Abstract
PURPOSE
Implant stability quotient (ISQ) values have been supposed to predict implant stability. However, the relationship between ISQ values and bone-to-implant contact ratio (BIC%) which is one of the predictors of implant stability is still unclear. The aim of the present study was to evaluate initial ISQ values in relation to BIC% using rabbit model.
MATERIALS AND METHODS
Four New Zealand white rabbits received a total of 16 implants in their tibia. Immediately after implant placement ISQ values were assessed. The measurements were repeated at the time of sacrifice of the rabbits after 4 weeks. Peri-implant bone regeneration was assessed histomorphometrically by measuring BIC% and bone volume to total volume values (bone volume %). The relationships between ISQ values and the histomorphometric output were assessed, and then, the osseointegration prediction model via the initial ISQ values was processed.
Under defined conditions, early and immediate loading protocols have been considered as attractive options compared with the classical 1- or 2-stage delayed loading approaches.1 Compared with delayed loading, early or immediate loadings mean not only an instant reduction in oral handicap, but also result in shorter treatment time and less service. The decision whether or not to continue with one of these treatment options at the time of implant placement is based on the assessment of implant stability. Several authors suggested that primary stability may be a useful predictor for osseointegration2,3 and that a high primary stability makes immediate loading more predictable.4 A number of methods have been introduced to assess implant stability using both invasive and non-invasive ways. Though assessment of removal torque and histologic and histomorphometric evaluation provide reliable data on the strength of the interface and the quality of implant anchorage in periimplant bone,4 these destructive measures are applicable in an experimental environment only. Clinical settings require non-destructive techniques. Non-destructive conventional methods, such as clinical evaluation through manipulation with forceps or judgment of percussion sound are highly subjective and lack the reliability. Peak insertion and removal torque values may be used,5 but torque measurements can be performed only during implant insertion. Other objective methods like Periotest (Gulden, Bensheim, Germany) or the Dental Fine Tester (Kyocera, Kyoto, Japan) have been proposed, and they can monitor implant stability over the healing period. However, their lacks of resolution, poor sensitivity and susceptibility to operator variables have been criticized.2
In recent years, Ostell™ device for resonance-frequency analysis (RFA) has been advocated to provide an objective measurement of implant primary stability and to monitor implant stability over the healing period3,6,7 and in the long term in a non destructive manner.8 This approach uses a transducer that is fixed to the implant and vibrated using a piezoceramic element with a frequency range from 5 to 15 KHz.9,10 The resulting vibration of the abutment-implant system produces a sharp increase in amplitude when the resonance frequency of the system is reached. This resonance frequency changes according to the stiffness of the excited abutment-implant system. Increasing bone anchorage of an implant would alter the resonance characteristics because of changes in stiffness of abutment-implant system in its peri-implant bone.10 Thus, changes in resonance frequency of an implant could indicate changes in anchorage of the implant and allow for conclusions on implant stability. A number of experimental and clinical studies showed increasing RFA values during healing after implant placement. These increased Implant Stability Quotient (ISQ) values were attributed to increased bone anchorage.11-13 Thus, changes in resonance frequency (RF) of an implant may possibly reflect changes in anchorage of the implant. Several factors influencing the RF of a dental implant have been proposed.14 Factors such as implant length and design, location of the first bone contact, degree of bone-to-implant contact (BIC), alveolar bone trabecular pattern, thickness of cortical bone and bone density have been investigated in different model studies, animal experiments and human studies.14-18 However, a correlation between RFA and other factors still remains conflicting and confusing.
This study attempted to verify the relationship between the ISQ values by RFA immediately after the implant placement for the future bone implant contact, BIC%.
The animal study was approved by the Institutional Animal Care and Use Committee (ASANH 200802105) in Asan Institute of Life Science and followed the routine guidelines of the Laboratory of Animal Research of Asan Medical Center (Seoul, Korea).
Threaded implants were manufactured via the machining of commercially pure titanium (Grade 4) (warentec Co., Seoul, Korea). The implants had lengths of 7.0 mm, outer diameters of 3.75 mm, and pitch-heights of 0.6 mm. The anodic oxidation treatment of the implant was performed at 300 V in an aqueous electrolytic solution of 0.02 M calcium glycerophosphate and 0.15 M calcium acetate. All procedures were performed at room temperature and a single implant anodization time was three minutes. A total of 16 implants were washed with distilled water, dried, and sterilized in ethylene oxide (EO) gas prior to animal surgery.
Four New Zealand white rabbits, each weighing 3 to 3.5 kg, were used in this study. For surgery, general anesthesia was induced through the intramuscular injection of 10 mg/kg of Zoletil (Vibac, Carros Cedex, France) and 0.15 ml/kg of Rompun (Bayer Korea, Ansan, Korea). Both rear legs of each rabbit were shaved and washed with iodine solution. Two percent lidocaine (1.0 ml) (Yu-han; 1:100,000) was administered at the tibial area. Using sterile surgical techniques, an incision was made into the skin to expose the proximal aspect of each tibia. The muscles were then dissected to allow for the elevation of the periosteum. The flat surface on the lateral aspect of the proximal tibia was selected for implant placement. Holes were drilled into the tibia with a low-speed rotary instrument under constant irrigation with sterile saline. Tapping procedures were omitted. Each rabbit had two implants inserted into each tibia, and a total of 16 implants were inserted. Muscle and fascial layers were closed in layers with Vicryl resorbable sutures (Woori Medical, Namyangju, Korea), while the skin was sutured with black silk for primary closure. Postoperatively, all animals received 50 mg/kg of Cefazolin sodium (Chong Kun Dang Pharm., Seoul, Korea) intramuscularly.19,20
Instantly after the implant placement, RFA was performed using Ostell™ Mentor (Integration Diagnostics AB, Göteborg, Sweden). The Smartpeg (Integration Diagnostics AB, Göteborg, Sweden) was attached to the fixture with the aid of a mount with 4 - 5 NCm of torque. Subsequently, the probe was held close to the peg in vertical and horizontal direction during the pulsing time (Fig. 1). After the processing time, the ISQ value was presented on the display. The measurement was repeated twice, once on the proximal side and the other on the inner side, respectively.10 Then averages were calculated to reduce measurement errors. Four weeks after the implant insertion, the ISQ values were measured twice again before the rabbits were sacrificed.
The implants and the surrounding bone were harvested en bloc and fixed in neutral buffered formalin, dehydrated in 70%, 90%, 95%, and 100% alcohol, and embedded in a light-curing resin (Technovit 7200 VLC; Kulzer, Wehrheim, Germany). An Exakt sawing machine with grinding equipment (Exakt Apparatebau, Norderstedt, Germany) was used to cut and grind sections approximately 50 um thick that were then stained with 1% toluidine blue prior to evaluation under a light microscope.21 All animals underwent histologic examination with the aid of an Olympus BX microscope (Olympus, Tokyo, Japan) connected to a computer. Image Tool Ver. 3.0 (San Antonio Dental School, University of Texas Health Science Center, USA) software was used to calculate the percentage of BIC% in whole implant surface and the bone volume % inside the thread. All the measurements were calculated under 100× magnification. A higher magnification objective and zoom were used to help determine whether or not the bone was in contact with the implant surface.
To measure the agreement for the repeated measurements of ISQ values, the root mean squared values and the intra class classification coefficient (ICC) was calculated. It showed 2.8 and 2.2 for the initial and final ISQ values, respectively. In terms of ICC, the values were 0.954 and 0.966 for the initial and final ISQ values, respectively, which indicated an excellent agreement.
Paired t tests were used to compare the difference between the initial and final ISQ values. In order to develop a BIC% prediction model, the normality assumption and equality of variance (homoscedasticity) were checked. In addition, individual rabbit's random effect was tested through random group resampling method.22 The rabbit random effect was not significant. There was no significant variation in the BIC% across the 4 rabbits in our sample. Thus, using a linear model looked sufficient. Multiple linear regression analyses were performed to determine associations between the ISQ values and the two histomorphometric values, BIC% and bone volume ratio.
The language R (R Development Core Team, 2009) was used to perform the data analysis. All values were considered significant when P<.05.
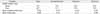
ISQ values, BIC ratio and bone volume ratio are shown in Table 1. Four weeks after the implant placement, the ISQ values were increased (P<.001) showing the average of 23.2 of the difference. However, there was no significant correlation between the initial and final ISQ values. In addition, there were no significant correlation either between the BIC% and bone volume%.
Results of the multiple regression analyses for the resultant 2 histomorphometric variables are presented in Table 2. The adjusted R2 for the ISQ values included in the regression analysis for the BIC% was 0.473. The initial ISQ values showed significant correlation with the BIC ratio and showed a positive association with the BIC%. On the contrary the final ISQ values did not show significant association on the BIC%. The bone volume% did not show any significant association with the ISQ values.
Stability both at placement and during function is an important criterion for the success of dental implant.15 Cadaver studies had shown that RFA values did correlate with the surface of BIC, and with the height of the crestal cortical bone penetrated by the implants in the oral aspects of the implant sites.16,23 On the contrary, many researchers have failed to show a correlation between the degree of implant-bone contacts and RFA measurement after healing period. Schliephake et al. could not find any correlation between BIC% and ISQ values of 80 implants in 10 foxhounds after healing periods of 1 or 3 months.17 Ito et al. presented similar results from an experiment where 24 implants placed in the tibia of four mini-pigs were analyzed with RF and histology after 1, 2 and 4 weeks.24
The present study confirmed both positive and negative results that had been reported previously about RFA value in clinical and experimental settings. The RFA values which were measured just before the rabbits were sacrificed showed no correlation with the histomorphometric parameters. At first we had expected to find more or less closer relationship between the final RFA values and the BIC%. On the contrary, the initial ISQ values showed a significant effect on the BIC% unlike the final RFA values. After looking at the raw data again, the final ISQ values showed a relatively narrower range than the initial ISQ values did. Statistically, homogeneity of an independent variable increases the variation in the regression coefficient for the output variable, making it difficult to assess the effect of the independent variable on the output variable. This is partly why the final RFA values showed the larger probability values than P>.05.
In addition, the upper portion of the rabbit tibia for experiments is composed of 1 - 2 mm thickness of cortical layer surrounding the medullary canal. It could be speculated that the differences of primary RFA value came from differences of thickness of cortical bone under same fixtures and same surgical skills. Miyamoto et al. found a strong linear correlation between resonance frequency and the thickness of cortical bone measured by computed tomography.25 However, in modern implant dentistry using moderately rough implants, the surface is often covered by a thin layer of bone, which is probably not important for the biomechanical support of implants. Hence, the final RFA values did not influence much on the BIC%.14
If some values immediately after an implant placement could predict a future retentive stability, it would provide important information to clinicians. Because of the considerable variation in the body reaction after a placement of a dental prosthetic implant, it seemed doubtful whether any single measurement for the initial stability would be suitable for predicting future BIC characteristics. This study suggested the possibility of primary stability measured by RFA using Ostell™ Mentor as a predicting factor of future osseointegration, although it had a limitation that the experiment were conducted with the rabbit tibia.
In this study, initial ISQ values measured by RFA showed significant correlation with the BIC% after 4 weeks of healing. And BIC prediction model which used ISQ values to predict future osseointegration status showed reliable results in a rabbit tibia model. Conclusively the ISQ values might be a useful clinical reference to predict the degree of osseointegration when placing an implant.
Figures and Tables
References
1. Esposito M, Grusovin MG, Willings M, Coulthard P, Worthington HV. Interventions for replacing missing teeth: different times for loading dental implants. Cochrane Database Syst Rev. 2007. 2:CD003878.
2. Meredith N. Assessment of implant stability as a prognostic determinant. Int J Prosthodont. 1998. 11:491–501.
3. Friberg B, Sennerby L, Linden B, Gröndahl K, Lekholm U. Stability measurements of one-stage Brånemark implants during healing in mandibles. A clinical resonance frequency analysis study. Int J Oral Maxillofac Surg. 1999. 28:266–272.
4. Szmukler-Moncler S, Piattelli A, Favero GA, Dubruille JH. Considerations preliminary to the application of early and immediate loading protocols in dental implantology. Clin Oral Implants Res. 2000. 11:12–25.
5. Kim SK, Heo SJ, Koak JY, Lee JH, Kwon JY. Development of predictable stability test for assessment of optimum loading time in dental implant. J Korean Acad Prosthodont. 2008. 46:628–633.
6. Rasmusson L, Kahnberg KE, Tan A. Effects of implant design and surface on bone regeneration and implant stability: an experimental study in the dog mandible. Clin Implant Dent Relat Res. 2001. 3:2–8.
7. Bischof M, Nedir R, Szmukler-Moncler S, Bernard JP, Samson J. Implant stability measurement of delayed and immediately loaded implants during healing. Clin Oral Implants Res. 2004. 15:529–539.
8. Heo SJ, Sennerby L, Odersjö M, Granström G, Tjellström A, Meredith N. Stability measurements of craniofacial implants by means of resonance frequency analysis. A clinical pilot study. J Laryngol Otol. 1998. 112:537–542.
9. Meredith N. A review of nondestructive test methods and their application to measure the stability and osseointegration of bone anchored endosseous implants. Crit Rev Biomed Eng. 1998. 26:275–291.
10. Sim CP, Lang NP. Factors influencing resonance frequency analysis assessed by Osstell mentor during implant tissue integration: I. Instrument positioning, bone structure, implant length. Clin Oral Implants Res. 2010. 21:598–604.
11. Meredith N, Book K, Friberg B, Jemt T, Sennerby L. Resonance frequency measurements of implant stability in vivo. A cross-sectional and longitudinal study of resonance frequency measurements on implants in the edentulous and partially dentate maxilla. Clin Oral Implants Res. 1997. 8:226–233.
12. Meredith N, Shagaldi F, Alleyne D, Sennerby L, Cawley P. The application of resonance frequency measurements to study the stability of titanium implants during healing in the rabbit tibia. Clin Oral Implants Res. 1997. 8:234–243.
13. Sennerby L, Persson LG, Berglundh T, Wennerberg A, Lindhe J. Implant stability during initiation and resolution of experimental periimplantitis: an experimental study in the dog. Clin Implant Dent Relat Res. 2005. 7:136–140.
14. Sennerby L, Meredith N. Implant stability measurements using resonance frequency analysis: biological and biomechanical aspects and clinical implications. Periodontol 2000. 2008. 47:51–66.
15. Meredith N, Alleyne D, Cawley P. Quantitative determination of the stability of the implant-tissue interface using resonance frequency analysis. Clin Oral Implants Res. 1996. 7:261–267.
16. Nkenke E, Hahn M, Weinzierl K, Radespiel-Tröger M, Neukam FW, Engelke K. Implant stability and histomorphometry: a correlation study in human cadavers using stepped cylinder implants. Clin Oral Implants Res. 2003. 14:601–609.
17. Schliephake H, Sewing A, Aref A. Resonance frequency measurements of implant stability in the dog mandible: experimental comparison with histomorphometric data. Int J Oral Maxillofac Surg. 2006. 35:941–946.
18. Alsaadi G, Quirynen M, Michiels K, Jacobs R, van Steenberghe D. A biomechanical assessment of the relation between the oral implant stability at insertion and subjective bone quality assessment. J Clin Periodontol. 2007. 34:359–366.
19. Lee SY, Koak JY, Heo SJ, Kim SK, Lee SJ, Nam SY. Osseointegration of anodized titanium implants coated with poly(lactide-co-glycolide)/basic fibroblast growth factor by electrospray. Int J Oral Maxillofac Implants. 2010. 25:315–320.
20. Yoon HI, Yeo IS, Yang JH. Effect of a macroscopic groove on bone response and implant stability. Clin Oral Implants Res. 2010. 21:1379–1385.
21. Donath K, Breuner G. A method for the study of undecalcified bones and teeth with attached soft tissues. The Säge-Schliff (sawing and grinding) technique. J Oral Pathol. 1982. 11:318–326.
22. Bliese P. Multilevel Modeling in R (2.3). A Brief Introduction to R, the multilevel package and the nlme package. Retrieved February 13, 2009. from http://www.R-project.org.
23. Gedrange T, Hietschold V, Mai R, Wolf P, Nicklisch M, Harzer W. An evaluation of resonance frequency analysis for the determination of the primary stability of orthodontic palatal implants. A study in human cadavers. Clin Oral Implants Res. 2005. 16:425–431.
24. Ito Y, Sato D, Yoneda S, Ito D, Kondo H, Kasugai S. Relevance of resonance frequency analysis to evaluate dental implant stability: simulation and histomorphometrical animal experiments. Clin Oral Implants Res. 2008. 19:9–14.
25. Miyamoto I, Tsuboi Y, Wada E, Suwa H, Iizuka T. Influence of cortical bone thickness and implant length on implant stability at the time of surgery-clinical, prospective, biomechanical, and imaging study. Bone. 2005. 37:776–780.




 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download