Abstract
An 18-year-old male presented severe hypodontia due to hypohidrotic ectodermal dysplasia was treated with Le Fort I maxillary osteotomy with simultaneous sinus floor augmentation using the mixture of cortical autogenous bone graft harvested from iliac crest and organic Bio-Oss to position the maxilla in a right occlusal plane with respect to the mandible, and to construct adequate bone volume at posterior maxilla allowing proper implant placement. Due to the poor bone quality at other sites, ridge augmentation with onlay graft was done to construct adequate bone volume allowing proper implant placement, using tissue harvested from the iliac bone. Seven implants were placed in the maxilla and 7 implants were inserted in the mandible and screw-retained metal ceramic FPDs were fabricated. The two year follow up data showed that dental implants should be considered as a good treatment modality for patients with ectodermal dysplasia.
Ectodermal dysplasia (ED) represents a group of inherited disorders characterized mainly by aplasia or dysplasia of tissues of ectodermal origin, namely skin, nails, hair, and teeth. ED is divided into two groups, hypohidrotic or hidrotic, based on the degree of sweat gland function.1,2 The most common condition among the ED syndromes is hypohidrotic ectodermal dysplasia (HED). HED is more severe form associated with hypodontia or anodontia, hypotrichosis (fine, sparse blond hair, including a decreased density in both eyebrows and eyelashes), and hypohidrosis or anhidrosis.2-4 Oral findings often are important and can include multiple abnormalities of the dentition (such as anodontia, hypodontia, or malformed peglike teeth), loss of occlusal vertical dimension, and protuberant lips. Also, patients with ED, because of tooth absence, have hypoplastic alveolar bone with knife-edge morphology result in bite collapse, making implant reconstruction a challenge.4-6
This article presents a case of an 18-year-old boy with an atrophic maxilla and mandible restored with dental implants. Patient underwent simultaneous orthognathic and sinus lift surgery followed by a second procedure of iliac crest bone grafting and implant placement to correct the oral and facial manifestations of the HED.
An 18-year-old male genetically diagnosed HED came to our clinic for implant rehabilitation of his edentulous maxilla and mandible. He was the only affected member in the family and his chief complaints were loose fitting denture and an unaesthetic appearance. Severe hypodontia (only one existing permanent tooth in the maxilla), dry mucosa, loss of vertical dimension, underdeveloped alveolar ridges and class III jaw relation were detected in the oral cavity (Fig. 1 and 2). Clinical and radiographic examination showed that only right maxillary second molar was present in the oral cavity. Both mandibular canines and the left mandibular first premolar were impacted. Severe maxillary and mandibular hypoplasia and mandibular prognathia were present, in addition to a loss of the vertical dimension. A CT Scan was ordered to evaluate the presence of sufficient cancellous bone volume at each potential implant position site and for site specific selection of the implants according to the surgical and prosthetic treatment plan. The residual bone height (RBH), was 8 mm at the former position of the maxillary central and lateral incisors, 7 - 8 mm of the second premolar, and 6 - 7 mm of the first molar (Fig. 3).
The patient was treated in the oral and maxillofacial center of Dey General Hospital under general anesthesia with nasotracheal intubation. The initial radiographs (panoramic and computed tomograms) and patient profile revealed severe maxillary and mandibular hypoplasia, mandibular prognathia, minimal vertical projection and bilateral large sinus cavities. Furthermore, diagnostic casts confirmed class III inter-arch relation in both sagittal and frontal planes. After mounting the diagnostic casts, anterior movements of the maxilla were evaluated in accordance with the estimated intermaxillary relation, desired occlusal plane, estimated position of the implants, and facial esthetic improvement. A written informed consent form was signed by the patient.
A Le Fort I maxillary osteotomy was performed with simultaneous sinus floor augmentation using the mixture of cortical autogenous bone graft harvested from iliac crest and organic Bio-Oss (Geistlich, Osteohealth Biomaterials, Bern, Switzerland) in a 1:1 ratio by M.B. Anterior and inferior repositioning of the maxilla was successfully attained with rigid fixation using 4 bone plate (Fig. 4). With the exception of the only emerged teeth in the oral cavity, extraction of the remaining impacted teeth was sequentially performed to prepare for future implant placement.
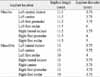
Radiographic evaluation revealed an appropriate healing with the stable bone height (22 mm) in posterior maxillary area. The bone quality at other sites was poor; therefore, ridge augmentation with onlay graft was done to construct adequate bone volume allowing proper implant placement, using tissue harvested from the iliac bone. Six month after surgery, bone plate and screw removal and dental implants insertion were performed under local anesthesia with intravenous sedation. The two-stage method was used for implant placement, providing a 12-week period between two stages. After 2 weeks, a temporary removable denture was fabricated for the patient. Seven implants (BIOMET 3i, OSSEOTITE®Implant Co., USA) were placed in the maxilla and 7 implants were inserted in the mandible, using a surgical template to assist appropriate implant placement (Fig. 5). All of the implants were placed with their neck leveled with the crestal bone. The implant insertion torque value was approximately 30 N/cm for all fixtures. The implant diameters and length were summarized in Table 1.
Diagnostic wax-up and digital imaging, were used to demonstrate the proposed functional and esthetic results that could be achieved. A diagnostic mounting and tooth-arrangement were completed for definitive evaluation of occlusal vertical dimension, interarch distance, centric relation, and the evaluation of the patient's esthetic anticipation. The patient returned to the prosthodontist immediately after completion of the surgery for delivery of temporary removable dentures, which were carefully relieved over the implant healing abutments while maintaining support for the surrounding soft tissues. Twelve weeks after insertion, implant stability was verified and final impressions were taken. Right side posterior mandibular implant was failed and removed. Definitive impression of the implants was made with a regular-viscosity polyether (Impregum F; Espe Dental, Seefeld, Germany) in a custom impression tray. Master casts (Die keen, Heraeus Kulzer Inc. Lafayette Blvd., USA) were fabricated. Despite the failure of right side posterior mandibular implant, a full maxillary bridge was fabricated, maintaining sufficient space for antagonistic implant. Ultimately, the failed implant was replaced. Abutment selection was performed on the master cast, and superstructures were fabricated according to the diagnostic set-up. On account of the poor bone quality a conventional loading protocol was applied, allowing 12 weeks before delivery of the final implant-retained restorations. During this period, provisional removable prosthesis was installed over the implants. Screw-retained metal ceramic FPDs were fabricated with an occlusal scheme that provided simultaneous contact in maximal intercuspation and group function articulation. At delivery, abutment screws and superstructure screws were tightened with controlled torque (35 and 15 N/cm2, respectively), and a clinical remount was done to refine the occlusion. The access holes were filled with a light-cured composite resin (Filtek Z250 -3M ESPE, St Paul, MN, USA). Oral hygiene instructions were provided to the patient. After tightening the retaining screws with the recommended torque, periapical radiographs were taken for the examination. One week later, the occlusion was re-adjusted and screw access holes were filled with the flowable resin.
Follow up clinical and radiographic examination performed 24 month after delivery of the final restoration. All implants were clinically stable and a successful functional implant assisted dental reconstruction was achieved according to criteria of Smith and Zarb.7 Relapse after orthognathic surgery was undetectable, and the intermaxillary relationship and facial profile were enhanced. Crestal bone resorption values were within normal ranges and no implant was lost during observation period. There was no clinical or radiographic sign of inflammation (pain, mobility, infection with suppuration, radiographic continuous peri-implant radiolucency) (Fig. 6). Periodontal and peri-implant soft tissues revealed no variations and were healthy, showing normal probing depth values. There was no sign of biting on cheeks and all of the relevant masticatory and facial muscles were relaxed and had normal tone. The implants were functionally active and competent in chewing and phonetic, as well as satisfying aesthetic concerns. The patient was fully satisfied with the functional and esthetic results and also his new found smile (Fig. 7).
The bone, a mesenchymally originated structure, is normal in patients with ED. However, the quantity of existing bone in patients with severe hypodontia is usually poor, and bone grafting procedures are usually necessary before implant placement. The main basic prerequisites for reconstruction of the edentulous maxilla and mandible are sufficient bone mass and orthoalveolar form.3,4,8 This can be obtained by augmentation of the available substrate using accepted techniques such as vertical and lateral augmentation of the alveolar ridge, sinus floor augmentation and orthognathic surgery.2,8,9
There are several reports of successful dental implant reconstruction in patients with ED. Although most of reports have addressed implant reconstruction in the severely atrophic maxilla, few have addressed reconstruction of the both maxilla and atrophic mandible.3,4,10 Further, only a few authors report the use of implants in the treatment of adult patients with ED and reports on bone augmentation are lacking.2-4,9 In our patient, the horizontal bone was poor and also the vertical bone height was unsatisfactory because of the lack of bone resulted from tooth aplasia. This led to an underdevelopment of the alveolar ridges. In our treatment plan, bilateral sinus lifts and onlay grafting in both maxilla and mandible helped to provide an adequate base for maxillary implants. In this patient, we decided to perform the orthognathic surgery and the grafting as 2 separate stages because of the concern with adequate blood supply, both to the denuded osteotomized bone that follows orthognathic surgery and to the free bone graft, which also needs good vascularization for satisfactory healing. Also, the implants were installed 6 months after the graft surgery. In spite of the fact that it makes treatment more long, this may reduce the unfavorable angulations and malpositioning of implants. In this study one implant in the site of right posterior molar was failed. It seems reasonable to assume that poor bone quality diminished vascularity were the main culprits of this issue.
It seems that obtaining a CT scan confer a number of advantages including: an aid to surgical treatment planning, identification of the ridge morphology, the ability to assess sufficient morrow space to support osseointegration, and additional bone quality.
It seems that the treatment of patients with severe hypodontia due to ectodermal dysplasia will be different according to the unique anatomic and dental status. The clinical report we have presented is a typical example of the required multidisciplinary treatment planning concepts necessary for successful rehabilitation of these patients. Further, the two year follow up data showed that dental implants should be considered as a good treatment modality for patients with ED.
Figures and Tables
Fig. 2
Pretreatment intraoral view showing disproportionate vertical dimension of occlusion, and underdeveloped alveolar ridges for implant rehabilitation.

References
1. Bergendal B. Oligodontia ectodermal dysplasia-on signs, symptoms, genetics, and outcomes of dental treatment. Swed Dent J Suppl. 2010. 205:13–78. 7–8.
2. Van Sickels JE, Raybould TP, Hicks EP. Interdisciplinary management of patients with ectodermal dysplasia. J Oral Implantol. 2010. 36:239–245.
3. Sclar AG, Kannikal J, Ferreira CF, Kaltman SI, Parker WB. Treatment planning and surgical considerations in implant therapy for patients with agenesis, oligodontia, and ectodermal dysplasia: review and case presentation. J Oral Maxillofac Surg. 2009. 67:2–12.
4. Ritto FG, Medeiros PJ, de Oliveira Mussel RL, de-Sá-Silva E. Rehabilitation of an adolescent with ectodermal dysplasia. Two-stage orthognathic, graft, and implant surgery: case report. Implant Dent. 2009. 18:311–315.
5. Yap AK, Klineberg I. Dental implants in patients with ectodermal dysplasia and tooth agenesis: a critical review of the literature. Int J Prosthodont. 2009. 22:268–276.
6. Lamazza L, Cerulli GM, Favaretti F, De Biase A. Implant-prosthetic partial-arch restoration in a patient with ectodermal dysplasia characterized by oligodontia and localized bone deficiency: a case report. Int J Oral Maxillofac Implants. 2009. 24:147–150.
7. Smith DE, Zarb GA. Criteria for success of osseointegrated endosseous implants. J Prosthet Dent. 1989. 62:567–572.
8. Lypka M, Yarmand D, Burstein J, Tso V, Yamashita DD. Dental implant reconstruction in a patient with ectodermal dysplasia using multiple bone grafting techniques. J Oral Maxillofac Surg. 2008. 66:1241–1244.
9. Stanford CM, Guckes A, Fete M, Srun S, Richter MK. Perceptions of outcomes of implant therapy in patients with ectodermal dysplasia syndromes. Int J Prosthodont. 2008. 21:195–200.
10. Peñarrocha M, García B, Martí E, Boronat A. Rehabilitation of severely atrophic maxillae with fixed implant-supported prostheses using zygomatic implants placed using the sinus slot technique: clinical report on a series of 21 patients. Int J Oral Maxillofac Implants. 2007. 22:645–650.
11. Hummel P, Guddack S. Psychosocial stress and adaptive functioning in children and adolescents suffering from hypohidrotic ectodermal dysplasia. Pediatr Dermatol. 1997. 14:180–185.
12. Chung DW, Vang MS, Park SW, Lim HP, Yang HS. Oral rehabilitation for a patient with oligodontia and maxillary hypoplasia. J Adv Prosthodont. 2009. 1:6–9.




 PDF
PDF ePub
ePub Citation
Citation Print
Print








 XML Download
XML Download