Abstract
When performing a tooth extraction, imminent collapse of the tissue by resorption and remodeling of the socket is a natural occurrence. The procedure for the preservation of the alveolar ridge has been widely described in the dental literatures and aims to maintain hard and soft tissues in the extraction site for optimal rehabilitation either with conventional fixed or removable prosthetics or implant-supported prosthesis.
After the removal of a tooth, a series of processes including scarring of the alveoli, which features a three-dimensional inevitable loss of alveolar volume by a crestal-lingual displacement of the mucogingival line take place.
It has been suggested that bone resorption occurs because of functional factors, metabolic and anatomic process (Fig. 1).1 The sequela with dental extraction is a 40 to 60% of three-dimensional bone loss over the next 2-3 years following extraction.2
It has been reported that the inevitable collapse both horizontally and vertically is taking place predominantly in the first three months after extraction.3 The extent of horizontal bone loss exceeds almost 3 times the vertical bone loss, since there is horizontal bone loss of 4 to 6 mm, up to 50% of the original width, during the next 6 to 12 months while there is a vertical bone loss of 1 to 3 mm after extraction during the first 6 to 12 months.3 Loss is even more pronounced when loss of adjacent teeth has occured.4
These changes are reflected clinically as changes in the ridge are visible: from the occlusal plane, the residual ridge crest changes its position, being resorbedlingually when compared to the original position before extractions. From the facial/buccal plane, the residual ridge often resorbs forms a depression between the facial/buccal alveolar ridges of the remaining teeth and is more pronounced when more than one tooth has been extracted (Fig. 2).5
A localized alveolar abnormality is even more severe if the facial cortical bone has been destroyed, either by disease or traumatic dental extraction.6 The facial/buccal bone has a higher tendency to resorption because it is thinner, less dense than the lingual cortical bone and less vascularized. Additionally, the epithelium that covers this cortical bone is thinner and the lip pressure over the ridge may also contribute to the bone loss reported.7 It is important to recognize this clinical scenario since implant therapy has established a need for horizontal thickness of at least 2 mm to reduce the vertical bone loss. One study reported that implants that have lost more than 3 mm of vertical bone had an average vestibular bone thickness of 1.3 mm when implant were placed.8
These processes of resorption and remodeling are associated with alveolar bone breakdown that simultaneously threatens the integrity of the soft tissues. This type of resorption, a combination between hard and soft tissue loss occasionally involve the presence of keratinized gingiva and mucogingival line migration in a coronal direction. The gingiva should have a width of at least 2 mm around the implant fixtures to protect it from future chronic irritation during mastication. Otherwise, soft tissue recession may occur leading to resorption and exposure of the implant coronal treads. Therefore, additional procedures will be necessary to augment the alveolar ridge and this will result in extended treatment through increased number of surgeries and higher costs for the patient. As this is not ideal, it may be prevented through planning at time of extraction.9, 10
When an implant restoration is planned, the literature has described procedures to minimize or compensate for the unwanted resorption process. What is required has to do with the severity of the alveolar defect and the need for primary stability in implant dentistry. This will be determined if the fixture is placed immediately in a single step or if multiple interventions are preferred.11,12
A contraindication is acute infection at the time of extraction.15
Traditionally, when performing dental extraction some horizontal displacement movements are performed, twisting and extrusion to luxate and extract the tooth. When it is extracted we have an empty socket and bleeding from the socket walls will lead to the formation of a clot. Some practitioners will compress the cortical plates with finger pressure. Currently this procedure is no longer considered acceptable as it contributes to resorption so that the expected defect is exacerbated.
Broadly, in order to perform the technique for alveolar ridge preservation (ARP), first a minimally invasive tooth extraction is performed and immediately, the socket is filled with biomaterials (bone graft material/collagen) or autogenous bone.16
In the event of a defect in the alveolar bone, its continuity is restored by utilizing collagen membranes before or during the filling of the alveoli. This aids in confining the osseous graft and preventing soft tissue ingrowth during the graft organization period.
The purpose of this procedure is to extract the tooth causing the least damage to the alveoli for the subsequent healing resulting in low bone resorption.
The patient is anesthetized conventionally and the gingival circular ligament is cut in one intention with a microscalpel or microelevator. The same tools can be used to dissect the Sharpey fibers, this is more common in the case of alveolar cancellous bone of the maxilla (Fig. 3). If the tooth has enough coronal surfaces to be retained with a forceps for extraction, this is done carefully and firmly for single-root teeth without using leverage through vertical and slightly rotational movements. If the coronal has significant breakdown or a residual root is present, a cut can be made to separate the tooth at the cervical to allow for easier root removal.17 A bur is then introduced sectioning the root into two halves. It is recommended that this is performed in a buccal-lingual/palatal direction, so that when separating the roots they displace mesiodistally without damaging the buccal plate that is commonly thinner.
For multi-rooted teeth, the vertical separation of roots individually is common with extraction of the individual roots via the use of radicular forceps, trying to avoid horizontal root displacement.18
Care should be taken to preserve as much alveolar walls as possible, to improve blood supply for the biomaterial and thus reduce resorption.
The purpose of this procedure is to minimize bone loss that occurs early after tooth extraction, reducing the need for surgical techniques of alveolar ridge augmentation.19
In the past, there have been several methods ranging from the socket cover with resorbable and non-resorbable membranes to be filled with biomaterials (resorbable and non-resorbable bone substitutes, including growth factors), with or without autogenous bone combined with the use of sponge gelatin or connective tissue.1,2,20-24
After atraumatic extraction, curettage is performed carefully and the socket is irrigated (Fig. 4). Next, the socket is filled with the osseous graft and it is condensed to the crestal level (Fig. 5). The alveolar opening is sealed with a resorbable sponge or membrane cut to size, which is sutured to the surrounding soft tissue to contain the graft within the socket (Fig. 6). The barrier prevents the loss of graft and accelerates the crestal healing of the keratinized gingival. If the alveolar bone has suffered damage, the continuity of the alveolar bone is restored.
The membrane prevents the gingival connective and epithelial migration into the defect and its contained osseous graft,25 as soft tissues grow 6 times faster than the bone tissue, also the membrane aids in clot stabilization.26 The wound stabilization is very important in periodontal repair and may also be of importance for the healing extraction sites (Fig. 7).20 With clot stabilization and isolating it from the epithelial elements provide a predictive maintenance of the alveolar ridge, improving the bone quality for dental implant procedures and restorative dentistry in the esthetic zone (Figs. 8-10).7,27
Among the advantages of ARP, there is a reduced treatment period and the trauma is reduced when compared with the transplanted graft block, preventing displacement of the mucogingival line. This implantation is benefited afterwards from the formation of keratinized soft tissue. It also increases the prosthetic rehabilitation quality and longevity.
When the extension intended to preserve is wide, slowly absorbable or non-resorbable material is recommended.2 To achieve ARP it is more important to use membrane than the filler material.7,21,28 Although we can achieve preservation only with a graft, the use of occlusive membranes on the graft prevents penetration of soft tissue in to the graft. This increases the total amount of vital bone and avoids losing its coronal aspect.29
Resorbable membranes for ARP facilitate future implant placement, especially in the anterior section with thin cortical plates.7
Membranes of collagen can be used in several layers as Shakibaie18 observed crestal-facial/buccal gingival thickening, which has particular interest in implantology.
In histological animal studies, Araujo demonstrated that the volume of preservation obtained with ARP can be reabsorbed again in the absence of a stimulus to the bone via implant loading.30 Bone is a specialized connective tissue with a calcified extracellular matrix and is dynamic for being in constant renovation.31 For more than a century, it has been known and accepted that to preserve bone, adequate forces through occlusal loading are necessary to stimulate the supporting bone to prevent resorption a form of osseous atrophy.32
The stimulus can only be provided from within by either natural teeth or implants.
In the aforementioned study by Shakibaie,18 it was demonstrated that there is an unquestionable need to use ARP. It was shown that in only 1 out of 10 patients with ARP requires an augmentation procedure to receive the implant properly. On the contrary, those who received no treatment for preservation, 6 out of 10 required augmentative procedures to make suitable the alveolar ridge for dental implant placements.
Given the vast scientific evidence and documentation of the above information, the benefits of conducting ARP in a regular basis is emphasized, it should be implemented from undergraduate training universities to institutions in the health system, rather than the traditional procedure that has been be considered obsolete for worsening the bone condition.
It is recommended to use an absorbable membrane independently of the biomaterial filler utilized. ARP improves the prognosis by maintaining the residual bone and reduce the need for surgical procedures for ridge augmentation. Thus, and increase in the success of tooth-born and implant-supported restorations is observed.
Figures and Tables
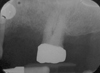
Fig. 1
Preoperative periapical radiograph demonstrating bone loss related to periodontal disease of the maxillary left 1st premolar necessitating extraction.

Fig. 4
Cortical perforations have been placed in the edentulous area on the buccal aspect of the ridge.

Fig. 7
Primary closure has been achieved and the site has been closed with a sufficient number of sutures.

References
1. Jahangiri L, Devlin H, Ting K, Nishimura I. Current perspectives in residual ridge remodeling and its clinical implications: a review. J Prosthet Dent. 1998. 80:224–237.
2. Ashman A. Ridge preservation: important buzzwords in dentistry. Gen Dent. 2000. 48:304–312.
3. Schropp L, Wenzel A, Kostopoulos L, Karring T. Bone healing and soft tissue contour changes following single-tooth extraction: a clinical and radiographic 12-month prospective study. Int J Periodontics Restorative Dent. 2003. 23:313–323.
4. Chen ST, Wilson TG Jr, Hämmerle CH. Immediate or early placement of implants following tooth extraction: review of biologic basis, clinical procedures, and outcomes. Int J Oral Maxillofac Implants. 2004. 19:12–25.
5. Pietrokovski J. The bony residual ridge in man. J Prosthet Dent. 1975. 34:456–462.
6. O'Brien TP, Hinrichs JE, Schaffer EM. The prevention of localized ridge deformities using guided tissue regeneration. J Periodontol. 1994. 65:17–24.
7. Lekovic V, Camargo PM, Klokkevold PR, Weinlaender M, Kenney EB, Dimitrijevic B, Nedic M. Preservation of alveolar bone in extraction sockets using bioabsorbable membranes. J Periodontol. 1998. 69:1044–1049.
8. Spray JR, Black CG, Morris HF, Ochi S. The influence of bone thickness on facial marginal bone response: stage 1 placement through stage 2 uncovering. Ann Periodontol. 2000. 5:119–128.
9. Hämmerle CH, Jung RE, Yaman D, Lang NP. Ridge augmentation by applying bioresorbable membranes and deproteinized bovine bone mineral: a report of twelve consecutive cases. Clin Oral Implants Res. 2008. 19:19–25.
10. Terheyden H, Iglhaut G. Chirurgische. Versorgung der Extraktionsalveole. Z Zahnärztl Impl. 2006. 22:42–45.
11. Glauser R, Zembic A, Hämmerle CH. A systematic review of marginal soft tissue at implants subjected to immediate loading or immediate restoration. Clin Oral Implants Res. 2006. 17:82–92.
12. Hämmerle C, Chen ST, Wilson T. Konsensuserklärung und empfohlene klinische Verfahren zum Einsetzen von Implantaten in Extraktionsalveolen. Implantologie. 2006. 14:335–338.
13. Solís-Moreno C, Nart-Molina J, Violant-Holz D, Santos-Alemany A. Tratamiento del alvéolo post-extracción. Revisión de la literatura actual. Rev Esp Odontoestomatológica de Implantes. 2009. 17:7–17.
14. Nart J, Marcuschamer E, Rumeu J, Santos A, Griffin TJ. Preservacion del reborde alveolar. Por que y cuando. Periodoncia Y Osteointegracion. 2007. 17:229–237.
15. John V, De Poi R, Blanchard S. Socket preservation as a precursor of future implant placement: review of the literature and case reports. Compend Contin Educ Dent. 2007. 28:646–653.
16. Danza M, Guidi R, Carinci F. Spiral family implants inserted in postextraction bone sites. Implant Dent. 2009. 18:270–278.
17. Terheyden H. Rekonstruktion und verzögerte Sofortrekonstruktion der Extraktionsalveole. Implantologie. 2006. 14:365–375.
18. Shakibaie MB. Socket and ridge preservation from the three-dimensional perspective - a clinical study. Z Zahnärztl Impl. 2009. 25:369–377.
19. Denissen HW, Kalk W, Veldhuis HA, van Waas MA. Anatomic consideration for preventive implantation. Int J Oral Maxillofac Implants. 1993. 8:191–196.
20. Wikesjö UM, Nilvéus R. Periodontal repair in dogs: effect of wound stabilization on healing. J Periodontol. 1990. 61:719–724.
21. Lekovic V, Kenney EB, Weinlaender M, Han T, Klokkevold P, Nedic M, Orsini M. A bone regenerative approach to alveolar ridge maintenance following tooth extraction. Report of 10 cases. J Periodontol. 1997. 68:563–570.
22. Haghighati F, Saaveh G. Essentials in Periodontal Regeneration. J Dent Tehran Uni Med Sci. 2007. 4:78–88.
23. Misch CE, Dietsh-Misch F, Misch CM. A modified socket seal surgery with composite graft approach. J Oral Implantol. 1999. 25:244–250.
24. Atwood DA, Coy WA. Clinical, cephalometric, and densitometric study of reduction of residual ridges. J Prosthet Dent. 1971. 26:280–295.
25. Dahlin C, Linde A, Gottlow J, Nyman S. Healing of bone defects by guided tissue regeneration. Plast Reconstr Surg. 1988. 81:672–676.
26. Wikesjö UM, Selvig KA, Zimmerman G, Nilvéus R. Periodontal repair in dogs: healing in experimentally created chronic periodontal defects. J Periodontol. 1991. 62:258–263.
27. Lekovic V, Kenney EB, Weinlaender M, Han T, Klokkevold P, Nedic M, Orsini M. A bone regenerative approach to alveolar ridge maintenance following tooth extraction. Report of 10 cases. J Periodontol. 1997. 68:563–570.
28. Camargo PM, Lekovic V, Weinlaender M, Klokkevold PR, Kenney EB, Dimitrijevic B, Nedic M, Jancovic S, Orsini M. Influence of bioactive glass on changes in alveolar process dimensions after exodontia. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2000. 90:581–586.
29. Artzi Z, Nemcovsky CE, Tal H. Efficacy of porous bovine bone mineral in various types of osseous deficiencies: clinical observations and literature review. Int J Periodontics Restorative Dent. 2001. 21:395–405.
30. Araújo M, Linder E, Wennström J, Lindhe J. The influence of Bio-Oss Collagen on healing of an extraction socket: an experimental study in the dog. Int J Periodontics Restorative Dent. 2008. 28:123–135.
31. Anderson HC, Cecil R, Sajdera SW. Calcification of rachitic rat cartilage in vitro by extracellular matrix vesicles. Am J Pathol. 1975. 79:237–254.
32. Wolff J. Das Gesetz der Transformation der Knochen. 1892. Berlin; Germany: Verlag von August Hirschwald.




 PDF
PDF ePub
ePub Citation
Citation Print
Print








 XML Download
XML Download