Abstract
PURPOSE
The aim of this study was to investigate a comparison of implant bone bed preparation with Er,Cr:YSGG laser and conventional drills on the relationship between implant stability quotient (ISQ) values and implant insertion variables.
MATERIALS AND METHODS
Forty implants were inserted into two different types of pig rib bone. One group was prepared with conventional drills and a total of 20 implants were inserted into type I and type II bone. The other group was prepared with a Er,Cr:YSGG laser and a total of 20 implants were inserted into type I and type II bone. ISQ, maximum insertion torque, angular momentum, and insertion torque energy values were measured.
RESULTS
The mean values for variables were significantly higher in type I bone than in type II bone (P < .01). In type I bone, the ISQ values in the drill group were significantly higher than in the laser group (P < .05). In type II bone, the ISQ values in the laser group were significantly higher than in the drill group (P < .01). In both type I and type II bone, the maximum insertion torque, total energy, and total angular momentum values between the drill and laser groups did not differ significantly (P ≥ .05). The ISQ values were correlated with maximum insertion torque (P < .01, r = .731), total energy (P < .01, r = .696), and angular momentum (P < .01, r = .696).
The replacement of missing teeth by means of endosseous titanium implants has proven to be a successful treatment modality for edentulous patients. The achievement and maintenance of primary implant stability are prerequisites to achieve osseointegration and long-term positive outcomes of osseointegrated implants.1,2 Implant stability has been suggested to be a useful predictor of osseointegration.3,4 The creation and application of a simple, clinically applicable noninvasive test to assess implant stability is highly desirable. Suggested methods include percussion, radiography, resonance frequency analysis, placement resistance, periotesting, reverse torque, and vibration methods in sonic and ultrasonic ranges.5
A clinical instrument was recently developed to analyze resonance frequency, which is then calculated into the implant stability quotient (ISQ) to represent bone-implant contact.4,6-9 ISQ replaces hertz, which is dependent on the transducer used, and ranges from 1 to 100 with 100 representing the highest degree of stability.9 ISQ levels for successfully integrated implants are reported to range from 57 to 82. Friberg et al.4 reported that the highest correlations were found between mean torque values of the upper crestal portion of the implant and the resonance frequency values at implant placement. There were also correlations between the cutting resistances and ISQ values of the implants. O'Sullivan et al.10 reported that there were correlations between the peak insertion torques and ISQ values of the implants, but Cunha et al.11 reported that correlations between the insertion torque and ISQ values were only observed in some implant designs. As a result, controversy still remains regarding the actual relationships of ISQ values to other variables. Therefore, a new method was developed to assess implant stability by calculating energy and angular momentum values during implant installation.12,13 The energy value represents the energy absorbed by bone during implant surgery, while the angular momentum value represents the load placed on the implant during implant insertion.
Ever since the effects of ruby laser irradiation on dental hard tissues were first reported in 1964,14 a variety of lasers have been employed in dentistry, including ruby, CO2, Nd:YAG, and Er:YAG lasers. The mechanisms of laser ablation in bones and dental hard tissues are documented for specific wavelengths and modes of certain lasers.14-16 However, only the erbium family of lasers produces wavelengths that are highly absorbed by hydroxyapatite and collagen and therefore clinically effective for use on hard tissue.17 In particular, the maximum absorption of laser energy in teeth occurs between wavelengths of 3 µm and 10 µm.17,18 The most recently developed laser is erbium, chromium: yttrium-scandium-gallium-garnet (Er,Cr:YSGG) with a wavelength of 2.78 µm. Many studies have revealed advantages of the erbium laser bone ablation method. Erbium laser ablation produces clear cuts that are as efficient as drilling.19-22
Although there have been several studies on the effectiveness of bone cutting with Er,Cr:YSGG lasers, few studies have investigated the effect of the laser on primary implant stability. Therefore, the objective of the present study was to investigate the effects of preparation with Er,Cr:YSGG laser and conventional drills on the relationships between implant stability quotient (ISQ) values and implant insertion variables.
A total of 40 straight implants measuring 4.1 × 8.5 mm (Oneplant, Warantec, Seoul, Korea) were used in this study. Two different types of pig rib bone were used in this experiment. Type I bone was retrieved from the distal aspect of the pig rib, and contained more cortical bone. Type II bone came from a more proximal region of the rib with less cortical component and higher bone marrow and spongeous trabeculae content. In order to standardize type I bone, the upper cortical region was ground until the spongy region was 3.5 mm in width, and the total width of the bone was greater than 6 mm. Using the same methods, the upper cortical region of type II bone was ground until the spongy region was greater than 6 mm. The bones were firmly attached to a base device. A total of 20 implants were inserted into each type of bone.
An Er,Cr:YSGG laser (Waterlase MD:BIOLASE, Irvine, CA, USA) was used at a 5.25 W power setting and 25 Hz/sec pulse repetition with 55% water and 65% air spray (calculated energy: 200 mj/pulse). Irradiation was performed with a sapphire tip (8.5 mm, 0.6 mmΦ, MG6; BIOLASE) in noncontact and focusing modes. During laser irradiation, the tip was maintained in a vertical orientation lightly touching the samples. For each type of bone, one was drilling group by conventional drill and the other was laser group prepared by an Er,Cr:YSGG laser . In the drilling group, it was followed protocols provided by the implant company (Oneplant, Warantec, Seoul, Korea). A point drill speed of 2,000 rpm was used to penetrate the bone and make the initial mark for the implant location. Twist drills that were 2 mm wide and 8.5 mm long, pilot drills 2 to 3 mm wide, and twist drills 3 mm wide and 8.5 mm long were used. In the laser group, in order to control the size and the shape of the implant bed, a special resin stent was fabricated (Fig. 1), with a 3 mm diameter round hole created with the Er,Cr:YSGG laser device.
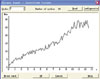
The implants were inserted with ELCOMED (W&H Dentalwerk, Bürmoos Gmbh, Austria), a machine developed for the perforation of bone and implant placement, at a calibrated torque of 50 Ncm at 20 rpm. ELCOMED enables the measurement of insertion torque during implant placement. Maximum insertion torque value is the peak insertion torque value that is reached at the final stage of implant insertion (Fig. 2).
Implant stability was measured with a resonance frequency analyzer (RFA) (Osstell Mentor; Integration Diagnostics AB., Götenborg, Sweden) at the time of implant placement. All measurements were made by the same dentist. The RFA device (Smartpeg; Integration Diagnostics AB., Gemlestadsvägen, Sweden) was placed by hand and tightened with a force of 5 - 10 Ncm onto the implant fixture. ISQ values were measured twice in parallel and perpendicular orientations to the bone.
New software programs were written to calculate the energy and angular momentum of implant installation in Java entitled "Software for the Measurement of Load Associated with Implant Installation" and "Software for the Measurement of Energy Absorbed by Bone."12,13 The writing of both software programs required special permission from the Industrial Property Office of South Korea. The calculation methods are as follows: first, the data of insertion torque are acquired from ELCOMED and entered into the programs. Then, the program automatically calculates the angular momentum and energy that developed during surgery.
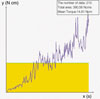
Torque can be thought of as "rotational force" or "angular force" that causes a change in rotational motion. This force is defined as linear force multiplied by a radius. The SI unit for torque is the Newton meter (Nm). Momentum (SI unit kg·m/s, or, equivalently, N·s) is the product of the mass and velocity of an object. In general, the momentum of an object can be conceptually thought of as how difficult it is to stop the object. Momentum is a conserved quantity, meaning that the total momentum of any closed system cannot be changed. The angular momentum of a particle about the origin is defined as L = r * p (L: angular momentum of the particle, r: the position of the particle expressed as a displacement vector from the origin, p: linear momentum of the particle). As seen from the definition, the derived SI units of angular momentum are Newton·meter·seconds (N·m·s or kgm2s-1). If a system consists of several particles, the total angular momentum about the origin can be obtained by adding (or integrating) all the angular momentums of the constituent particles (Fig. 3).
Energy (J) is roughly force times distance, but more precisely, it is E=∫F ds. This states that the energy (E) is equal to the integral (along a certain path) of the force. Since energy is strictly conserved and is also locally conserved, it is important to remember that the definition of energy and the transfer of energy between the "system" and adjacent regions is work: ΔE = W+Q (ΔE: amount of energy transferred, W: work done on the system, Q: the heat flow into the system). The energy required to insert an implant was determined by plotting the insertion torque against the angular displacement of the implant in radians.23 The energy values were assessed by plotting an insertion torque graph into the second program. The total energy and energy for each region was determined.
The SAS package version 9.1.3 (SAS Institute, Cary, NC, USA) was used for statistical analyses. The Kolmogorov-Smirnov test was used to assess the normality of the data. To compare the values of variables in type I and type II bone, and to compare the values of variables in type I bone and type II bone both in the laser group and drill group, independent t-tests were conducted. Finally, the influence of each parameter on ISQ values was analyzed by a Pearson correlation analysis. The Pearson correlation coefficients were calculated to assess the effects of ISQ values on maximum insertion torque, angular momentum, and energy values. The significance level was set at 5%.
The results of the Kolmogorov-Smirnov test indicated that the data rows were normally distributed. Two-way analyses of variance (ANOVA) demonstrated no evidence of interaction between bone and surgical method.
No identifiable signs of side effects such as burning or carbonization were observed during surgical procedures. Table 1 shows the comparisons of t-values for the ISQ, maximum insertion torque, total energy, and total angular momentum values in type I and type II bone. The mean values for all variables in type I and type II bone differed significantly (P < .01). All values were higher in type I bone than type II bone.
Table 2 shows the comparison of the t-values for the ISQ, maximum insertion torque, total energy, and total angular momentum values between the drill and laser groups in type I bone. The ISQ values were significantly higher in the drill group than the laser group (P < .05). The maximum insertion torque, total energy, and total angular momentum values did not differ significantly between the drill and laser groups (P > .05). Table 3 shows the comparison of the t-values for the ISQ, maximum insertion torque, total energy, and total angular momentum values between the drill and laser groups in type II bone. The ISQ values in the laser group were significantly higher than in the drill group (P < .01). The maximum insertion torque, total energy, and total angular momentum values did not differ significantly between the drill and laser groups (P ≥ .05).
Table 4 illustrates correlations between ISQ and maximum insertion torque values at implant insertion (P < .01, r = 0.731), between ISQ and total energy values (P < .01, r = 0.696), and between ISQ and angular momentum values (P < .01, r = 0.696).
It is apparent that primary stability is essential for the success and longevity of osseointegrated implants.3,10 Sennerby et al.24 have shown the importance of engaging cortical bone to implant stability and found that implants that were connected to the cortical bone by only a few threads still had greater initial holding power than implants that were completely surrounded by cancellous bone.24,25 Three parameters govern the achievement of primary stability: implant geometry, type of surgical procedure, and bone quality of the recipient site (density and stiffness).26 The mean values for all variables in type I and type II bone differed significantly (P < .01). All values were higher in type I bone than in type II bone.
In Table 4, a direct correlation can be seen between the ISQ and maximum insertion torque values (P < .01, r = 0.731). This corresponds with the results of Friberg et al.,6 who measured bone density in the marginal, middle, and apical parts of implants in the maxilla. Subsequent RFA measurements showed a correlation between implant stability and the density of the marginal bone, but the same correlation was not seen at any other parts of the implant site. As a result, Friberg et al. concluded that marginal bone properties were the main determinants of RFA measurements. ISQ values were also correlated to angular momentum (P < .01, r = 0.696) and energy values (P < .01, r = 0.696) at implant insertion. After implant insertion, bone has been observed to undergo remodeling at the implant-bone interface in in vivo studies. If high trauma was delivered to the implant-bone site, stress to the bone would increase. Bone remodeling at this interface between the bone and implant would then be delayed. Therefore, it is best to decrease stress to the bone. Stress can be thought of as energy applied to the bone. A new software program was written to calculate energy using insertion torque data.13 This energy is related to the load in the bone. In general, the energy can be divided into mechanical load and heat to the bone. Since energy is also lost in the generation of heat within the hand piece, in the generation of noise, and in the friction between the components of the hand piece and motor,27 the total energy calculated by insertion torque may be an overestimate of the energy imparted to the bone. Nonetheless, if the energy is excessive, the bone will exhibit slow healing or necrosis. With our new software program, the stress on the bone and the amount of bone remodeling that occurs can be approximated. Insights drawn from new methods and software programs might result in new implants that demonstrate higher implant stability and lower damage to bone during surgery.
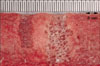
In Fig. 4, which shows the comparison of the preparation site with drills (left) and lasers (right) group, a wide gap, especially in the apical area of the implant supporting area, was observed. Although the sizes of the cavities up to 3 mm in diameter were adjusted by stents, the actual sizes of the cavities were unknown in laser group. This means that in comparing the cavities prepared with convention drills, the laser preparation resulted in a wider gap between the implant surface and the lateral wall of the bony cavity. This phenomenon was also reported by other studies28,29 with the Er:YAG laser. Schwarts et al.29 prepared implant channels in the lower jaws of beagle dogs using an Er:YAG laser device and conventional drills. Three screw-type titanium implants from different manufacturers were randomly inserted. Histological and histomorphometric analysis was conducted during the second and twelfth week of recovery. In the two week specimen, it was found that Er:YAG laser osteotomy frequently resulted in wide peri-implant gaps, particularly in the apical area of the implant supporting bone, caused by the mode of application.
One interesting finding in our study is that in the laser group, we found wider peri-impant gaps just after the operation (Fig. 4). Ultimately, the wider peri-implant gap, maximum insertion torque, total energy, and total angular momentum values between the drill and laser groups did not differ significantly in type I and type II bone. For future purposes, in vivo studies of bone response after the insertion of titanium implants in sites prepared with Er,Cr:YSGG lasers and in sites prepared with conventional drills are needed.
Within the limitations of this study, the effects of preparation with Er,Cr:YSGG laser on the relationship between implant stability quotient (ISQ) values and implant insertion variables were comparable to those observed in drilling sites. Our new Java program can be used to ascertain the energy produced with implant placement, which can be used in combination with resonance frequency analysis to predict implant stability.
Figures and Tables
References
1. Adell R, Lekholm U, Rockler B, Brånemark PI. A 15-year study of osseointegrated implants in the treatment of the edentulous jaw. Int J Oral Surg. 1981. 10:387–416.
2. Albrektsson T, Brånemark PI, Hansson HA, Lindström J. Osseointegrated titanium implants. Requirements for ensuring a long-lasting, direct bone-to-implant anchorage in man. Acta Orthop Scand. 1981. 52:155–170.
3. Meredith N. Assessment of implant stability as a prognostic determinant. Int J Prosthodont. 1998. 11:491–501.
4. Friberg B, Sennerby L, Linden B, Gröndahl K, Lekholm U. Stability measurements of one-stage Brånemark implants during healing in mandibles. A clinical resonance frequency analysis study. Int J Oral Maxillofac Surg. 1999. 28:266–272.
5. Meredith N. A review of nondestructive test methods and their application to measure the stability and osseointegration of bone anchored endosseous implants. Crit Rev Biomed Eng. 1998. 26:275–291.
6. Friberg B, Sennerby L, Meredith N, Lekholm U. A comparison between cutting torque and resonance frequency measurements of maxillary implants. A 20-month clinical study. Int J Oral Maxillofac Surg. 1999. 28:297–303.
7. Meredith N, Book K, Friberg B, Jemt T, Sennerby L. Resonance frequency measurements of implant stability in vivo. A cross-sectional and longitudinal study of resonance frequency measurements on implants in the edentulous and partially dentate maxilla. Clin Oral Implants Res. 1997. 8:226–233.
8. Meredith N, Alleyne D, Cawley P. Quantitative determination of the stability of the implant-tissue interface using resonance frequency analysis. Clin Oral Implants Res. 1996. 7:261–267.
9. Barewal RM, Oates TW, Meredith N, Cochran DL. Resonance frequency measurement of implant stability in vivo on implants with a sandblasted and acid-etched surface. Int J Oral Maxillofac Implants. 2003. 18:641–651.
10. O'Sullivan D, Sennerby L, Meredith N. Measurements comparing the initial stability of five designs of dental implants: a human cadaver study. Clin Implant Dent Relat Res. 2000. 2:85–92.
11. da Cunha HA, Francischone CE, Filho HN, de Oliveira RC. A comparison between cutting torque and resonance frequency in the assessment of primary stability and final torque capacity of standard and TiUnite single-tooth implants under immediate loading. Int J Oral Maxillofac Implants. 2004. 19:578–585.
12. Kim SH, Lee SJ, Cho IS, Kim SK, Kim TW. Rotational resistance of surface-treated mini-implants. Angle Orthod. 2009. 79:899–907.
13. Kim SK, Heo SJ, Koak JY, Lee JH. Development of predictable stability test for assessment of optimum loading time in dental implant. J Korean Acad Prosthodont. 2008. 46:628–633.
14. Li ZZ, Reinisch L, Van de Merwe WP. Bone ablation with Er:YAG and CO2 laser: study of thermal and acoustic effects. Lasers Surg Med. 1992. 12:79–85.
15. Buchelt M, Kutschera HP, Katterschafka T, Kiss H, Lang S, Beer R, Losert U. Erb:YAG and Hol:YAG laser osteotomy: the effect of laser ablation on bone healing. Lasers Surg Med. 1994. 15:373–381.
16. Friesen LR, Cobb CM, Rapley JW, Forgas-Brockman L, Spencer P. Laser irradiation of bone: II. Healing response following treatment by CO2 and Nd:YAG lasers. J Periodontol. 1999. 70:75–83.
17. Walsh LJ. The current status of laser applications in dentistry. Aust Dent J. 2003. 48:146–155.
18. Featherstone JD. Caries detection and prevention with laser energy. Dent Clin North Am. 2000. 44:955–969.
19. Eversole LR, Rizoiu IM. Preliminary investigations on the utility of an erbium, chromium YSGG laser. J Calif Dent Assoc. 1995. 23:41–47.
20. Kimura Y, Yu DG, Fujita A, Yamashita A, Murakami Y, Matsumoto K. Effects of erbium,chromium:YSGG laser irradiation on canine mandibular bone. J Periodontol. 2001. 72:1178–1182.
21. Wang X, Ishizaki NT, Suzuki N, Kimura Y, Matsumoto K. Morphological changes of bovine mandibular bone irradiated by Er,Cr:YSGG laser: an in vitro study. J Clin Laser Med Surg. 2002. 20:245–250.
22. Wang X, Zhang C, Matsumoto K. In vivo study of the healing processes that occur in the jaws of rabbits following perforation by an Er,Cr:YSGG laser. Lasers Med Sci. 2005. 20:21–27.
23. Lewandrowski KU, Lorente C, Schomacker KT, Flotte TJ, Wilkes JW, Deutsch TF. Use of the Er:YAG laser for improved plating in maxillofacial surgery: comparison of bone healing in laser and drill osteotomies. Lasers Surg Med. 1996. 19:40–45.
24. Sennerby L, Thomsen P, Ericson LE. A morphometric and biomechanic comparison of titanium implants inserted in rabbit cortical and cancellous bone. Int J Oral Maxillofac Implants. 1992. 7:62–71.
25. O'Sullivan D, Sennerby L, Meredith N. Influence of implant taper on the primary and secondary stability of osseointegrated titanium implants. Clin Oral Implants Res. 2004. 15:474–480.
26. Östman PO, Hellman M, Wendelhag I, Sennerby L. Resonance frequency analysis measurements of implants at placement surgery. Int J Prosthodont. 2006. 19:77–83.
27. O'Sullivan D, Sennerby L, Jagger D, Meredith N. A comparison of two methods of enhancing implant primary stability. Clin Implant Dent Relat Res. 2004. 6:48–57.
28. Sasaki KM, Aoki A, Ichinose S, Yoshino T, Yamada S, Ishikawa I. Scanning electron microscopy and Fourier transformed infrared spectroscopy analysis of bone removal using Er:YAG and CO2 lasers. J Periodontol. 2002. 73:643–652.
29. Schwarz F, Olivier W, Herten M, Sager M, Chaker A, Becker J. Influence of implant bed preparation using an Er:YAG laser on the osseointegration of titanium implants: a histomorphometrical study in dogs. J Oral Rehabil. 2007. 34:273–281.




 PDF
PDF ePub
ePub Citation
Citation Print
Print






 XML Download
XML Download