Abstract
PURPOSE
The aim of this systematic review is to address treatment outcomes of Mandibular implant overdentures relative to implant survival rate, maintenance and complications, and patient satisfaction.
MATERIALS AND METHODS
A systematic literature search was conducted by a PubMed search strategy and hand-searching of relevant journals from included studies. Randomized Clinical Trials (RCT) and comparative clinical trial studies on mandibular implant overdentures until August, 2010 were selected. Eleven studies from 1098 studies were finally selected and data were analyzed relative to number of implants.
RESULTS
Six studies presented the data of the implant survival rate which ranged from 95% to 100% for 2 and 4 implant group and from 81.8% to 96.1% for 1 and 2 implant group. One study, which statistically compared implant survival rate showed no significant differences relative to the number of implants. The most common type of prosthetic maintenance and complications were replacement or reattaching of loose clips for 2 and 4 implant group, and denture repair due to the fracture around an implant for 1 and 2 implant groups. Most studies showed no significant differences in the rate of prosthetic maintenance and complication, and patient satisfaction regardless the number of implants.
A mandibular implant supported overdenture is an excellent treatment option for fully edentulous patients in terms of masticatory function, chewing ability and patient's satisfaction. To improve support and stability of a denture, various numbers of implants (typically one, two, or four) have been recommended for mandibular implant overdentures. McGill1 and York2 consensus reports declared that the two implants overdenture for the mandible was recommended as the first treatment option for edentulous patients.
Four implants have been suggested as one of the treatment options for edentulous patients seeking mandibular implant overdentures. However, in terms of prosthetic maintenance and complications, and patient satisfaction, two and four implant groups do not appear to be significantly different.3 Therefore, two implants have been considered to be a more reasonable treatment option based on presumed cost-effectiveness. Meanwhile, a single implant has recently been proposed to be adequate for retention of the mandibular overdenture and suggested as an alternative for edentulous patients.4-7 However, very few studies have compared the number of implants in a manner useful for clinical decision-making. A recent review showed patient satisfaction and function of the prosthesis did not seem to be dependent on the number of implants.8 However, the review lacked methodological description, which means a narrative rather than systematic approach. Therefore we conducted a controlled systematic review, focused on comparing outcomes between various numbers of implants.
This systematic review aimed to address treatment outcomes related to the number of implants for mandibular implant overdentures in terms of 1) implant survival rate, 2) maintenance and complications, and 3) patient satisfaction.
The PICO format (Population, Intervention, Comparisons, Outcomes)9 was used to define a clear clinical question. In comparative clinical studies involving completely edentulous participants (P) requiring mandibular implant overdentures opposing conventional maxillary complete denture (I) with various numbers of implants (one, two, and four) (C), what were the survival rate of implants, prosthetic maintenance and complications, and patient satisfaction outcomes (O).
A systematic literature search was conducted using the combined Mesh terms ("mandibular prosthesis" or "Denture, Overlay") and ("dental implants" or "dental prosthesis, implant supported") and ("clinical study" or "comparative study" or "outcome assessment" or "epidemiologic studies" or "intervention studies" or "patient satisfaction") and limited by ("Human" and "English") in the databases, Medical Literature Analysis and Retrieval System Online (MEDLINE). The aim was to identify all publications comparing the number of implants for up to and including August 1, 2010.
The electronic search was further augmented by hand search through the following journals: Clinical Implant Dentistry and Related Research, Clinical Oral Implants Research, Implant Dentistry, International J of Oral and Maxillo-facial Implants, International J of Oral and Maxillo-facial Surgery, International J of Periodontics & Restorative Dentistry, International J of Prosthetics, J of Clinical Periodontology, J of Dental Research, J of Oral Implantology, J of Oral and Maxillo-facial Surgery, J of oral Rehabilitation, J of Periodontology, J of Prosthetics, J of Prosthetic Dentistry, and Periodontology 2000.
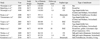
RCT, quasi-randomized and comparative clinical trial studies on mandibular implant overdentures (MIO) until August, 2010 were selected. Only root form endosseous standard implants were considered. The opposing dentition was conventional complete maxillary denture. Finally, only studies published in English were included. Meanwhile, case reports or technical reports without a statistical comparison were excluded. The duration of follow-up period less than 1 year of function was excluded as were studies without implant survival, prosthetic or patient satisfaction evaluation. Both rigid types of applications such as milled bar or combinations of attachment types, and cantilevered applications of attachments were also excluded. Papers without abstracts were also excluded (Table 1).
At the outset, two independent reviewers evaluated selection of the articles based on the established inclusion and exclusion criteria. The sample size, patient age, observation period, type of implant, number of implant, type of attachment, treatment outcomes and the outcome of statistical analysis were extracted from each included article. Analysis was based on the implant survival rate, prosthetic maintenance and complications, and patient satisfaction.
The implant survival rate denotes the percentage of implants still present at follow-up after initial placement of implants. Prosthetic maintenance and complications denoted mechanical damage of the implant superstructures. Among these, 'matrix or clip loosening', 'detachment or loss of matrix' and 'fracture of mandibular denture-base' were reporter. Prosthetic maintenance and complications were classified to the type and frequency relative to the number of implants as far as possible. Patient satisfaction concerning chewing ability, phonetics, and social function were evaluated by mean "a score of six scales questionnaire", a visual analogue scale (VAS), or in some cases by mention of patient preference.
The PubMed search yielded 1098 titles. Thirteen publications were selected by independent screening of the titles and abstracts from the PubMed search. According to the established inclusion exclusion criteria. In addition, one publication was also included by hand search (Fig. 1). Based upon reading the fourteen full text articles, a total of eleven studies were finally selected and divided according to the number of implant (one, two, or four) in terms of survival rate of implants, prosthetic maintenance and complications, and patient's satisfaction. Eight studies3,10-16 compared 2 and 4 implant groups with bar attachments. Three studies7,17,18 compared 1 and 2 implant overdenture group with ball attachments (Table 2).
Six papers7,10,11,14,15,18 presented data on the implant survival which ranged from 95.0% to 100% for 2 and 4 implant group and from 81.8% to 96.1% for 1 and 2 implant group, the latter range including 81.8% survival for immediately loaded implants. In a comparison of 2 and 4 implant group, Meijer et al.11 showed that there was no significant difference between the groups. Visser et al.14 showed a survival rate of 98.3% for a two implant group and 100% for a four implant group without statistical analysis. A pooled survival rate of 99.4% was presented by Batenburg et al.10 and that of 97.9% was presented by Wismeijer et al.15 Meanwhile, in a comparison of 1 and 2 implant groups, Walton et al.7 showed a pooled survival rate of 96.1%. Kronstrom et al.18 showed the lowest pooled survival rate of 81.8% following immediate loading.
Six studies7,11,13,14,17,18 presented data on prosthetic maintenance and complications. Replacing new clips or reattaching loose clips was the most common type of prosthetic maintenance and complications with 2 and 4 implant overdentures with bar attachments, followed by repairing a fractured denture base or artificial teeth. According to Visser et al.,14 a 2 implant overdenture group had a tendency for a greater need of prosthetic aftercare than that of a 4 implant overdenture. However, the study by Stoker et al.13 and Meijer et al.11 showed no significant difference in rate of prosthetic complications between 2 and 4 implant group (Table 3). Meanwhile the 1 year randomized controlled study by Walton et al.,7 found that the most frequent maintenance event was repairing a broken denture around the implant in the 1 implant group and replacing a loose matrix in the 2 implant group, but the differences were not statistically significant. In a follow-up of this study from 1 to nearly 5 years, Gonda et al.17 also found a tendency for slightly more frequent denture base fractures in the 1 implant group beyond the first year, but the rate also was not significantly different. Replacing retentive O-rings was reported as the most common prosthetic maintenance, in the study of immediately loaded 1 and 2 implant groups by Kronstrom et al.18 but there was no significant difference in rates (Table 4). Most studies showed no significant differences in the rate of prosthetic maintenance and complication regardless the number of implants in both 2 and 4 implant groups, and 1 and 2 implant groups.
Five studies3,11,14,16,18 presented patient satisfaction comparisons for mandibular implant overdentures. The methods to measure how much patients were satisfied with their denture mostly depended on a questionnaire. Several items such as speech, aesthetics, retention, mastication, and social function were used and the scales of patient satisfaction varier across studies. The four studies3,11,14,16 comparing 2 and 4 implant group showed that there was no significant different between the groups (Table 3). Walton et al.7 evaluated overall patient satisfaction with a VAS scale and also showed no significant different between 1 and 2 implant group (Table 4). However, the participants were on average far more satisfied after overdenture treatment than before treatment irrespective of the number of implants. All studies showed there was no significant difference in patient satisfaction regardless the number of implants in both 2 and 4 implant groups, and 1 and 2 implant groups.
This systematic review of randomized and comparative clinical trials examined the treatment outcomes of mandibular implant-supported overdentures relative to implant survival rate, maintenance complications, and patient satisfaction. Data related to implant survival rates were insufficient to conduct a statistical meta-analysis on those factors, so data were descriptively analyzed. The follow-up period of the trials ranged from 1 to 10 years, and the survival rate of the implants in 10 of the 11 trials ranged from 95% to 100% under conventional loading. One trial loaded one or two implants with an overdenture immediately on implant insertion and reported the lowest implant survival rate of 82% after one year.18 It is reasonable to conclude therefore that the prognosis of one or more implants loaded conventionally after a few months is excellent independent of the number of implants.
The most common complication in maintaining implant overdentures involves loosening of attachment devices and fractured dentures. There was some indication that fractured dentures are more common during the first year when the denture rests only on one implant.7 However, the incidence of fractures seems to even out between the group in subsequent years.17 Nonetheless, there might be some benefit, at least during the first year, in reinforcing the denture base around the implant.19 It is important also to realize that the duration of the trial reporting on overdentures with one implant is still relatively short. Perhaps as time progresses, the stress concentrated by one implant rather than multiple implants, on the denture may indeed result in a greater incidence of fractures.
The number of implants did not increase significantly the satisfaction of the patients with the overdenture. Apparently patient satisfaction following the transition to an implant supported denture from conventional mucosal support is very substantial in all of the trials we reviewed. Consequently, any subtle advantage that might occur from multiple implants, at least in the short-term, is not measureable, and especially when the psychometric instrument, such as a structured questionnaire, is relatively insensitive.20 Indeed, the difference between satisfaction from dentures on one or two implants did not appear even with the potentially more sensitive VAS used by Walton et al.7
The single implant overdenture has benefits for cost effectiveness, and the optimally simplified surgical and prosthetic procedures. Component cost was significantly saved in a single implant group.7 Time savings for the single implant were 22% at implant placement, 16% for relining to add the attachment, and 24% for postsurgical complications and denture adjustments.7 However, a review study21 on seven single implant overdenture publications up to August, 2008 found the single implant survival rate was 100% under conventional loading and about 82% under immediate loading. A mandiblular single implant overdenture may be considered very promising treatment option based on this review.21 However, several dangers related to surgical placement of single implants in the mandibular midline were reported.21-24 For example, severely resorber residual ridge and the presence of certain blood vessels in the central of mandible might cause severe hemorrhage during surgery in the floor of the mouth. Despite this problem, it is reasonable to state that the outcome of overdentures on a single implant seems very encouraging as a cost-effective and relatively non-invasive procedure with a very acceptable prognosis at present.
The survival rate of implant supporting mandibular overdentures is high regardless of the number of implants. Denture maintenance is likely not influenced substantially by the number of implnats and patient satisfaction is typically high again regardless of the number of implants supporting and retaining the overdenture.
Figures and Tables
References
1. Feine JS, Carlsson GE, Awad MA, Chehade A, Duncan WJ, Gizani S, Head T, Lund JP, MacEntee M, Mericske-Stern R, Mojon P, Morais J, Naert I, Payne AG, Penrod J, Stoker GT, Tawse-Smith A, Taylor TD, Thomason JM, Thomson WM, Wismeijer D. The McGill consensus statement on overdentures. Mandibular two-implant overdentures as first choice standard of care for edentulous patients. Montreal, Quebec, May 24-25, 2002. Int J Oral Maxillofac Implants. 2002. 17:601–602.
2. Thomason JM, Feine J, Exley C, Moynihan P, Müller F, Naert I, Ellis JS, Barclay C, Butterworth C, Scott B, Lynch C, Stewardson D, Smith P, Welfare R, Hyde P, McAndrew R, Fenlon M, Barclay S, Barker D. Mandibular two implant-supported overdentures as the first choice standard of care for edentulous patients-the York Consensus Statement. Br Dent J. 2009. 207:185–186.
3. Timmerman R, Stoker GT, Wismeijer D, Oosterveld P, Vermeeren JI, van Waas MA. An eight-year follow-up to a randomized clinical trial of participant satisfaction with three types of mandibular implant-retained overdentures. J Dent Res. 2004. 83:630–633.
4. Cordioli G, Majzoub Z, Castagna S. Mandibular overdentures anchored to single implants: a five-year prospective study. J Prosthet Dent. 1997. 78:159–165.
5. Krennmair G, Ulm C. The symphyseal single-tooth implant for anchorage of a mandibular complete denture in geriatric patients: a clinical report. Int J Oral Maxillofac Implants. 2001. 16:98–104.
6. Maeda Y, Horisaka M, Yagi K. Biomechanical rationale for a single implant-retained mandibular overdenture: an in vitro study. Clin Oral Implants Res. 2008. 19:271–275.
7. Walton JN, Glick N, Macentee MI. A randomized clinical trial comparing patient satisfaction and prosthetic outcomes with mandibular overdentures retained by one or two implants. Int J Prosthodont. 2009. 22:331–339.
8. Klemetti E. Is there a certain number of implants needed to retain an overdenture? J Oral Rehabil. 2008. 35:80–84.
9. Needleman IG. A guide to systematic reviews. J Clin Periodontol. 2002. 29:6–9.
10. Batenburg RH, Raghoebar GM, Van Oort RP, Heijdenrijk K, Boering G. Mandibular overdentures supported by two or four endosteal implants. A prospective, comparative study. Int J Oral Maxillofac Surg. 1998. 27:435–439.
11. Meijer HJ, Raghoebar GM, Batenburg RH, Visser A, Vissink A. Mandibular overdentures supported by two or four endosseous implants: a 10-year clinical trial. Clin Oral Implants Res. 2009. 20:722–728.
12. Payne AG, Solomons YF. Mandibular implant-supported overdentures: a prospective evaluation of the burden of prosthodontic maintenance with 3 different attachment systems. Int J Prosthodont. 2000. 13:246–253.
13. Stoker GT, Wismeijer D, van Waas MA. An eight-year follow-up to a randomized clinical trial of aftercare and cost-analysis with three types of mandibular implant-retained overdentures. J Dent Res. 2007. 86:276–280.
14. Visser A, Raghoebar GM, Meijer HJ, Batenburg RH, Vissink A. Mandibular overdentures supported by two or four endosseous implants. A 5-year prospective study. Clin Oral Implants Res. 2005. 16:19–25.
15. Wismeijer D, van Waas MA, Mulder J, Vermeeren JI, Kalk W. Clinical and radiological results of patients treated with three treatment modalities for overdentures on implants of the ITI Dental Implant System. A randomized controlled clinical trial. Clin Oral Implants Res. 1999. 10:297–306.
16. Wismeijer D, Van Waas MA, Vermeeren JI, Mulder J, Kalk W. Patient satisfaction with implant-supported mandibular overdentures. A comparison of three treatment strategies with ITI-dental implants. Int J Oral Maxillofac Surg. 1997. 26:263–267.
17. Gonda T, Maeda Y, Walton JN, MacEntee MI. Fracture incidence in mandibular overdentures retained by one or two implants. J Prosthet Dent. 2010. 103:178–181.
18. Kronstrom M, Davis B, Loney R, Gerrow J, Hollender L. A prospective randomized study on the immediate loading of mandibular overdentures supported by one or two implants: a 12-month follow-up report. Int J Oral Maxillofac Implants. 2010. 25:181–188.
19. Gonda T, Ikebe K, Dong J, Nokubi T. Effect of reinforcement on overdenture strain. J Dent Res. 2007. 86:667–671.
20. Brondani MA, MacEntee MI. The concept of validity in sociodental indicators and oral health-related quality-of-life measures. Community Dent Oral Epidemiol. 2007. 35:472–478.
21. Alsabeeha N, Payne AG, De Silva RK, Swain MV. Mandibular single-implant overdentures: a review with surgical and prosthodontic perspectives of a novel approach. Clin Oral Implants Res. 2009. 20:356–365.
22. Woo BM, Al-Bustani S, Ueeck BA. Floor of mouth haemorrhage and life-threatening airway obstruction during immediate implant placement in the anterior mandible. Int J Oral Maxillofac Surg. 2006. 35:961–964.
23. van den Bergh JP, ten Bruggenkate CM, Tuinzing DB. Preimplant surgery of the bony tissues. J Prosthet Dent. 1998. 80:175–183.
24. Kalpidis CD, Setayesh RM. Hemorrhaging associated with endosseous implant placement in the anterior mandible: a review of the literature. J Periodontol. 2004. 75:631–645.




 PDF
PDF ePub
ePub Citation
Citation Print
Print






 XML Download
XML Download