Abstract
BACKGROUND
In order to restore severely attrited teeth properly, surgical intervention in the form of a crown-lengthening procedure may be required. And also, proper diagnosis and treatment sequencing is critical to obtain a successful results. Adequate diagnostic wax-up ensures good esthetics and healthy periodontal tissue.
CASE DESCRIPTION
This clinical case report describes a diagnostically based protocol for restoration on mandibular anterior teeth with crown lengthening procedure and the treatment of partially edentulous mandible combined with an edentulous maxilla. In addition, the effort to prevent the combination syndrome was described.
A short clinical crown is defined as any tooth with less than 2 mm of sound, opposing parallel walls remaining after occlusal and axial reduction. The common causes of short clinical crown include caries, erosion, tooth malformation, fracture, attrition, excessive tooth reduction, eruption disharmony, exostosis and genetic variation.1 When restoring a short clinical crown, the clinician may attempt to gain length by placing a subgingival margin. However, deep subgingival margins that encroach upon the biologic width jeopardize the periodontal tissue and are therefore not desirable.1,2 Davarpanah et al.1 and Assif et al.3 suggest the therapeutic modalities which include surgical lengthening of clinical crowns, forced eruption of teeth, altering tooth preparation design and foundation restorations. However, the short clinical crown cannot be evaluated by visual inspection alone. A thorough examination that includes clinical examination, radiographic examination, and diagnostic cast analysis is essential for successful rehabilitation of severely complicated oral dentition. Inadequate diagnosis and improper treatment plan may not ensure a satisfactory result. Visualization of the desired result is a prerequisite of successful therapy.1 Average biologic width consists of epithelial attachment (0.97 mm) plus connective tissue attachment (1.07 mm). This gives an average value of 2 mm. When this biologic width is violated by a restoration, as a defense mechanism, inflammatory response accelerates bone loss to provide space for new connective tissue attachment, which results in increased pocket depth.2 Therefore, impingement of a restoration on the biologic width will trigger loss of bone, connective tissue and epithelial attachment.
Several studies have also shown that 2 to 3 mm band of attached gingiva is preferable to maintain the restored tooth successfully. Since the resecting nature of this procedure, there is a risk of reducing the width of attached gingiva. For this reason, it is important to diagnose and evaluate the attached gingiva when planning surgical crown lengthening procedure.2
In company with the short clinical crown length, the probability of the combination syndrome was also anticipated in this case. A patient wearing a maxillary complete denture opposed by mandibular anterior teeth and a distal extension removable partial denture can easily show the combination syndrome, which was coined by Kelly.4 He described following five characteristic changes: loss of bone from the anterior part of the maxillary ridge, overgrowth of maxillary tuberosity, papillary hyperplasia, extrusion of the lower anterior teeth, and bone loss under the partial denture bases. The anterior part of the maxilla is the weakest part to resist stress and when the mandibular anterior teeth occlude anterior to the basal support, trauma is inevitable.4,5 In addition, according to Palmqvist et al.6, loss of established posterior occlusal contacts can be attributed not only to bone resorption under mandibular distal extension bases, but also to wear of the artificial denture teeth as well as changes in position of the anterior mandibular teeth. Such changes in occlusion facilitate the clenching activity and thereby increase the pressure on the maxillary anterior alveolar bone. Kelly4 discussed various possibilities to avoid combination syndrome, including the use of the roots of anterior mandibular teeth and endodontic implant to support the overdenture.
This clinical report demonstrates the treatment sequence including the determination of the required length of crown and visualization of desired results through diagnostic wax up and thorough examinations. In addition, the effort to prevent the combination syndrome was also described.
In this case, 66 year old woman patient visited the clinic complaining of discomfort of the dentures.
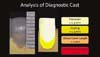
She had undergone a heart valve surgery twice in 1968 and 1998 and was under warfarin medication. Following problem lists were detected. The mandibular anterior teeth showed extremely short clinical crown length. The reverse compensating curve of the old prostheses, overgrowth of mandibular symphysis area, and bone resorption of mandibular posterior region were observed. The possibility of combination syndrome was anticipated due to the recent extraction of maxillary anterior teeth (Fig. 1 and 2). As Davarpanah et al.1 suggested, a thorough examination was performed. In radiographic examination, any periapical radiolucency was not detected even though the dentin was exposed to oral cavity. The periodontal ligament was within normal limit. The crown-to-root ratio was about 1:3. In clinical examination, attached gingival band was 4 to 5 mm width, and periodontal pocket depth was 3 mm or less. Neither periodontal problem nor tooth mobility was detected. On the properly mounted diagnostic cast examination, the imaginary line from retromolar pad 2/3 point to mandibular premolar tip was drawn. The distance between the imaginary line and the mandibular incisor's tip was 4 to 5 mm. The clinical crown was 2 mm height. According to Ash and Nelson7, the diagnostic wax up was undertaken to allow the crown to be 9 mm length. Supposing the height of coping, porcelain and the amount of subgingival margin position were 1.5 mm, 2.5 mm and 1 mm respectively, the required additional crown length was calculated as 2 mm (Fig. 3 and 4).
Based on the examination as mentioned above, the treatment plan was established. The mandibular anterior teeth were planned to have a surgical crown lengthening procedure of 2 mm extension as determined by diagnostic wax-up. Complete denture for maxilla and removable partial denture with linguoplate for mandible were planned. As mentioned by Langer et al.8, linguoplate was planned to prohibit the extrusion of mandibular anterior teeth and minimize the force upon the premaxilla. Mandibular anterior teeth were planned to be fabricated as single crowns. Bilateral balanced occlusion scheme was applied to the distal extension of the mandibular removable partial denture. The patient was suggested the implant installation at the second molar area to supplement the support of denture, but she denied the suggestion on account of economic problem.
The patient was referred to the department of periodontology for surgical crown lengthening procedure, and visited our department 2 months after operation. The planned amount of crown length was gained enough (Fig. 5). The walls of the anterior teeth were prepared as parallel as possible. The individual trays were fabricated. One sheet of baseplate wax (Dae-dong industry, Daegu, Korea) was covered for relief and tray resin (Quicky, Nissin Dental Products Inc., Kyoto, Japan) was adapted to the cast. By using the individual trays, functional impressions were registered both in maxilla and in mandible. Maxillary wax rim was fabricated as a general method. The vertical dimension of the patient and the amount of anterior exposure were maintained equal to previous old denture. Mandibular recording base and wax rim were fabricated, and then the resin cap made of DuraLay resin (Reliance Dental Mfg. Co., Worth, IL, USA) was attached to the recording base for stabilization during interocclusal registration, as described by Chang et al.9 (Fig. 6). Facebow transfer was followed by mandibular teeth wax up, coping fabrication and porcelain-fused-to-gold crown fabrication. After the mandibular anterior teeth were delivered to the patient, mandibular functional impression was taken. Framework and wax rim were fabricated as a general method. Interocclusal record was taken again, and artificial teeth were arranged to have a scheme of bilateral balanced occlusion. The definitive denture was delivered to the patient without any problem (Fig. 7). Implant placement was recommended again, but the patient hesitated over for economic problem. However, she had agreed to recall check for every six months. After 4 months, on the recall check, the gingiva and periodontum were healthy (Fig. 8). She had been satisfied with the prostheses for esthetic and functional aspects.
The complications with the short clinical crown demand a circumspect treatment plan and proper sequencing of therapy to ensure an optimal result for both the patient and the clinician. Proper treatment sequencing is critical when a patient requires multiple fixed restorations in conjunction with a removable partial and complete denture. The vertical dimension, centric relation, and occlusal plane must be determined first, followed by a diagnostic wax up which is essential for fixed prosthesis. An accurate diagnostic and interdisciplinary approach is necessary for obtaining improved, conservative and predictable results in esthetically compromised areas, such as the anterior mandibular dentition. Periodontal health is of paramount importance for all teeth, both sound and restored. Thus, this procedure, as an adjunct to a restorative treatment, can produce predictable results, while ensuring good esthetics and maintaining periodontal health.
As Langer et al.8 emphasized the importance of the posterior support in conjunction with the combination syndrome, the treatment plan should be designed to provide posterior occlusal support and to minimize occlusal pressure in the anterior maxilla. Hence, the level of the incisal edges of the mandibular anterior teeth should be assessed in comparison of the proposed posterior occlusal plane. The mandibular removable partial denture should be supported anteriorly by cingulum rest with a linguoplate as the major connector. The linguoplate delays the overeruption of the mandibular teeth, and also facilitates accurate positioning the removable partial denture during relining procedures. Posteriorly, maximum support is obtained by extending the denture base. Maximum occlusal support posteriorly with no contact anteriorly in centric occlusion and a balanced articulation in eccentric movements further reduce pressure on the anterior maxillary ridge. Posterior occlusal contact must be maintained by constant relining of the distal extension denture base to compensate for its resorption. Every effort should be made to avoid the potentially destructive occlusal forces exerted on the anterior maxillary residual ridge.
In conclusion, proper treatment plan should be established before clinical procedures. With the aim of it, a thorough examination including clinical examination, radiographic assessment and diagnostic wax up are essential. In this case report, visualization of the desired results has guaranteed the outstanding surgical and prosthodontic outcomes. In addition, the treatment modality was determined by the apparent potential to develop the combination syndrome, and every effort was exerted on fabricating properly designed removable partial denture that distributes occlusal forces evenly.
Figures and Tables
References
1. Davarpanah M, Jansen CE, Vidjak FM, Etienne D, Kebir M, Martinez H. Restorative and periodontal considerations of short clinical crowns. Int J Periodontics Restorative Dent. 1998. 18:424–433.
2. Yeh S, Andreana S. Crown lengthening: basic principles, indications, techniques and clinical case reports. N Y State Dent J. 2004. 70:30–36.
3. Assif D, Pilo R, Marshak B. Restoring teeth following crown lengthening procedures. J Prosthet Dent. 1991. 65:62–64.
4. Kelly E. Changes caused by a mandibular removable partial denture opposing a maxillary complete denture. J Prosthet Dent. 1972. 27:140–150.
5. Kwon KR, Kim YS, Kim CH, Kim HJ, Moon HS, Park SW, Park CJ, Song KY, Lee JS, Lee CH, Lim YJ, Chung MK, Jeong JH, Jeong CM, Cho IH, Cho HW, Choi DG, Han JH. Prosthodontic treatment for edentulous patients. 2007. 1st ed. Seoul: Shinhung international;426–428.
6. Palmqvist S, Carlsson GE, Owall B. The combination syndrome: a literature review. J Prosthet Dent. 2003. 90:270–275.
7. Ash M, Nelson S. Wheeler's Dental Anatomy. Physiology and Occlusion. 2003. 8th ed. Philadelphia: Saunders;230–238.
8. Langer Y, Laufer BZ, Cardash HS. Modalities of treatment for the combination syndrome. J Prosthodont. 1995. 4:76–81.
9. Chang IT, Heo SJ, Koak JY, Lee SB, Lee HY, Han DH, Hwang SH, Kye KS, Cho SA, Lim JS, Vang MS, Park HO, Park JM, Jin TH, Shin SY, Cho LR. Textbook of removable partial denture. 2004. 1st ed. Seoul: Jeesung Publishing Co.;373–382.




 PDF
PDF ePub
ePub Citation
Citation Print
Print









 XML Download
XML Download