Abstract
PURPOSE
The aim of this study was to evaluate the periodontal and prosthodontic complications of multiple freestanding implants in the posterior jaws for up to 1 year of function.
MATERIALS AND METHODS
Eight patients received 20 implants posterior to canines. Two or more implants were consecutively inserted to each patient. Single crowns were delivered onto the implants. Marginal bone loss, implant mobility, probing depth, and screw loosening were examined to evaluate the clinical success of such restorations for maximum 1 year of functional loading.
RESULTS
All the implants performed well during the observation period. Neither periodontal nor prosthodontic complications were found except a slight porcelain chipping. While the marginal bone level was on average 0.09 mm lower around the implant after 6 months of loading, it was 0.15 mm higher after 1 year.
When two or more consecutive posterior teeth are missing, is it possible for each tooth to be separately restored by single tooth implant? Splinting multiple implants to replace consecutive teeth has been thought to help in distribution of functional loads and therefore reduce marginal bone loss.1 However, single-tooth implant restoration has shown predictable long-term results.2-4 In addition, separate single-tooth implants are advantageous in aesthetics and passive framework fit while splinted implants effectively distribute functional loads.5-7
Improvements in implant design and surface, such as frictional implant-abutment connection, microthreading, and rough surface, help to reduce marginal bone loss around the implant.8-11 Because of the improvements, single-tooth implant restoration has shown optimally maintained marginal bone levels although more harmful loads are given to the single implant.12-15 Also, the development of recommended torque and change of implant-abutment interface design have decreased the frequency of screw loosening, which was one of the major complications in single implant restoration.12,16,17 Such biomechanical advancements implying splinted restorations can be replaced with separate single-tooth implants, which are more suitable for aesthetics and passive fit.
However, there have been only a few studies reporting the clinical results in multiple single-tooth implant restorations.1,5,15 Although those studies showed excellent clinical results, the number of the studies is still insufficient. The implants used in this investigation (Inplant™, Warantec, Seoul, South Korea) also have the characteristics of microthreads, rough surface and friction connection at the implant-abutment interface that are considered adequate for separate single-tooth implant restoration. There has been no study about the clinical outcome of such restoration using these implants.
The purpose of this prospective cohort study was to evaluate the periodontal and prosthodontic complications of consecutive freestanding implants in the posterior jaws for up to 1 year of function.
This prospective study was intended for the subjects with two or more consecutively missing teeth in the posterior quadrants and planned to be restored by multiple single-tooth implant restorations. From November 2008 to March 2010, 16 volunteers received 45 implants and implants with more than 6 months of loading were selected for this investigation. This study included smokers, the patients with hypertension or diabetes mellitus who were well controlled under medication. The patients with any other systemic disease that was likely to compromise implant survival were excluded.18 The study population eventually consisted of 8 patients (3 men and 5 women) with a mean age of 45.6 years (range of 32 - 59 years) at implant placement. Their descriptive data are summarized in Table 1. Informed written consent was obtained from all subjects following approved institutional review board guidelines for clinical research.
Two or more implants were consecutively inserted to the healed sites in patients'posterior jaws. Local anesthesia was given before implant surgery. A crestal incision and a releasing vertical incision were made at the surgical site and mucoperiosteal flaps were elevated. Implants were inserted according to manufacturer's recommendation. Top of the inserted implant was at the equicrestal level and insertion torque was over 30 Ncm. The cover screw was used to cover the fixture-abutment connection part of the implant. If the threads of the implants were exposed, the exposed site was grafted with alloplast bone powder (MBCP, Biomatlante, Bretagne, France) and absorbable collagen membrane (Bio-Gide, Geistlich Pharma AG, Wolhusen, Switzerland). At the second staged surgery, the cover screws were removed and healing abutments were connected. The final impression was taken and the separate single-tooth restorations were delivered after 3 months of implant insertion. The permanent restorations were cement-retained. Every single restoration was permanently cemented (GC FujiCEM, GC Corporation, Tokyo, Japan). Metal-ceramics or zirconia-ceramics were the materials for the final restorations. The mutually protected occlusion was applied to avoid unfavorable loading.
Control visits were scheduled at 3, 6, and 12 months after prosthetic restoration for the first year. Manual pressure was applied to the implant-supported restoration to rule out the presence of mobility at each appointment. Probing depth and thread exposure were also recorded to assess the peri-implant soft tissue condition at every follow-up examination. Observed periodontal and prosthetic complications, including gingival swelling and screw loosening, were recorded at each visit.
The radiographs were taken perpendicular to the long axis of the implants with a long-cone parallel technique. The crestal bone level was measured from the fixture-abutment interface to the first visible bone-to-implant contact (BIC). The authors calculated the change in the crestal bone level using the original dimension of the inserted implants. The pitch distance between macrothreads of Inplant™ was 0.9 mm. The true crestal bone level was calculated through the proportional expression using the actual and radiographically measured values of the macrothread pitch (Fig. 1). The crestal bone level at the time of delivery of the final restoration was regarded as a baseline. The marginal bone loss was defined as the difference between the true crestal bone levels at the baseline and each appointment. It was measured at both the mesial and distal aspects of each implant.19 A single investigator performed the radiographic analysis.
From the 20 inserted implants, 45% (n = 9) were placed in the maxilla and 55% (n = 11) in the mandible. Sixty five percent (n = 13) of all the prosthetics were zirconia-ceramic crown while 35% (n = 7) of them were metal-ceramic. Fourteen implants were loaded for 6 months and rest of the implants for 1 year. The mean function period was, therefore, 7.8 months. No implant was recorded as failure during the observation period, resulting in the implant success rate of 100% after loading.
In all cases, mobility and thread exposure were not detected. One implant, which was inserted at maxillary right second molar area, showed an increase in probing depth by 2 mm without any clinical signs and symptoms. Another implant, which was inserted at maxillary left second molar area, the probing depth was decreased by 1 mm.
There were no periodontal complications reported during the observation period. No patient suffered from pain around the inserted implants. There was no screw loosening in all of the cases. A slight porcelain chipping was found on a maxillary right second molar metal ceramic crown at 6 months of loading.
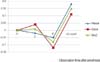
Fig. 2 shows the mean of the marginal bone loss data acquired from the radiographic evaluation and proportional expression, as mentioned above. The marginal bone around the implants was resorbed after 6 months of loading. However, a small amount of bone was gained after 1 year. The mean marginal bone loss was 0.05 mm at the mesial side of the implant, and 0.12 mm at the distal side after 6 months of loading. The mean marginal bone gain after 1 year was 0.18 mm at the mesial side, and 0.11 mm at the distal side.
The purpose of this study was to evaluate the clinical results and marginal bone changes between multiple freestanding implants in the posterior jaws functionally loaded for 6 months to 1 year. The clinical outcome of this prospective study indicates that such multiple freestanding restorations may lead to excellent results, at least in short term. Results of the present study correspond with the results of earlier study by Norton1. He evaluated marginal bone loss between multiple freestanding implants functionally loaded for up to 7.5 years in the posterior jaws, concluding that Astra Tech implant (Astra Tech AB, Mölndal, Sweden) performed extremely well in that situation. Besides, in full arch rehabilitation, potentially higher patient satisfaction with single-implant restorations was reported, compared with splinted fixed prostheses, because of the close similarity between the final restorations and the patient's prior natural dentition.21
The results of the present study in marginal bone loss were similar to those of the previous, which reported the mean marginal bone loss of the splinted implants as 0.18 mm after 1 year of loading.22 It seems that microthreaded neck of Inplant™ decreases the peak interfacial shear stress on the cortical bone and contributes to maintaining the bone level.23 However, cumulative bone level according to the observation time after loading was not typical. Another previous study showed that the majority of the bone loss occurred early in the loading period regardless of implant neck design,24 while a small amount of marginal bone gain was observed in this investigation at 1 year of loading. Such a result was hard to interpret and to ascertain what might be the cause. Further long-term follow ups are needed.
No periodontal complications were reported in this investigation. However, with respect to prosthodontic complications, there was 1 case of slight porcelain chipping. It occurred 6 months after loading on maxillary right 2nd molar region. The patient was a 60-year-old female. The implant was restored with metal-ceramic crown. The natural mandibular right second molar tooth was opposite to the restoration to make an occlusion. There was no occlusal contact on the left side of the arch due to missing of the left molars. Therefore, unilateral mastication was considered to be the contributing factor to the chipping. Another causative factor could be long clinical crown length of this restoration, which is shown to be one of the causes for porcelain fracture.24
Figures and Tables
Fig. 1
Possible distortion was accounted from the true dimension of the implant. The proportional expression to calculate the amount of marginal bone level change is shown on the upper left part of this figure (a: distance between fixture-abutment interface and the first visible bone to implant contact measured from radiograph b: pitch distance measured from radiograph x: assumed amount of real bone change, 0.9: pitch distance between macrothreads).

References
1. Norton MR. Multiple single-tooth implant restorations in the posterior jaws: maintenance of marginal bone levels with reference to the implant-abutment microgap. Int J Oral Maxillofac Implants. 2006. 21:777–784.
2. Gotfredsen K. A 5-year prospective study of single-tooth replacements supported by the Astra Tech implant: a pilot study. Clin Implant Dent Relat Res. 2004. 6:1–8.
3. Norton MR. Biologic and mechanical stability of single-tooth implants: 4- to 7-year follow-up. Clin Implant Dent Relat Res. 2001. 3:214–220.
4. Wennström JL, Ekestubbe A, Gröndahl K, Karlsson S, Lindhe J. Implant-supported single-tooth restorations: a 5-year prospective study. J Clin Periodontol. 2005. 32:567–574.
5. Solnit GS, Schneider RL. An alternative to splinting multiple implants: use of the ITI system. J Prosthodont. 1998. 7:114–119.
6. Guichet DL, Yoshinobu D, Caputo AA. Effect of splinting and interproximal contact tightness on load transfer by implant restorations. J Prosthet Dent. 2002. 87:528–535.
7. Wang TM, Leu LJ, Wang J, Lin LD. Effects of prosthesis materials and prosthesis splinting on peri-implant bone stress around implants in poor-quality bone: a numeric analysis. Int J Oral Maxillofac Implants. 2002. 17:231–237.
8. Hansson S. A conical implant-abutment interface at the level of the marginal bone improves the distribution of stresses in the supporting bone. An axisymmetric finite element analysis. Clin Oral Implants Res. 2003. 14:286–293.
9. Bozkaya D, Muftu S, Muftu A. Evaluation of load transfer characteristics of five different implants in compact bone at different load levels by finite elements analysis. J Prosthet Dent. 2004. 92:523–530.
10. Hansson S. Implant-abutment interface: biomechanical study of flat top versus conical. Clin Implant Dent Relat Res. 2000. 2:33–41.
11. Hansson S, Norton M. The relation between surface roughness and interfacial shear strength for bone-anchored implants. A mathematical model. J Biomech. 1999. 32:829–836.
12. Palmer RM, Palmer PJ, Smith BJ. A 5-year prospective study of Astra single tooth implants. Clin Oral Implants Res. 2000. 11:179–182.
13. Norton MR. The Astra Tech Single-Tooth Implant System: a report on 27 consecutively placed and restored implants. Int J Periodontics Restorative Dent. 1997. 17:574–583.
14. Puchades-Roman L, Palmer RM, Palmer PJ, Howe LC, Ide M, Wilson RF. A clinical, radiographic, and microbiologic comparison of Astra Tech and Brånemark single tooth implants. Clin Implant Dent Relat Res. 2000. 2:78–84.
15. Norton MR. Marginal bone levels at single tooth implants with a conical fixture design. The influence of surface macroand microstructure. Clin Oral Implants Res. 1998. 9:91–99.
16. Palmer RM, Smith BJ, Palmer PJ, Floyd PD. A prospective study of Astra single tooth implants. Clin Oral Implants Res. 1997. 8:173–179.
17. Henry PJ, Laney WR, Jemt T, Harris D, Krogh PH, Polizzi G, Zarb GA, Herrmann I. Osseointegrated implants for single-tooth replacement: a prospective 5-year multicenter study. Int J Oral Maxillofac Implants. 1996. 11:450–455.
18. Hwang D, Wang HL. Medical contraindications to implant therapy: part I: absolute contraindications. Implant Dent. 2006. 15:353–360.
19. Brägger U. Radiographic parameters for the evaluation of peri-implant tissues. Periodontol 2000. 1994. 4:87–97.
20. Albrektsson T, Zarb G, Worthington P, Eriksson AR. The long-term efficacy of currently used dental implants: a review and proposed criteria of success. Int J Oral Maxillofac Implants. 1986. 1:11–25.
21. Markiewicz MR, Raina A, Chuang SK, Margarone JE 3rd, Dodson TB. Full-mouth rehabilitation with single-tooth implant restorations. Overview and report of case. NY State Dent J. 2010. 76:36–42.
22. Shin YK, Han CH, Heo SJ, Kim S, Chun HJ. Radiographic evaluation of marginal bone level around implants with different neck designs after 1 year. Int J Oral Maxillofac Implants. 2006. 21:789–794.
23. Hansson S. The implant neck: smooth or provided with retention elements. A biomechanical approach. Clin Oral Implants Res. 1999. 10:394–405.
24. Scherrer SS, de Rijk WG. The effect of crown length on the fracture resistance of posterior porcelain and glass-ceramic crowns. Int J Prosthodont. 1992. 5:550–557.




 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download