). After 1 month of soft tissue healing, alginate impressions (Aroma Fine DF II, GC, Tokyo, Japan) were made for an individual tray. Functional impressions were taken for CD in the maxilla and implant-supported overdenture in the mandible at the fixture level by pick-up impression technique using regular type vinyl polysiloxane impression materials (Express, 3M ESPE, MN, USA).
On master cast, SFI-Bar® adapters (Cendres + Métaux, Biel/Bienne, Switzerland) (Fig. 2A) were connected to each fixture analog and the inter-implant distance was measured. The height of the adapters were 3 mm and 1 mm, respectively parallel with occlusal plane. After connecting ball joint to one side of tube bar (Cendres + Métaux, Biel/Bienne, Switzerland) (Fig. 2B), tube bar gauge (Cendres + Métaux, Biel/Bienne, Switzerland) was connected to the other side of the tube bar. Then the ball joint was connected with one adapter and a curved surface of tube bar gauge was seated on the other adapter (Fig. 3A). Tube bar was then cut off at the gap of tube bar gauge with Premium Disc (Cendres + Métaux, Biel/Bienne, Switzerland) (Fig. 3B). The SFI-Bar® female (Cendres + Métaux, Biel/Bienne, Switzerland) made up of gold alloy was cut and prepared according to the length of the bar.
During laboratory procedure, metal portion above the bar was opened so that the gold female part can be attached to overdenture in clinical office. Metal frameworks of maxillary CD and mandibular implant-supported overdenture were fabricated. Wax rim and wax denture try-in for the maxilla and mandible were performed in the same manner with provisional denture. VD was determined as the value of existing provisional denture. After curing of dentures in common way, retention and occlusion were checked and clinical remounting was done.
Adapters were then connected to the implant fixtures in the mouth with 35 Ncm (Fig. 4). Periapical standard view was taken to verify connection. The ball joints were secured to the adapters by fixation screws with 20 Ncm, and prepared tube bar was also connected to the ball joints. Marginal fits of the SFI-Bar® were evaluated with periapical radiograph. After checking occlusion, retention, and facial appearance (Fig. 5), the final dentures were delivered without connecting the female part and daily maintenance care was instructed using interdental cleansing aids.
At the next recall appointment, female part was attached to the bar. The space under the bar was blocked out with utility wax (Fig. 6) and the gold female part was attached to the denture with self-curing processing material (Vertex-Dentimex, Zeist, Netherlands) in the mouth under habitual bite force (Fig. 7). Management of tooth brushing was performed through periodic recall check and peri-implant bone was assessed with radiographs (Fig. 8). The activation of gold female part was not required during periodic recall appointment.
Compared with complete denture, implant-supported overdenture improves the stability of the prosthesis. Increased number of implants may guarantee more retention. However, there is a problem of increased cost and anatomical limitations in severely resorbed residual ridges, especially in the mandible. Several studies demonstrated that the two-implants-supported overdenture therapy can be considered as a very reliable treatment for patients with an edentulous mandible.5-7 Therefore, two-implants-supported overdenture in the mandible should be the standard treatment modality for full edentulous patients suffering from discomfort with their conventional denture.5-7
Immediate or early loading protocols for the edentulous mandible offer the patient with many advantages in terms of decreased number of visits, early functional recovery, and reduction of surgical exposure.8 Short-term outcomes of immediate or early loading protocols for mandibular implant-supported overdenture showed success, comparable to delayed loading protocols in curtained cases. However, this treatment option is not universally appropriate for all patients. Although no evidence was found in long-term studies to support delayed loading protocols for mandibular implant-supported overdenture, delayed loading of prosthesis is expected to show better results than immediate or early loading.9 Further long-term studies concerning loading protocol of mandibular implant-supported overdenture are required. Implant can be placed either by 1-stage procedure or 2-stage procedure to set load-free for a few months. If the optimal implant stability is not achieved or if there is a risk that the provisional denture transmits excessive forces to the implants, the 2-stage procedure could be preferable.10 We conducted 2-stage submerged implants in this case with delayed loading.
There are various options for implant-supported overdenture attachments. There is no difference in implant survival rates, peri-implant outcome and patient satisfaction regardless of splinting.11 However, several articles showed that the non-splinted design requires more prosthetic maintenance and the bar attachment system has been shown to be a more successful prosthesis.11 While bar system has the best maintainability,2 laboratory procedures such as soldering and welding give rise to errors and increase in cost. Besides, several bar framework material such as gold alloy, silver-palladium alloy, commercially pure titanium, and cobalt-chromium alloy presented a lower effect on the stress distribution of an overdenture.12
SFI-Bar® was recently developed and made up for the weakness of casting bar attachment system. According to manufacturer, due to the telescopic design of the bar joints, no lateral stress is applied to the implants. The risk of implant failure is therefore significantly reduced. However, further long-term studies concerning lateral stress on implants with this system are required. Prefabricated bar of SFI-Bar® attachment is round shape. Compared to other bar forms such as ovoid-shaped or parallel-wall shaped bar, round bar allows more rotational movements of the overdenture. Deslis et al. described that there may be little denture-fracture probably due to the possible movement over the round bar.13 Metal framework reinforcement is not required for a SFI-Bar® on two-implants. As some parts of the system are not fixed to bar by soldering or welding, there is room for stress release that avoids implant preload. Moreover, the absence of soldering joints, which sometimes reduces the length of the retentively usable bar surfaces, also can be advantageous. Since soldering is not required and titanium grade 5 is used as bar material, there is no risk of corrosion. Two concepts of female parts are available in this system. One is the milled gold female part with asymmetrical design of the retention in the resin for more room in the tongue area and a better esthetic. This female part can be adjusted and cut individually. The other is the titanium female part with replaceable plastic retention inserts for adjusting the retention force. Three retention levels are available. According to manufacturer, the titanium matrix with plastic inserts as a female part for SFI-Bar® on two implants is not recommended due to excessive wear at the titanium male parts.
In this case, the patient is satisfied with good function and favorable esthetics by using implant-supported overdenture. However, periodic recall check is necessary and long-term clinical results are required.
Figures and Tables
Fig. 2
Components of SFI-Bar®. A: Adapters, B: Fixation screw, large ball joint, and tube bar, C: Assembled bar component which will be secured on adapters.

Fig. 3
Customization of the bar. A: After combining ball joint and tube bar on one side, the tube bar gauge was connected on the other side, B: Tube bar was cut off at the gap of tube bar gauge with disc.

Fig. 5
Extraoral photographs. A: Before delivery of final denture, B: After delivery of final denture.
References
1. Bilhan H, Erdogan O, Ergin S, Celik M, Ates G, Geckili O. Complication rates and patient satisfaction with removable dentures. J Adv Prosthodont. 2012. 4:109–115.
2. Takeshita S, Kanazawa M, Minakuchi S. Stress analysis of mandibular two-implant overdenture with different attachment systems. Dent Mater J. 2011. 30:928–934.
3. van Kampen F, Cune M, van der Bilt A, Bosman F. Retention and postinsertion maintenance of bar-clip, ball and magnet attachments in mandibular implant overdenture treatment: an in vivo comparison after 3 months of function. Clin Oral Implants Res. 2003. 14:720–726.
4. Fenlon MR, Sherriff M, Walter JD. Association between the accuracy of intermaxillary relations and complete denture usage. J Prosthet Dent. 1999. 81:520–525.
5. Feine JS, Carlsson GE, Awad MA, Chehade A, Duncan WJ, Gizani S, Head T, Heydecke G, Lund JP, MacEntee M, Mericske-Stern R, Mojon P, Morais JA, Naert I, Payne AG, Penrod J, Stoker GT, Tawse-Smith A, Taylor TD, Thomason JM, Thomson WM, Wismeijer D. The McGill consensus statement on overdentures. Mandibular two-implant overdentures as first choice standard of care for edentulous patients. Gerodontology. 2002. 19:3–4.
6. Vercruyssen M, Marcelis K, Coucke W, Naert I, Quirynen M. Long-term, retrospective evaluation (implant and patient-centred outcome) of the two-implants-supported overdenture in the mandible. Part 1: survival rate. Clin Oral Implants Res. 2010. 21:357–365.
7. Thomason JM, Kelly SA, Bendkowski A, Ellis JS. Two implant retained overdentures-a review of the literature supporting the McGill and York consensus statements. J Dent. 2012. 40:22–34.
8. Hong JW, Ahn SG, Leem DH, Seo JM. Immediate placement and functional loading of implants on canine with fixed partial denture for a patient having canine protected occlusion: a case report. J Adv Prosthodont. 2012. 4:52–56.
9. Esposito M, Grusovin MG, Willings M, Coulthard P, Worthington HV. Interventions for replacing missing teeth: different times for loading dental implants. Cochrane Database Syst Rev. 2007. 04. 18. (2):CD003878.
10. Esposito M, Grusovin MG, Chew YS, Coulthard P, Worthington HV. Interventions for replacing missing teeth: 1- versus 2-stage implant placement. Cochrane Database Syst Rev. 2009. 07. 08. (3):CD006698.
11. Stoumpis C, Kohal RJ. To splint or not to splint oral implants in the implant-supported overdenture therapy? A systematic literature review. J Oral Rehabil. 2011. 38:857–869.
12. Spazzin AO, Dos Santos MB, Sobrinho LC, Consani RL, Mesquita MF. Effects of horizontal misfit and bar framework material on the stress distribution of an overdenture-retaining bar system: a 3D finite element analysis. J Prosthodont. 2011. 20:517–522.
13. Deslis A, Hasan I, Bourauel C, Bayer S, Stark H, Keilig L. Numerical investigations of the loading behaviour of a prefabricated non-rigid bar system. Ann Anat. 2012. 05. 11.




 PDF
PDF ePub
ePub Citation
Citation Print
Print






 XML Download
XML Download