Abstract
PURPOSE
To compare the fracture resistance and the mode of failure of endodontically treated teeth restored with different post-core systems.
MATERIALS AND METHODS
Root canal treatment was performed on 40 maxillary incisors and the samples were divided into four groups of 10 each. For three experimental groups post space preparation was done and teeth were restored with cast post-core (Group B), stainless steel post with composite core (Group C) and glass fiber post with composite core using adhesive resin cement (Group D). Control group (A) samples were selected with intact coronal structure. All the samples were prepared for ideal abutment preparation. All the samples were subjected to a load of 0.5 mm/min at 130° until fracture occurred using the universal testing machine. The fracture resistance was measured and the data were analyzed statistically. The fracture above the embedded resin was considered to be favorable and the fracture below the level was considered as unfavorable. The statistical analysis of fracture resistance between different groups was carried out with t-test. For the mode of failure the statistical analysis was carried out by Kruskal-Wallis test and Chi-Square test.
RESULTS
For experimental group Vs control group the fracture resistance values showed significant differences (P<.05). For the mode of failure the chi-square value is 16.1610, which means highly significant (P=.0009) statistically.
CONCLUSION
Endodontically treated teeth without post core system showed the least fracture resistance demonstrating the need to reinforce the tooth. Stainless steel post with composite core showed the highest fracture resistance among all the experimental groups. Teeth restored with the Glass fiber post showed the most favorable fractures making them more amenable to the re-treatment.
Restoration of the mutilated endodontically treated tooth is a subject that has been evaluated and discussed widely in dental literature. The endodontically treated tooth is a unique subset of teeth requiring restoration due to the loss of the tooth structure, the changed physical characteristics by the altered collagen cross linking, the dehydration, the altered esthetic characteristics of the residual tooth and the impaired neurosensory feedback mechanism.1 Esthetic, functional and structural rehabilitation of a pulpless tooth is critically important to ensure a successful restorative outcome. In cases where most of the coronal portion is lost, a common method to restore such teeth is the use of a post and core, onto which a full crown is cemented.2 The dowel is a post or other relatively rigid, restorative material placed in the root of a non-vital tooth also retaining the core. The post functions primarily to aid the retention of the restoration and to protect the tooth by dissipating or distributing forces along the tooth. On the contrary, the tooth is weakened if dentin is sacrificed to place a large diameter dowel.3 The decision regarding post placement should be based on the amount of remaining tooth structure, anatomic position of the tooth, functional load on the tooth and esthetic requirement of the tooth. Endodontic posts can be preformed and custom made; metallic and non metallic; stiff and flexible and esthetic and non-esthetic.3 Until 1980, the cast metal post and core was considered the standard option to rebuild an endodontically treated broken tooth. Today numerous tooth colored posts are available like zirconium coated carbon fiber post, all Zirconium, Cerapost, Fiber reinforced light post and glass fiber post.1 The restoration of endodontically treated teeth with metal free, physiochemically homogenous materials that have physical properties similar to those of dentin has become a major objective in dentistry. Fiber reinforced posts were able to reduce root fracture possibility to minimum risk and displayed significantly higher survival rate.4 Glass fiber posts integrally bond to the composite core and provide a natural hue improving the esthetics without compromising much on the strength.4 Current literature provides sparse information on the comparison of post systems with different modulus of elasticity and their effects on the fracture resistance of root canal treated teeth. Thus the present study was conducted to compare the fracture resistance and the mode of failure of endodontically treated teeth restored with different post-core systems like cast post-core, stainless steel post with composite core and glass fiber post with composite core.
Forty recently extracted maxillary central incisors (without caries, cervical abrasion and fracture) were collected and examined under a stereomicroscope. Measurements of maximum buccolingual and mesiodistal dimensions at cementoenamel junction for each tooth were conducted by Vernier-caliper with 0.1 mm accuracy. The teeth were cleaned and stored in normal saline at room temperature (24 - 28℃) to prevent dehydration before and during experimental procedures. Root canal treatment was carried out on all specimens and obturation was done by lateral condensation technique using 40-size gutta-percha (Dentsply, Addlestone, Surrey, UK) as a master cone. The selected teeth were randomly assigned into four experimental groups.
Access cavities were sealed with light cure composite resin (Charisma; Heraeus Kulzer GmbH, Hanau, Germany) and a crown preparation of 8 mm from incisal edge to cervical region was made. The specimen teeth in group B, C and D were prepared by removing the crown of the teeth with a fine grit diamond wheel perpendicular to the long axis of the teeth with remaining tooth length standardized to approximately 16 mm. A shoulder of 1 mm was prepared around the full circumference of tooth with cylindrical diamond bur.
The post space preparation was done with Peeso-Reamer up to number 5 size to a depth of 10 mm under full water irrigation.5 A direct technique was used to fabricate a post core pattern with inlay wax (Harvard Blue-Wax; Richter & Hoffmann Harvard Dental-GmbH, Berlin). The core dimensions were kept the same as the dimension in Group A. The pattern was casted with Type III cast gold alloy (Dentozam-M, Sempsa, Madrid, Spain) using a lost wax technique.6 The post was then sand blasted for 3 - 4 seconds with 50 µm aluminum oxide powder and then cleaned with distilled water to improve the adhesion. The post space was treated with the chelating agent (Glyde; DeTrey GmbH O-78467 Konstang, Germany) and subsequently irrigated with 5.25% sodium hypochlorite solution to remove the smear layer. The post was cemented with the dual cure adhesive resin cement (Panavia F; Kuraray, Osaka, Japan) according to the manufacturer's recommendation.
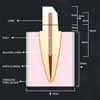
The post space preparation was done to a depth of 10 mm with a peeso-reamer number 5 matching the diameter of stainless steel post (SB post; J Mortia, USA).The post space preparation and the cementation were done similar to Group B. A light polymerizing composite core-resin material (Clearfil Photo Core; Kuraray, Tokyo, Japan) was used for core build up with 20 seconds of light curing for each increment. The dimensions of the core simulated with the crown preparation were shown in Fig. 1.
Post space preparation was done by Peeso-Reamer as in Group B specimens and then with size-matching-reamer provided by the manufacturer to a depth of 10 mm with full water irrigation. The post space preparation was done similar to Group B. The Glass fiber post (Mirafit; Hager Werken, Germany) was then applied and shortened with diamond disks to a height of 4 mm above the tooth margin namely a total post length of 14 mm. The prepared posts were sandblasted for 3 - 4 seconds and cleaned with distilled water and treatment of post space was done as in Group B specimen. The post cementation and core build up was done similar to Group C specimens.
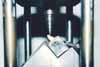
Each specimen was mounted in a Stainless steel block of size 19×19×20 mm with acrylic resin and socket was relined with a silicone rubber impression material approximately 0.25 mm thick, as described by Lovdahl et al.7 and Chan et al.8 All completed specimens were stored in normal saline at a room temperature for a period of 30 days before testing procedure. A special fixture was prepared to mount the tooth (along the long axis) at an angle of 1300 to the point of the application of the force (Fig. 2). The specimen with stainless steel block was mounted on a special fixture on a computer controlled Instron Universal Testing Machine (Model-4467, Instron Coronation Road, High Wycombe, Buckinghamshire, UK). The compressive load was applied with 1 mm diameter, ballended steel compressive head at an angle of 130° to the long axis of the tooth (Fig. 2). The force was applied by measuring in the midline of the palatal slope from a point 4 mm from the start of palatal surface, at a rate of 0.5 mm/min until visible or audible evidence of fracture or indication of inability of the specimen to withstand a greater load was shown. The force at fracture was measured in MPa and the type of fracture was recorded as Restorable (site of fracture above acrylic resin) or non-restorable (site of fracture below acrylic resin). Descriptive data were collected and analysed. The comparative evaluation of mean fracture resistance between the experimental groups was carried out with t-test. For the mode of failure the statistical analysis was done by non parametric Kruskal-Wallis test and Chi-Square test.
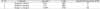
The analysis of variance was used to compare the mean differences between the groups and within the groups to evaluate fracture resistance. In all the tested samples of Group A exhibited the lowest fracture resistance while Group C exhibited highest fracture resistance among the all four groups (Table 1). For experimental group Vs control group the fracture resistance values showed significant differences (P=.0001) (Table 2). For comparative evaluation of mean fracture resistance between two experimental groups t-test was used, which was statistically non-significant for Group C vs Group D (Table 3). For the mode of failure a statistical analysis for comparing all four groups was done by non parametric Kruskal-Wallis test and proved to be statistically significant (P<.05). The chi-square value is 16.1610, which is highly significant (P=.0009) statistically. The results showed that Group D had all restorable fractures than remaining Groups (Fig. 3).
Root canal therapy utilized singly on a mutilated tooth does not save the tooth; instead, it saves the root. To restore back the strength of fractured root canal treated teeth, a post and core would serve as an ideal solution which protects the weakened tooth.2 Historically, the cast metal post and cores were the only viable and available choice.9 They relatively consume more time and fail twice as often as prefabricated metal posts and tend to cause nonsalvageable root fractures.10,11 Metallic prefabricated posts resulted in a heterogeneous combination with dentin, the stresses of which may be vital to the root.12 In the days of routine porcelain-fused to metal crowns with sub-gingival margins, core esthetics was never a concern. Today with all ceramic restorations crowns, onlays and veneers, margins are often supragingival. A metallic or dark post (Carbon fiber) or core will have a "Shine through" effect. Hence several tooth-colored posts have been developed. The use of composite core build up has paved the way to reproduce the shade and translucency of natural teeth.13
The present in vitro study was attempted to compare the fracture resistance and the mode of failure of endodontically treated teeth restored with conventional cast post core with stainless steel post with composite core and glass fiber post with composite core. Human maxillary anterior teeth are more susceptible to trauma and receive more angular forces. Hence they were selected to represent the best possible option to simulate the clinical situations.14
From the data it is observed that group A i.e. control group demonstrated the least mean fracture resistance values as compared to experimental groups. Group C recorded the highest mean fracture resistance values among experimental groups followed by Group D and Group B (Table 1). A comparative analysis of fracture resistance values between control group and experimental groups shows high statistical significance (P=.0001) which was determined by using t-test. The teeth restored with stainless steel post with composite core i.e. Group C showed significantly higher mean fracture resistance than other experimental groups when compared with control group (Table 2). However comparative analysis values among the Group C and Group D were statistically non-significant (Table 3). The results of this study are consistent with Kantor and Pines,15 Robbins1 who recommended post and core to increase the fracture resistance. The above results are also consistent with Wadhwani et al.,2 who demonstrated the highest mean fracture resistance values for stainless steel post 174 kg and mean value of 135 kg for glass fiber post. Newman et al.16 also supports this findings demonstrating highest mean fracture resistance for stainless steel post followed by glass fiber post. However these results are contrary to the findings of Lovdahl and Nicholls,7 Sorensen,17 Trope,18 Sidoli,19 and Dean20 who suggested that the use of stainless steel post for reinforcing the tooth is difficult to justify and possibly detrimental. Anusavice et al. recorded the maximum biting force of 100 - 193 Mpa (756 N).21 These forces are considerably higher in the oral cavity under physiological conditions that affect incorporated dental materials by exposing them to permanent bending stress.21,22 If we take this into consideration all experimental groups, should be clinically acceptable. The ideal post should not be evaluated on its size or rigidity but its ability to respect the root structure.9 The teeth restored with cast-post-core showed cervical and middle third root fracture making them non-restorable; whereas glass fiber post demonstrated all core fractures making the teeth amenable to retreatment. Thus the placement of post after endodontic therapy is a good policy preventing fracture of the tooth at the gingival crest. Most root fracture of unposted endodontically treated teeth occurs at the gingival level of the tooth since the root is encased in bone and others resist the forces applied to crown. The results of present study are consistent with Sirimai14 and Sidoli19 demonstrating no root fractures for fiber post i.e. restorable fractures.
Material property of the post has been shown to affect the stress distribution. It is more favorable when two substances of equivalent or almost near modulus of elasticity approximate each other. Thus considering that the modulus of elasticity for dentin i.e. 20,000 Mpa, the glass fiber post (54,000 Mpa) would be considered a more favorable post in terms of stress distribution as compared to stainless steel (220,000 Mpa). When stress is applied to the post system, a very rigid post (with high modulus of elasticity) will no longer follow the elastic deformation but will create localized stress peak inside the root, eventually leading to system failure (root fracture). Therefore from the above studies it can be concluded that the fiber post has characteristics simulating natural dentinal structure than any other previously used post and it acts as a shock-absorber, dissipating much stresses on the finished restoration with small fraction forces to dentinal walls thus demonstrating restorable fractures. The composite core has excellent adaption and forms strong bond to remaining tooth structure, bondable posts, resin cements, and ultimately the final restoration creating the monoblock. In addition it is esthetic, simple and predictable.9 The introduction of glass fiber posts and composite resin has brought a new concept of "Endoesthetics" into picture. Moreover glass fiber post is translucent and creates a monoblock, bonding every component directly or indirectly thus reinforces the intra-radicular tooth structure with excellent transverse strength.23
Limitations of the study:- 1)The study of design did not include the fabrication of cast crowns which would give a more realistic picture of in vivo performance. 2) This study may not accurately reflect the situation in vivo as the fracture resistance was determined by applying heavy load to a single point. But considering the present status, glass fiber post can be strongly recommended as it is a perfect amalgamation of physical properties like modulus of elasticity close to dentin and good fracture resistance with most coveted endoesthestics demanded by the patient. However, a further research of a large scale in this field is required before anything can be deemed ultimate for the clinical use. Additional in vitro and in vivo studies are required for the long-term results.
1) The endodontically treated teeth without post core system showed the least fracture resistance demonstrating the need to reinforce the tooth. 2) The teeth restored with stainless-steel post/composite core demonstrated the highest fracture resistance compared to the other post systems. 3) All teeth restored with glass fiber post had restorable fractures making them more amenable to retreatment; with the advantage of being excellent as far as endoesthetics is concerned.
Figures and Tables
References
1. Robbins JW. Restoration of the endodontically treated tooth. Dent Clin North Am. 2002. 46:367–384.
2. Wadhwani KK, Shrivastava S, Nigam P. Comparative evaluation of fracture resistance of various post systems: An in vitro study. J Conserv Dent. 2003. 6:56–61.
3. Galen WW, Mueller KI. Cohen S, Burns RC, editors. Restoration of the Endodontically Treated Tooth. Pathways of the Pulp. 2002. 8th ed. St. Louis: Mosby;765–796.
4. Akkayan B, Gülmez T. Resistance to fracture of endodontically treated teeth restored with different post systems. J Prosthet Dent. 2002. 87:431–437.
5. Shillingburg HT, Hobo S, Whitsett LD, Jacobi R, Brackett SE. Preparations for extensively damaged teeth. Fundamentals of fixed prosthodontics. 1997. 3rd ed. Chicago: Quintessence;181–209.
6. Martínez-Insua A, da Silva L, Rilo B, Santana U. Comparison of the fracture resistances of pulpless teeth restored with a cast post and core or carbon-fiber post with a composite core. J Prosthet Dent. 1998. 80:527–532.
7. Lovdahl PE, Nicholls JI. Pin-retained amalgam cores vs. cast-gold dowel-cores. J Prosthet Dent. 1977. 38:507–514.
8. Chan RW, Bryant RW. Post-core foundations for endodontically treated posterior teeth. J Prosthet Dent. 1982. 48:401–406.
9. Freedman GA. Esthetic post-and-core treatment. Dent Clin North Am. 2001. 45:103–116.
10. Standlee JP, Caputo AA, Collard EW, Pollack MH. Analysis of stress distribution by endodontic posts. Oral Surg Oral Med Oral Pathol. 1972. 33:952–960.
11. Torbjörner A, Karlsson S, Odman PA. Survival rate and failure characteristics for two post designs. J Prosthet Dent. 1995. 73:439–444.
12. Fredriksson M, Astbäck J, Pamenius M, Arvidson K. A retrospective study of 236 patients with teeth restored by carbon fiber-reinforced epoxy resin posts. J Prosthet Dent. 1998. 80:151–157.
13. Rosentritt M, Fürer C, Behr M, Lang R, Handel G. Comparison of in vitro fracture strength of metallic and tooth-coloured posts and cores. J Oral Rehabil. 2000. 27:595–601.
14. Sirimai S, Riis DN, Morgano SM. An in vitro study of the fracture resistance and the incidence ofvertical root fracture of pulpless teeth restored with six post-and-coresystems. J Prosthet Dent. 1999. 81:262–269.
15. Kantor ME, Pines MS. A comparative study of restorative techniques for pulpless teeth. J Prosthet Dent. 1977. 38:405–412.
16. Newman MP, Yaman P, Dennison J, Rafter M, Billy E. Fracture resistance of endodontically treated teeth restored with composite posts. J Prosthet Dent. 2003. 89:360–367.
17. Sorensen JA, Martinoff JT. Clinically significant factors in dowel design. J Prosthet Dent. 1984. 52:28–35.
18. Trope M, Maltz DO, Tronstad L. Resistance to fracture of restored endodontically treated teeth. Endod Dent Traumatol. 1985. 1:108–111.
19. Sidoli GE, King PA, Setchell DJ. An in vitro evaluation of a carbon fiber-based post and core system. J Prosthet Dent. 1997. 78:5–9.
20. Dean JP, Jeansonne BG, Sarkar N. In vitro evaluation of a carbon fiber post. J Endod. 1998. 24:807–810.
21. Anusavice KJ. Mechanical Properties of Dental Materials (Chapter 4). Phillips' Science of Dental Materials. 1996. 10th ed. Philadelphia: WB Saunders Co.;49–74.
22. Ottl P, Hahn L, Lauer HCh, Fay M. Fracture characteristics of carbon fibre, ceramic and non-palladium endodontic post systems at monotonously increasing loads. J Oral Rehabil. 2002. 29:175–183.
23. Glassman GD, Serota KS. Endoesthetics. Rehabilitation of the endodontically treated tooth. Dent Clin North Am. 1998. 42:799–811. xii




 PDF
PDF ePub
ePub Citation
Citation Print
Print





 XML Download
XML Download