Abstract
PURPOSE
The aim of this study was to evaluate the thickness of buccal and palatal alveolar bone and buccal bony curvature below root apex in maxillary anterior teeth of Korean adults using Cone-beam CT images.
MATERIALS AND METHODS
The 3D image was reconstructed with dicom file obtained through CBCT from 20 - 39 year old Korean subjects (n = 20). The thickness of buccal and palatal plate, root diameter, the buccal bony curvature angle below root apex and the distance from root apex to the deepest point of buccal bony curvature were measured on maxillary anterior teeth area using OnDemand3D program.
RESULTS
Mean thickness of buccal plate 3 mm below CEJ was 0.68 ± 0.29 mm at central incisor, 0.76 ± 0.59 mm at lateral incisor, and 1.07 ± 0.80 mm at canine. Mean thickness of palatal plate 3 mm below CEJ was 1.53 ± 0.55 mm of central incisor, 1.18 ± 0.66 mm of lateral incisor, 1.42 ± 0.77 mm of canine. Bucco-lingual diameter 3 mm below CEJ was 5.13 ± 0.37 mm of central incisor, 4.58 ± 0.46 mm of lateral incisor, and 5.93 ± 0.47 mm of canine. Buccal bony curvature angle below root apex was 134.7 ± 17.5° at central incisor, 151.0 ± 13.9° at lateral incisor, 153.0 ± 9.5° at canine. Distance between root apex and the deepest point of buccal bony curvature of central incisor was 3.67 ± 1.28 mm at central incisor, 3.90 ± 1.51 mm at lateral incisor, and 5.13 ± 1.70 mm at canine.
CONCLUSION
Within the limitation of this study in Korean adults, the thickness of maxillary anterior buccal plate was very thin within 1mm and the thickness of palatal plate was thick, relatively. The buccal bony curvature below root apex of maxillary central incisor was higher than that of lateral incisor and canine and it seems that the buccal bony plate below root apex of central incisor is most curved.
Implant placement in anterior maxilla area is a very difficult treatment due to patient's high esthetic demands and challenging anatomy of the area.1 A prominent root position is almost always accompanied by a thin, frail buccal plate that may be damaged during tooth removal, resulting in a deformed edentulous ridge whose bone morphology would require augmentation for placing an implant in an optimal position for prosthetic restoration.2-6 Orofacial ridge anatomy including crest width and facial bone atrophy should be assessed carefully before implant placement. Based on the careful evaluation, implant placement in the ideal position would be possible. Additional surgical procedures such as soft tissue and ridge augmentation are required when bone atrophy and deficient crestal width exist in the operating area. Depending on the severity of the conditions, a simultaneous or a staged approach is selected.
Clinically sound and sophisticated radiograph techniques such as dental computerized tomography (CT) can assist in diagnosing deficiencies in the dimension. Most of previous studies assessing maxillary cortical plate thickness with medical and spiral CT technology used cadaver skulls, not live subjects, with limited sample size. Cone-beam CT (CBCT) has several advantages compared to conventional CT techniques for evaluating bone structures around teeth. It is noninvasive, has high resolution, low dose of radiation, financial advantage and allows full three dimensional characterization of alveolar bone.7
The purpose of this study is to evaluate the thickness of buccal and palatal alveolar bone and buccal bony curvature in maxillary anterior teeth of adult Korean using CBCT images. The results of this study will provide valuable guidelines for choosing proper implant fixture with regards to diameter, length and axis of surgical drilling procedure.
The study subjects were Korean adults whose CBCT images were taken at the Department of Oromaxillofacial Radiology in the Chosun University Dental Hospital. The subjects had all maxillary anterior teeth without obvious periodontal disease. Twenty subjects were selected. Their ages ranged from 20 to 39 years (26.3 ± 4.79 years, 10 males/10 females).
The skulls were imaged with CBCT (Hitachi CB Mercuray CBCT unit, Hitachi Medical, Tokyo, Japan). The CBCT was set at 110 kVp and 10 mA while acquiring a total of 512 slices in 10 sec. The images were reconstructed and analyzed using OnDemand3D (Cybermed, Seoul, Korea). The center of each tooth was measured on the sagittal and horizontal plane.
From the 3D images, five aspects of the measurements were recorded by using OnDemand3D. Distance between cementoenamel junction (CEJ) and buccal bone crest, thickness of buccal and palatal plates, root diameter, buccal bony curvature angle below root apex and distance from root apex to the deepest point of buccal bony curvature were statistically analyzed on each maxillary anterior tooth.
The distance between CEJ and buccal bone crest was measured on each maxillary anterior tooth (Fig. 1).
Four reference lines were used and all of them were perpendicular to the axis of each tooth. Line A was drawn at 3 mm below CEJ, line B was drawn at 4.5 mm below CEJ, line C was drawn at the midpoint between CEJ and root apex, and line D was drawn at root apex. The thickness of buccal and palate alveolar plates was measured at reference lines (Fig. 1).
Mesio-distal and bucco-lingual diameter of each root was measured at reference line A (Fig. 2).
Three reference points were used (P, Q, R hereafter). Reference point P is the upper most and anterior part of buccal plate, point R is the one on buccal plate which meets with reference line D, and point Q is the deepest point on the buccal bony curvature between P and R. The angle formed by the points was measured (Fig. 3).
The distance from line D to point Q was vertically measured (Fig. 4).
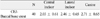
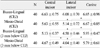
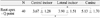
The mean distance between CEJ and buccal bone crest was 2.03±0.61 mm in central incisor, 2.46 ± 0.65 mm in lateral incisor and 2.71 ± 0.65 mm in canine. Generally, buccal bone crest of maxillary anterior teeth existed within 3 mm from CEJ (Table 1).
The mean thickness of buccal plate at each maxillary anterior tooth in reference line A (3 mm below CEJ) was 0.68 ± 0.29 mm of central incisor, 0.76 ± 0.59 mm of lateral incisor, and 1.07 ± 0.80 mm of canine.
Generally, each thickness of buccal plate in central incisor, lateral incisor and canine was very thin in reference line A and B (Table 2).
The mean thickness of palatal plate at each maxillary anterior tooth in reference line A (3 mm below CEJ) was 1.53 ± 0.55 mm of central incisor, 1.18 ± 0.66 mm of lateral incisor, and 1.42 ± 0.77 mm of canine. Each thickness of the palatal plate in central incisor, lateral incisor and canine was statistically significantly thicker than that of the buccal plate and gradually increased from line A to line D (Table 3).
At 3 mm below CEJ, the large value was showed in the diameter of the root, in order of canine, central incisor and lateral incisor (Table 4).
Buccal bony curvature angle (∠PQR) below root apex was 134.7 ± 17.5° at central incisor, 151.0 ± 13.9° at lateral incisor, 153.0 ± 9.5° at canine. The smallest value was shown in buccal bony curvature angle of maxillary central incisor, which means that central incisor is most curved (Table 5).
The distances between root apex and the deepest point (Q) of buccal bony curvature were 3.67 ± 1.28 mm at central incisor, 3.90 ± 1.51 mm at lateral incisor, and 5.13 ± 1.70 mm at canine. The distance between root apex and the deepest point (Q) of buccal bony curvature in canine was significantly larger than that of lateral and central incisor (Table 6).
Placement of implants in a correct 3-dimensional position is a key to an esthetic treatment outcome regardless of the implant system used. Long-term stability including harmonious gingival margins around implants and adjacent teeth can be guaranteed by facial bone with sufficient width and height.8,9
Generally, buccal alveolar bone crest of maxillary anterior teeth existed within 3 mm from CEJ. These results support the theory that implant head should be at least 3 mm apical to an imaginary line connecting the cementoenamel junctions (CEJs) of the adjacent teeth.10
With respect to the reference lines A, B, C and D, the thickness of buccal plate in central incisor, lateral incisor and canine was all less than 1 mm. These findings support the fact that implant platform should be placed more palatally because it can be postulated that the buccal alveolar bone plate of South Korean adult is generally very thin, within 1 mm.
It is important to place the axis of the implant corresponding to the incisal edges of the adjacent teeth or slightly palatal to this landmark.11,12 Otherwise implant can perforate the buccal alveolar plate. Kan and Rungcharassaeng13 stated that primary stability of implant is achieved by engaging the palatal wall and bone approximately 4 mm to 5 mm beyond the apex of the extraction socket. And it can be achieved by pressing the drills bodily against the palatal wall of the socket during the sequential osteotomy. Although thick labial bone plate is generally resistant to resorption and grafting is unnecessary, bone grafting is frequently done in case of thin labial bone to prevent collapse and minimize resorption regardless of the gap size.
The final implant diameter was within the confines of the tooth socket, without engaging the coronal portion of the labial plate, which is generally thin, to prevent perforation. A minimal distance of 2 mm between the implant and adjacent teeth is recommended to minimize marginal bone loss due to encroachment.13 When this is not possible, an augmentation procedure is necessary prior to or during implant placement.14,15 The suggested diameter for implants in the central incisor and canine areas is approximately 5 mm to 6 mm, and lateral incisors is approximately 3 mm to 4 mm.16,17
At 3 mm below CEJ, the diameter of the root shows a large value in order of canine (5.93 ± 0.47 mm), central incisor (5.13 ± 0.37 mm) and lateral incisor (4.58 ± 0.46 mm) in size. Therefore, wide neck implants are not recommended for the use in the anterior maxilla. Also, the narrow neck implant which is most often recommended in lateral incisor areas was recommended due to the small diameter in Korea adults. Buser et al1 suggested that the narrow neck implant with a shoulder diameter of 3.5 mm is most often used in lateral incisor areas with a minimal gap size of 5.5 mm.
In this study, buccal bony curvature angle (∠PQR) below root apex of maxillary central incisor was the smallest, and it seems that the buccal bony plate of central incisor below root apex is most curved.
Thus the long axis of the drill during surgical drilling procedure in the central incisor should be parallel to buccal alveolar plate to prevent perforation of the buccal plate. Also a tapered implant is recommended.
In case of immediate implant placement following tooth extraction, the length of implant fixture should be as long as possible for initial stability.18 In this study, the mean distance between root apex and the deepest point of buccal bony curvature was 3.67 ± 1.28 mm in central incisor, 3.90 ± 1.51 mm in lateral incisor, and 5.13 ± 1.70 mm in canine. This can be used as guidelines for selecting proper implant fixture length to prevent buccal plate perforation.
Within the limitation of this study in Korean adults, the thickness of maxillary anterior buccal plate was very thin within 1mm and the thickness of palatal plate was thick. The buccal bony curvature below root apex of maxillary central incisor was higher than that of lateral incisor and canine and it seems that the buccal bony plate below root apex of central incisor is most curved.
Figures and Tables
 | Fig. 1Reference lines and measurement of the thickness of the buccal and palatal alveolar plates of each maxillary anterior tooth. |
References
1. Buser D, Martin W, Belser UC. Optimizing esthetics for implant restorations in the anterior maxilla: anatomic and surgical considerations. Int J Oral Maxillofac Implants. 2004. 19:43–61.
2. Nevins M, Camelo M, De Paoli S, Friedland B, Schenk RK, Parma-Benfenati S, Simion M, Tinti C, Wagenberg B. A study of the fate of the buccal wall of extraction sockets of teeth with prominent roots. Int J Periodontics Restorative Dent. 2006. 26:19–29.
3. Cardaropoli G, Araújo M, Lindhe J. Dynamics of bone tissue formation in tooth extraction sites. An experimental study in dogs. J Clin Periodontol. 2003. 30:809–818.
4. Johnson K. A study of the dimensional changes occurring in the maxilla after tooth extraction. Part 2 : Closed face immediate denture treatment. Aust Dent J. 1964. 9:6–13.
5. Araújo MG, Lindhe J. Dimensional ridge alterations following tooth extraction. An experimental study in the dog. J Clin Periodontol. 2005. 32:212–218.
6. Schropp L, Wenzel A, Kostopoulos L, Karring T. Bone healing and soft tissue contour changes following single-tooth extraction: a clinical and radiographic 12-month prospective study. Int J Periodontics Restorative Dent. 2003. 23:313–323.
7. Swasty D, Lee JS, Huang JC, Maki K, Gansky SA, Hatcher D, Miller AJ. Anthropometric analysis of the human mandibular cortical bone as assessed by cone-beam computed tomography. J Oral Maxillofac Surg. 2009. 67:491–500.
8. Belser UC, Buser D, Hess D, Schmid B, Bernard JP, Lang NP. Aesthetic implant restorations in partially edentulous patientsa critical appraisal. Periodontol 2000. 1998. 17:132–150.
9. Buser D, von Arx T. Surgical procedures in partially edentulous patients with ITI implants. Clin Oral Implants Res. 2000. 11:83–100.
10. Langer B, Sullivan DY. Osseointegration: its impact on the interrelationship of periodontics and restorative dentistry. Part 3. Periodontal prosthesis redefined. Int J Periodontics Restorative Dent. 1989. 9:240–261.
11. Becker W, Sennerby L, Bedrossian E, Becker BE, Lucchini JP. Implant stability measurements for implants placed at the time of extraction: a cohort, prospective clinical trial. J Periodontol. 2005. 76:391–397.
12. London RM. The esthetic effects of implant platform selection. Compend Contin Educ Dent. 2001. 22:675–682.
13. Kan JYK, Rungcharassaeng K. Immediate placement and provisionalization of maxillary anterior single implants: a surgical and prosthodontic rational. Pract Periodontics Aesthet Dent. 2000. 12:817–824.
14. Smukler H, Castellucci F, Capri D. The role of the implant housing in obtaining aesthetics: generation of peri-implant gingivae and papillae-Part 1. Pract Proced Aesthet Dent. 2003. 15:141–149.
15. Esposito M, Ekestubbe A, Gröndahl K. Radiological evaluation of marginal bone loss at tooth surfaces facing single Brånemark implants. Clin Oral Implants Res. 1993. 4:151–157.
16. Garber DA, Salama MA, Salama H. Immediate total tooth replacement. Compend Contin Educ Dent. 2001. 22:210–216. 218
17. Saadoun AP, Le Gall MG. Periodontal implications in implant treatment planning for aesthetic results. Pract Periodontics Aesthet Dent. 1998. 10:655–664.
18. Gelb DA. Immediate implant surgery: three-year retrospective evaluation of 50 consecutive cases. Int J Oral Maxillofac Implants. 1993. 8:388–399.




 PDF
PDF ePub
ePub Citation
Citation Print
Print







 XML Download
XML Download