Abstract
PURPOSE
The aim of this study was to examine the relationship between tooth loss and sub-clinical atherosclerosis in Korean adults.
MATERIALS AND METHODS
The subjects were part of a cohort study conducted in Ansan city by the Korea University medical school as part of the Korean Genome project. 749 subjects over than 40 years old were evaluated. After taking panoramic radiography, the amount of tooth loss was calculated. The intima-media thickness (IMT) was assessed by using ultrasonography at the common carotid artery. Traditional cardiovascular risk factors for atherosclerosis were also evaluated. The relationship between tooth loss and the IMT was evaluated using ANOVA with Scheffe's multiple comparison method in univariate analysis. Multiple regression analysis was also performed to determine the significance between the IMT and tooth loss.
RESULTS
With age, tooth loss increased, but there was no significant increase in other traditional cardiovascular risk factors. Univariate analysis revealed the IMT to be positively related with the amount of tooth loss. Regression analysis of the IMT in the anterior and posterior tooth loss revealed that only the posterior tooth loss was significantly related with the IMT at all sites of the common carotid artery (right far wall, P = .015; left far wall, P = .008; right near wall, P < .001; left near wall, P = .001).
Cardiovascular diseases, cerebrovascular diseases and peripheral arterial diseases are responsible for approximately 50% of all mortality in the United State, Europe and Japan.1 Atherosclerosis is a major component of these diseases.1 The traditional risk factors, including behavior, diet, lifestyle and family history, do not affect totally the development of atherosclerosis. Many studies have suggested that inflammation plays a key role in the development of atherosclerosis.2,3
Chronic periodontitis is a typical inflammatory disease. Periodontitis is a chronic infection and inflammation in the periodontal tissue, leading to the destruction of bone structure surrounding the teeth, and finally leading to tooth loss.4 The prevalence of periodontal disease appears particularly high in the adult population.5 Chronic periodontitis is the most common reason for tooth loss in adults aged 40 years or more.6 Especially in Korea, chronic periodontitis occurs in 7 out of 10 adults.7
It was recently reported that periodontal disease affects not only oral physiological and esthetical aspects but also systemic diseases, such as cardiovascular diseases or atherosclerosis.8.9 Several well-designed pre-clinical studies provided possible mechanistic explanations for the relation between periodontal infections and atherosclerotic cardiovascular disease.10,11 Recent observational studies and meta-analysis also demonstrate modest but significantly increased risks of cardiovascular diseases among people exposed to periodontal diseases or infections.12,13
B-mode ultrasonography is a non-invasive and highly reliable tool for assessing the early stages of atherosclerosis14 by measuring the thickness of the inner layer of the vessel walls. This procedure has been used extensively to monitor the carotid artery and identify the sub-clinical atherosclerosis condition. These days, several studies reported a positive relationship between periodontitis and IMT which is a subclinical method to measure atherosclerosis. However, these studies were performed only in the United States15-18 and Europe,19,20 not in Asia. This study examined the relation between tooth loss and sub-clinical atherosclerosis in Korean adults more than 40 years of age.
As part of the Korean genome epidemiology studies, the Korea University School of Medicine's genomics research institute compiled information since 2001 of 5,020 citizens living in Ansan City aged between 40 and 69 years via a telephone survey, and performed a cohort study every 2 years. Among 926 individuals who have regularly taken panoramic radiography screening from March 2008 to September 2008 at the Korea University Ansan Medical Center's Department of Dentistry, 749 individuals were participated in this study. These individuals were selected because they were not related to any other subjects and have consistently cooperated in this cohort study for the past eight years.
The evaluation of tooth loss was assessed by panoramic radiography readings. Extractions of third molars and extractions performed for orthodontic treatments were not considered as tooth loss, whereas extractions for the purpose of dental implant treatments were considered as tooth loss. The type of tooth loss was categorized as anterior and posterior. All radiography readings and assessments were done by one dentist.
Certified examiners scanned the common carotid artery bilaterally with B-mode ultrasound using a 5-MHz linear probe array transducer and a high-resolution instrument (TITAN™, Sonosite® Japan). During the examination, the participants were in the horizontal position. The far and near walls were measured 1 cm away from the bifurcation.
Personal information such as age, gender, smoking, alcohol consumption, physical activities, prior medial history and family history was collected from all participants. Regarding smoking or alcohol consumption, the participants were categorized as never smokers or drinkers, past smokers or drinkers, and current smokers or drinkers.
First, the participant's blood pressure was measured on both forearms in the sitting position, and then it was measured again twice on the forearm that had a higher value. After each participant took a 5-minute rest in the supine position, the blood pressure was measured twice one more with 30 second intervals in the sitting position.
The waist circumference was measured 3 times at the largest dimension using a tape measure, and the mean was calculated. The body mass index (BMI), which is the weight in kilograms divided by height in meters squared, was also used to estimate the overall adiposity.
All the data in the study were summarized with mean ± standard deviation for continuous variables and with frequency (percentage) for discrete variable. The relationships between tooth loss and the traditional cardiovascular risk factors for atherosclerosis were analysed with analysis of variance (ANOVA) for continuous variables such as age, body mass index, waist hip ratio, and blood pressure. Chi squared test or Fisher's excat test were used to discrete variables including gender, alcohol consumption, smoking, and exercise. For univariate analysis of the relationship between tooth loss and carotid artery IMT, ANOVA with Scheffe's multiple comparison was performed. Multiple regression analysis with stepwise variable selection was used to determine the significance of tooth loss as an independent prognostic factor of IMT. All statistical analyses were performed using SAS v.9.13. A P value of < .05 was considered statistically significant.
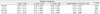
Of the 749 individuals, there were 373 males and 376 females. The average age of the individuals without tooth loss, 1 to 8 teeth loss, 9 to 15 teeth loss and more than 16 teeth loss was 53.1, 55.1, 60.6 and 65 years, respectively. There were more individuals with teeth loss (480 individuals) than those without (269 individuals). There were no significant differences in tooth loss between men and women. However, there was an increase in tooth loss with age (P < .0001) (Table 1).
Regarding alcohol consumption, 332 individuals were non-drinkers, 35 individuals used to drink but quit, and 395 individuals still consumed alcohol during the period of this study. Individuals who consumed alcohol outnumbered those who did not, but there was no significant relation between regular drinkers and tooth loss. Regarding smoking, there were more individuals who did not smoke than those who did but the difference was not significant. Similarly, no statistical significance was observed in comparing the obesity level with the amount of tooth loss. There was a slight correlation between the increase in tooth loss and the increase in systolic blood pressure, but less with the diastolic blood pressure. However, this result was also statistically insignificant. Finally, regarding to physical activity, tooth loss and the amount of physical activity appeared to be negatively correlated while individuals who did not exercise appeared to have increased tooth loss on average compared to those who practiced some form of regular exercise.
Posterior tooth loss (mean of 2.156) had a much higher incidence than anterior tooth loss (mean of 0.581) among the loss of anterior and posterior tooth combined (mean of 2.996) (Table 2).
A gender difference in the IMT of the common carotid artery has been reported. Therefore, the male group and female group were analyzed separately (Table 3, 4). In the case of females, an increase in tooth loss correlated with a noticeable increase in IMT at both the left and right near positioned walls and par positioned wall (RTCF, P = .0479; LTCF, P = .0030; RTCN, P = .0041; LTCN, P = .0254). In the case of males, there was a significant correlation between tooth loss and the IMT in the right far and near positioned walls and the left near positioned wall of the common carotid artery (RTCF, P = .0324; RTCN, P = .0115; LTCN, P = .0217). However, the statistical significance in the left far positioned near positioned wall was marginal (P = .1041).
After selecting variable regression models, the effect of anterior and posterior tooth loss on IMT was determined through regression analysis (Table 5). The increase in posterior tooth loss correlated with the increase in IMT in both the far and near positioned walls of the common carotid arteries (RTCF, P = .015; LTCF, P = .008; RTCN, P < .001; LTCN, P = .001). However, the anterior tooth loss did not show significant correlation with the increased IMT (RTCF, P = .115; LTCF, P = .530; RTCN, P = .906; LTCN, P = .759).
This study examined the relationship between tooth loss and sub-clinical atherosclerosis in Korean adults aged more than 40 years. The amount of tooth loss in the posterior area was significantly related with the IMT of the common carotid arteries. Because periodontal disease is the commonest reason for posterior tooth extraction in those aged over 40 and tooth extraction is the end-point of periodontal disease. It is suggested that periodontitis might be the factor of atherosclerosis, which is a cause of cardiovascular and cerebrovascular diseases. A significant relation between periodontitis and carotid IMT might provide evidence for a role of periodontitis in the pathogenesis of atheroma formation.
Inflammation plays a main role in the pathogenesis of atherosclerosis from its initiation to the development of clinical complications.2,21 In atherogenesis, inflammation plays a continuous role from endothelial cell expression of adhesion molecules to the development of a fatty streak, established plaque and finally plaque rupture.3 Exposure to infections, such as periodontitis, seem to perpetuate the inflammatory events in atherogenesis. The proposed biological mechanisms of the interaction between periodontitis and cardiovascular disease include direct bacterial effects on platelets, autoimmune response, invasion and/or uptake of bacteria in endothelial cells and macrophages, and endocrine-like effects of pro-inflammatory mediators.22
Carotid atherosclerosis, seem to atherosclerosis in the carotid, is frequently measured as an increase in the thickness of the IMT of the arterial wall. Measurement of this parameter has attracted considerable attention because it is strongly in with disease in the coronary and cerebral arteries. In addition, it is also a good predictor of both cardiovascular and cerebrovascular ischaemic events. The IMT of the carotid artery, as measured by B-mode ultrasound, is a measure of a preclinical atherosclerosis that has been shown to be related with coronary heart disease, both prevalent23 and incident.24,25
Since Beck et al. reported that subjects with severe generalized periodontitis had a higher odds (OR 1.3, 95% CI 1.03-1.66) of having carotid IMT of 1 mm or more after correcting for other known factors,15 many studies have reported the relationship between periodontal disease and carotid artery IMT.16-19 They confirmed that severe bone loss,17 overall periodontal bacterial burden16 and tooth loss18 were associated with carotid IMT. This study is also coincidental with previous studies. A recent pilot study reported the effect of periodontal therapy on the changes in the carotid IMT.26 A group of otherwise healthy individuals affected by mild to moderate periodontitis was treated with root debridement. Six and twelve months later, the level of IMT was decreased significantly at different locations in the carotid artery. This pilot study suggests that changes in IMT after periodontal therapy are possible in systemically healthy subjects.
Many studies have also reported a relationship between tooth loss and cardiovascular disease. In a study of tooth loss and heart disease, an American telephone health survey system, known as Behavioral Risk Factor Surveillance System (BRFSS), was used to survey 41,891 individuals between 40 and 79 years of age. The results confirmed that individuals with tooth loss due to periodontal diseases had a higher risk of some form of heart disease than those without tooth loss.27 Therefore, tooth loss may be a subclinical factor of systemic diseases. From 1992 to 1995, the Republic of Korea National Health Insurance Corporation performed health screenings on 867,256 adult men and women aged 30 to 95; the amount of tooth loss of all participants was recorded. A study that examined fourteen years of tooth loss and stroke records of these patients concluded that tooth loss, stroke and the subtypes of stroke might be interrelated. The results indicated that an increase in tooth loss increased the likelihood of having a stroke more than in individuals who had not lost any tooth. Furthermore, tooth loss was independently associated with an increased risk of hypertension and stroke, particularly with hemorrhagic stroke.28
There was more posterior tooth loss than anterior tooth loss in the sample group, and the amount of anterior tooth loss and the corresponding IMT appeared to be statistically significant. This may be because the posterior area of the oral cavity is a vulnerable area to control the plaque mechanically by individuals. Moreover, most posterior teeth have furcation, which can make plaque control difficult. Therefore, furcation-involved teeth with periodontitis have a poor long-term prognosis.29 The greater influence of posterior periodontium on the development of atheroslerosis can be inferred, highlighting the importance of proper maintenance of the posterior teeth and periodontium.
A relationship between atheroma development (deduced via IMT interpretations) with tooth loss is highly likely. However, because of a relatively small sample size in this study, the calculated statistical significance of the various correlations may have considerable margins of error. In addition, there are many ways that tooth loss can occur but this study did not categorize tooth loss in accordance to this. Hence, it is unclear if all individuals truly experienced tooth loss due to chronic periodontal diseases alone. Many factors may also increase the IMT and further investigations on how these factors affect the sample will be necessary to strengthen the findings of this study. This study is also subjected to the limitation of a cross-sectional design, which allows the detection of a relationship but not the cause and the effect. The effect of periodontal therapy on changes in carotid IMT have to be verified to understand the cause and the effect better.
This study confirmed the positive relationship between the increased tooth loss in the posterior area and the accumulation of atheroma in the arteries. As chronic periodontitis is a major cause of tooth loss in those more than 40 years of age, it might be a risk factor for atherosclerosis.
Figures and Tables
ACKNOWLEDGMENTS
This study was supported by a grant of the Korea Centers for Disease Control and Prevention (2008-E00169-00).
References
1. Lusis AJ. Atherosclerosis. Nature. 2000. 407:233–241.
2. Libby P. Inflammation and cardiovascular disease mechanisms. Am J Clin Nutr. 2006. 83:456S–460S.
3. Ridker PM, Silvertown JD. Inflammation, C-reactive protein, and atherothrombosis. J Periodontol. 2008. 79:1544–1551.
4. Kinane DF. Causation and pathogenesis of periodontal disease. Periodontol 2000. 2001. 25:8–20.
5. Papapanou PN. Epidemiology of periodontal diseases: an update. J Int Acad Periodontol. 1999. 1:110–116.
6. Reich E, Hiller KA. Reasons for tooth extraction in the western states of Germany. Community Dent Oral Epidemiol. 1993. 21:379–383.
7. Ministry of Health & Welfare, Korea Centers for Disease Control and Prevention. 2007 Statistics of National Health. 2008. 66.
8. Southerland JH, Taylor GW, Moss K, Beck JD, Offenbacher S. Commonality in chronic inflammatory diseases: periodontitis, diabetes, and coronary artery disease. Periodontol 2000. 2006. 40:130–143.
9. Kinane D, Bouchard P. Group E of European Workshop on Periodontology. Periodontal diseases and health: Consensus Report of the Sixth European Workshop on Periodontology. J Clin Periodontol. 2008. 35:333–337.
10. Brodala N, Merricks EP, Bellinger DA, Damrongsri D, Offenbacher S, Beck J, Madianos P, Sotres D, Chang YL, Koch G, Nichols TC. Porphyromonas gingivalis bacteremia induces coronary and aortic atherosclerosis in normocholesterolemic and hypercholesterolemic pigs. Arterioscler Thromb Vasc Biol. 2005. 25:1446–1451.
11. Lalla E, Lamster IB, Hofmann MA, Bucciarelli L, Jerud AP, Tucker S, Lu Y, Papapanou PN, Schmidt AM. Oral infection with a periodontal pathogen accelerates early atherosclerosis in apolipoprotein E-null mice. Arterioscler Thromb Vasc Biol. 2003. 23:1405–1411.
12. Blaizot A, Vergnes JN, Nuwwareh S, Amar J, Sixou M. Periodontal diseases and cardiovascular events: meta-analysis of observational studies. Int Dent J. 2009. 59:197–209.
13. Persson GR, Persson RE. Cardiovascular disease and periodontitis: an update on the associations and risk. J Clin Periodontol. 2008. 35:362–379.
14. Bond MG, Wilmoth SK, Enevold GL, Strickland HL. Detection and monitoring of asymptomatic atherosclerosis in clinical trials. Am J Med. 1989. 86:33–36.
15. Beck JD, Elter JR, Heiss G, Couper D, Mauriello SM, Offenbacher S. Relationship of periodontal disease to carotid artery intima-media wall thickness: the atherosclerosis risk in communities (ARIC) study. Arterioscler Thromb Vasc Biol. 2001. 21:1816–1822.
16. Desvarieux M, Demmer RT, Rundek T, Boden-Albala B, Jacobs DR Jr, Sacco RL, Papapanou PN. Periodontal microbiota and carotid intima-media thickness: the Oral Infections and Vascular Disease Epidemiology Study (INVEST). Circulation. 2005. 111:576–582.
17. Engebretson SP, Lamster IB, Elkind MS, Rundek T, Serman NJ, Demmer RT, Sacco RL, Papapanou PN, Desvarieux M. Radiographic measures of chronic periodontitis and carotid artery plaque. Stroke. 2005. 36:561–566.
18. Castillo R, Fields A, Qureshi G, Salciccioli L, Kassotis J, Lazar JM. Relationship between aortic atherosclerosis and dental loss in an inner-city population. Angiology. 2009. 60:346–350.
19. Soder B, Yakob M, Nowak J, Jogestrand T. Risk for the development of atherosclerosis in women with a high amount [corrected] of dental plaque and severe gingival inflammation. Int J Dent Hyg. 2007. 5:133–138.
20. Leivadaros E, van der Velden U, Bizzarro S, ten Heggeler JM, Gerdes VE, Hoek FJ, Nagy TO, Scholma J, Bakker SJ, Gans RO, ten Cate H, Loos BG. A pilot study into measurements of markers of atherosclerosis in periodontitis. J Periodontol. 2005. 76:121–128.
21. Libby P, Ridker PM, Maseri A. Inflammation and atherosclerosis. Circulation. 2002. 105:1135–1143.
22. Paquette DW, Brodala N, Nichols TC. Cardiovascular disease, inflammation, and periodontal infection. Periodontol 2000. 2007. 44:113–126.
23. Burke GL, Evans GW, Riley WA, Sharrett AR, Howard G, Barnes RW, Rosamond W, Crow RS, Rautaharju PM, Heiss G. Arterial wall thickness is associated with prevalent cardiovascular disease in middle-aged adults. The Atherosclerosis Risk in Communities (ARIC) Study. Stroke. 1995. 26:386–391.
24. Salonen JT, Salonen R. Ultrasonographically assessed carotid morphology and the risk of coronary heart disease. Arterioscler Thromb. 1991. 11:1245–1249.
25. Bots ML, Hoes AW, Koudstaal PJ, Hofman A, Grobbee DE. Common carotid intima-media thickness and risk of stroke and myocardial infarction: the Rotterdam Study. Circulation. 1997. 96:1432–1437.
26. Piconi S, Trabattoni D, Luraghi C, Perilli E, Borelli M, Pacei M, Rizzardini G, Lattuada A, Bray DH, Catalano M, Sparaco A, Clerici M. Treatment of periodontal disease results in improvements in endothelial dysfunction and reduction of the carotid intima-media thickness. FASEB J. 2009. 23:1196–1204.
27. Okoro CA, Balluz LS, Eke PI, Ajani UA, Strine TW, Town M, Mensah GA, Mokdad AH. Tooth loss and heart disease: findings from the behavioral risk factor surveillance system. Am J Prev Med. 2005. 29:50–56.
28. Choe H, Kim YH, Park JW, Kim SY, Lee SY, Jee SH. Tooth loss, hypertension and risk for stroke in a Korean population. Atherosclerosis. 2009. 203:550–556.
29. Pihlstrom BL. Periodontal risk assessment, diagnosis and treatment planning. Periodontol 2000. 2001. 25:37–58.




 PDF
PDF ePub
ePub Citation
Citation Print
Print






 XML Download
XML Download