INTRODUCTION
The success of adhesive bonding of a ceramic restoration depends on a number of factors such as the ceramic system, luting agent, curing light characteristics, and surface treatments. Among those, adequate polymerization of the resin-based luting cement is one of the critical factors for the stability and clinical performance of the ceramic restoration. Adequate curing of a resin cement under a ceramic restoration is also a very important factor in obtaining adequate physical1 and biologic properties.2
Dual-cured resin cements have been developed in an attempt to combine the most desirable properties of the chemical-curing and light-curing materials, thereby providing adequate polymerization in deeper areas, reduced inhibition zone, and shorter setting time.3 Although the additional use of a chemically curing catalyst may compensate for these problems, it is also reported that the incorporation of the necessary catalyst has the potential for discoloration of the luting resin and disadvantage which causes lower bond strength in interference with some self-etching adhesives.4,5 Therefore, Calamia and Calamia6 recommended the use of a sorely light-curing luting composite resin due to certain clinical advantages.
To obtain the most out of the mechanical and chemical properties of photo-activated light or dual polymerization cements, the light should reach the porcelain subjacent cement in an intensity that is capable of polymerizing its light activation component.7 Strang et al.8 reported that dental ceramic absorbs 40% to 50% of the curing light intensity and that increased ceramic thickness requires increased exposure times beyond 30 to 40 seconds exposure for adequate resin curing. Blackman et al.9 found that the thickness of the ceramic affected the curing of luting resins because of light absorption of the ceramic.
Mechanical properties of resinous materials are dependent on the degree of conversion of the resin matrix.1 The degree of conversion can be assessed by direct and indirect methods. Direct methods such as FT-IR1,10 or laser Raman spectroscopy11 are the most sensitive techniques, but they are very time consuming and expensive.12 Economic alternatives are the indirect methods, such as depth of cure13 and microhardness testing.13,14 These indirect methods were reported to be easy to perform and demonstrated differences between different exposure situation.15 Hardness testing at various situations is the most common technique used for measuring the degree of conversion for resin cements. Rueggeberg et al.16,17 pointed out that surface hardness measurements showed results similar to those obtained with FT-IR spectroscopy.
There are many recent researches which show the relationships between porcelain thickness and light curing time and units. However the efficiency of light transmission in polymerization of different kinds of resins and resin-based cements under different thickness of ceramic restorations has not been fully investigated.14
This study was undertaken to ascertain the way in which the thickness of porcelain samples affects the completeness of cure of an underlying light cured resin based materials of uniform thickness by using the VHN to evaluate resin polymerization.
MATERIALS AND METHODS
A pressable lithium disilicate-based glass ceramic (IPS e.max MO-0 ingot, Ivoclar vivadent, Liechtenstein) was selected as for ceramic disc fabrication in this study. Four resin materials were examined in this study (Table 1). Two restorative resins (Z350: 3M ESPE Filtek™ flowable, A2 Shade, St. Paul, MN, USA; Z250: 3M ESPE Filtek™ universial, A2 Shade, St. Paul, MN, USA) and a dual cured resin cement (VL: Variolink® II ivoclar vivadent base: transparent, Liechtenstein) either with or without a self-curing catalyst (VLC: Variolink® II ivoclar vivadent catalyst: low viscosity /transparent, Liechtenstein) were used as specimens.
Light curing of the resin materials was carried out with a LED light (WBL-100 Santafe DLX LED Lamp 936 mW/cm2 S-Denti, Seoul, Korea) for 20 and 40 seconds. Power density of light-curing units was monitored using a radiometer (Cure-Rite™ Dentsply International, NY, USA).
Ceramic disc preparation
Three glass-ceramic disc specimens of 0.5 mm, 1 mm and 2 mm thickness with 10 mm diameter were fabricated according to the manufacture's instruction. In each specimen, 0.5 mm and 1 mm discs were made of framework material. In 2 mm thick disc, it was made of 1 mm framework material with layering material (IPS e.max Ceram layering glass-ceramic BL-2 shade ivoclar vivadent, Liechtenstein). The discs were trimmed with diamond burs to produce flat superior and inferior surfaces which were then polished using abrasive paper (DEER® silicon carbide water proof abrasive paper CC-1200Cw). The abrasive paper was secured to a flat bench surface and the disc moved over the abrasive paper in a circular motion under light digital pressure until a smooth flat surface was obtained, and the thicknesses of the discs were measured by digital caliper (Dial caliper D, Girrbach Dental GmbH, Durrenweg, Germany).
Resin specimen preparation
A silicone mold of 7 mm in diameter and 1 mm in height was placed on the glass slab. To ensure that each specimen of resin based material was of the same thickness (1 mm height), a metal ring (0.2 mm thick, 1 mm height) was placed in the center of the mold.
For specimen preparation, a clear glass slab on top of a black background was used as a supporting surface and to decrease the reflectivity of the underlying surface toward the specimen.
Four resin materials were filled into the silicone mold. Then, the resin materials in control group were covered with a glass microscopic slide (1 mm) to obtain a flat polymerized surface. For the resin specimens curing beneath ceramic, the ceramic disc previously described was placed on top of the thin slide glass (1 mm) to prevent adhesion of the resin materials to the disc (Fig. 1).
Curing was performed using a LED light for 20 or 40 seconds. The light outputs of the curing units were measured before each testing procedure using a radiometer. The light tips were in close contact with either the microscopic slide or ceramic disc. Using two light curing times, 4 types of resin based materials, and 3 kinds of ceramic discs provided 32 subgroups (Table 2). Each experimental and control subgroup contained 5 specimens with 4 points measured.
All specimens were stored in light-proof containers in distilled water at room temperature for 24 hours. The microhardness was measured using a microhardness tester (Model DMH-2 No.D9137 Matsuzawa Seiki, Japan) with a marker for Vicker's unit. Microhardness indentations were made on the bottom surface of each specimen. Four readings with 25 g load for 10 seconds were taken on each surface, and the average was converted into a Vicker's hardness number (VHN).
Statistical analysis
Descriptive statistics of VHNs according to three different thicknesses of upper porcelain layer including one control group and four different types of lower resin layer at two curing time points were displayed as mean and standard deviation. Considering four repeated measurements were obtained from the same specimen, a mixed-level repeated measures three-way analysis of variance (ANOVA) was used to compare mean VHNs by different thicknesses of porcelain and different types of resin, applying the mixed procedure with compound symmetry covariance structure, in the SAS statistical package version 9.13 (SAS Inc., Cary, NC, USA). Type one error level 0.05 was used in determining statistical significance.
RESULTS
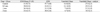
The mean VHNs for each specimen are shown in Table 3 and 4. Four VHN values from each resin specimen were measured. Although variations in the VHN values for these replicates were apparent, it was not found to be statistically significant in ANOVA (P>.05). Tukey HDS indicated significant differences in mean VHN according to porcelain thickness, resin material, and time (P<.001).
The results indicate that, for curing times of both 20 s and 40 s, the mean VHN decreased as the thickness of the overlaying porcelain increased in all resin types (Figs. 2 and 3). Z350 at control group revealed the highest values of VHN both in 20 and 40 seconds curing condition which was not significantly different with Z250 (P<.01). VHNs of resin specimens under 2 mm discs had shown the least values regardless of resin types or light curing time.
The increase in VHN of the underlying resin materials with increasing curing time of the light was again statistically significant (P<.05).
As with the light curing, the hardness of all four resin materials increased with increasing light curing time from 20 to 40 seconds. In control group, both 20 and 40 seconds of curing, the hardness of Z350 was significantly higher than VL and VLC, but not significant with Z250 (P<.01). The prolonged curing time was more influential on VL under all ceramic thicknesses which recorded the lowest values among all resin materials (P<.01).
The use of a catalyst produced significantly higher VHNs than VL groups regardless of the porcelain thickness or light curing time. A significant difference was detected between the dual-cured and light-cured cements when photopolymerized under the same ceramic disc in both 20 and 40 seconds curing (P<.05).
Both universal and flowable restorative resins (Z350 and Z250) showed significantly higher VHN values than cement materials (VL and VLC) (P<.05). However, between the two restorative resin groups (Z350 and Z250), no significant differences were detected (P<.01).
DISCUSSION
In the present study the influence of the factors (ceramic thickness, the influence of additional chemical curing, light curing time) upon the polymerization rate of resin materials was examined by determination of Vicker's microhardness.
For highly esthetic ceramic prosthesis, Magne and Belser also recommended the minimum tooth reduction depth 0.3 - 0.5 mm, and for fully coverage more than 1.5 mm preparation is needed in incisal area.18 In consideration of the anterior esthetic ceramic prosthesis, IPS e.max Press was chosen and 0.5 mm, 1.0 mm, 2.0 mm ceramic discs were fabricated which could simulate proper reduction depth.
To produce natural-looking restorations, proper thick veneer layering is inevitable. In 0.5 and 1 mm discs, measuring and building up the proper veneer ceramic was impossible. But in 2 mm disc, to simulate transparent crown third part, the 2 mm thickness consisted of a 1 mm thick framework material and 1 mm thick layering material.
After that to regulate the distance between the light tip and the surface of ceramic restoration, we used 1 mm thickness slide glass in control and experimental group so that we could control the influence of light source distance and avoid direct contact with the restorations.
In case of restorative resins (Z350 and Z250), 20 to 30 seconds of light curing was recommended and for Variolink II, 10 to 40 seconds curing time was recommended by the manufacturer. To compare the time factor, specimens were cured for 20 and 40 seconds with LED light in this study.
By far in a number of studies, the curing efficiency of halogen and LED curing units has been compared.15,19 Generally, it was found that the decisive factor which determined the degree of monomer conversion was not the source of light but the intensity of light resulting in the expected physical and mechanical properties of resin composites.13,19
From our results, statistically significant differences in VHNs light cured through ceramic discs were found between the LED exposure time 20 and 40 seconds. Therefore, it can be concluded that the curing efficiency of the LED light with a longer exposure time of 40 seconds is significantly higher than that with shorter exposure time of 20 seconds in all four resin types including dual curing resin cement. This is inconsistent with other investigations that showed the ability of high-power LED or QTH lights to reduce exposure time in curing resin-based materials.20 Nevertheless, many studies have shown that sufficient curing time would result in higher degree of conversion, polymerization depth, and hardness values.21,22
In this study, regardless of light curing time and types of resin specimens, the mean VHN decreased significantly as the thickness of the overlaying porcelain increased, which is in agreement with Koch et al. who found that the transmission of light through dental ceramic is dependent on its thickness.13 The thickness of porcelain veneer was considered as the primary factor determining the light transmittance available for polymerization.23,24 Jung et al.19 reported that dual polymerization of a resin luting agent produced greater hardness and polymerization for depths under 2 mm thick for Empress 2 ceramic restorations when compared to light polymerization alone. Hofmann et al.15 obtained similar results by using 2.5 mm-thick Empress ceramic specimens. On the other hand, Akgungor et al.25 suggested that for Empress 2 ceramic, a thickness of less than 2 mm did not affect complete polymerization of the light-polymerized resin luting agent. This controversial result could be related to the longer light exposure time of 60 seconds used in that study. Similarly, some authors20,26 suggested that a minimum 60 seconds of light exposure was necessary for adequate polymerization of the resin luting agents through ceramic or composite restorations with a thickness of less than 2 mm. In this study recommended by manufacturer light curing time 20 and 40 seconds were compared. From the results of this study, resin materials under ceramic thickness of 2 mm require additional light curing time. The research with prolonged curing time more than 40 seconds will be needed.
The use of a catalyst resulted in a higher degree of polymerization. Twenty seconds light curing with catalyst showed higher VHNs compared to 40 seconds light curing without catalyst, which emphasized the importance of the self-curing catalyst. This result is supported by El-Mowafy and Rubo3 who showed that dual-curing resin cements reached an adequate degree of conversion even in the area that was less accessible to the curing lights. VHN values of this study indicate that the catalyst is recommendable in most cases, because statistical differences were found even in the control group.
It was also demonstrated that restorative resins (Z350 and Z250) showed higher VHN values than resin cements (VL and VLC) regardless of ceramic discs and light curing times. Although many kinds of resin cements were studied throughout last few decades, no study had compared the restorative resins and the luting cements. Our results pointed out that restorative composites showed higher physical properties than luting resin cements throughout the all variable conditions.
Many kinds of commercially used restorative resin materials show high film thickness in room temperature, but a strong correlation was found between the consistency and the film thickness of the luting agents, which is supported by the temperature dependency on the film thickness.27 If the flowability of restorative resins obtaines a film thickness in room temperature, they could be considered as a luting resin cements.
In this study, the result implies that if the flow of restorative resin permits, they can be considered as luting materials which show better mechanical properties than normally used resin cements. More researches will be needed in this part.
CONCLUSION
Within the limitations of this study, the following conclusions could be drawn.
1. The decrease in VHN of the underlying resin based materials with increasing thickness of the porcelain disc was statistically significant.
2. The increase in VHN with an increase in curing time was highly significant.
3. The use of a self-curing catalyst increased the VHN which showed stronger influence than doubled light curing time.
4. Restorative composites showed significantly higher VHN values compare to resin cements.




 PDF
PDF ePub
ePub Citation
Citation Print
Print





 XML Download
XML Download