INTRODUCTION
Ceramic materials for CAD/CAM technology can be divided into two subgroups: polycrystalline ceramics and glass ceramics.
1 Glass ceramics have improved over the years in their compositions and processing techniques.
2 The dental ceramics that offer a combination of adequate translucency and improved mechanical strength are one of the research areas of the dentistry.
3 A new group of CAD/CAM ceramics has recently been introduced: zirconia-reinforced lithium silicate (ZLS) glass ceramics.
34 ZLS materials comprise a lithium-silicate glass ceramic that is strengthened with 8 – 12% zirconia crystals.
5 Manufacturers claim that the addition of 8 – 12% of zirconia could act as a crystal phase that can strengthen the material and prevent crack propagation.
26 The ZLS represents an attempt to combine resistance of polycrystalline ceramics with the esthetic properties of glass ceramics.
2 Although these ceramics are still relatively new to the dental market,
in vitro testing reports demonstrated that they have excellent optical and physical properties similar to lithium disilicate glass ceramics.
125 However, there are a few
in vivo studies that reveal details of the mechanical behavior and bonding performance of resin composite to ZLS CAD/CAM blocks.
12
Lithium disilicate and ZLS glass ceramics could be prepared as monolithic and bilayer restorations.
27 Beside the advantages of the usage of CAD/CAM restorations as monolithic, bilayer manufacturing is still preferred in anterior restorations.
8
All-ceramic restorations are known to be prone to fracture. 9 The usage of ceramics as monolithic or bi-layer may be related to mechanical complications encountered.
10 Fracture of veneering ceramics still remains the primary cause of all-ceramic crown failures.
11 Although the data are not clear as to how fractures occur, delamination with the exposure of core ceramic and minor chipping are the most frequent reasons for all ceramic restoration failures.
121314
The fractured all ceramic restorations can be repaired with intraoral adhesive repair procedures. In this way, removal of the restoration can be avoided by bonding resin composite to the fractured surface. With increasing fracture frequency of bilayer CAD/CAM ceramics, micromechanical and chemical bonding procedures are required to enhance the bond strength between ceramics and resin composite.
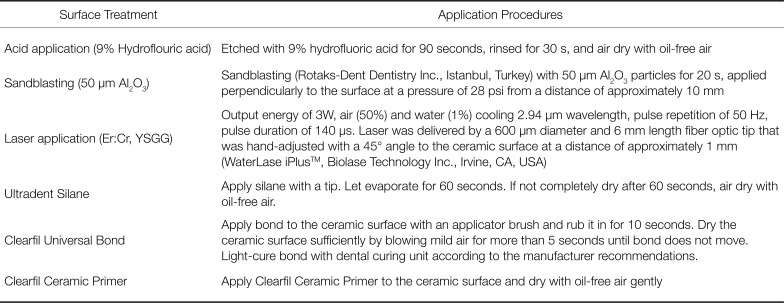
19 Mechanical surface treatments create microroughness at the ceramic surface, thus increasing the surface of ceramic and providing micromechanical interlocking.
1 Acid etching (etching with hydrofluoric acid (HF), etching with acidulated phosphoric acid or a phosphate fluoride), roughening with sandblasting (with aluminum oxide particle), roughening with diamond bur, and laser etching could be applied for micromechanical bonding.
1516 Recently, laser etching has become available as a current technology for bonding resin composites to the ceramics.
1517 Er, Cr: YSGG is a currently introduced laser that could be applied to both soft- and hard-tissue.
18 There are many
in vitro studies about the effect of Er, Cr: YSGG laser on the bond strength of resin composite to the ceramics. However, the effect of this laser on the bond strength of resin composite to new ZLS CAD/CAM blocks and the comparison of these results with the other CAD/CAM ceramics were not discussed previously in literature.
A strong resin bond relies on chemical bonding to the ceramic surface in addition to micromechanical interlocking.
19 Chemical bonding procedure consists of silane and bonding agent application. As chemical bonding procedure gets more complicated, a simple method to enhance the bond strength becomes necessary. Some molecules are available that contain a combination of silane and primer as an alternative to the silane/bond procedure. These one bottle silane coupling agents are able to create a direct bonding between ceramic surfaces and resin composite.
20 In this way, the ceramic repair procedure can be simplified clinically by eliminating the bond application step.
Concerning ceramic materials, mechanical failures and the propagation of cracks through the veneering ceramic and core ceramic in bilayer all ceramic restorations have been frequently reported in the literature.
2122 Repairable fractures in ceramic restorations can occur in many different types from small veneer chipping to large fractures that contain core and veneering ceramic together. Due to the different bond strength values depending on the exposed surface in the fracture, it is valuable to investigate the bond strength of the resin composite onto ceramic cores and veneering ceramics.
12
The null hypothesis of this study was that the exposure of the core ceramic on the fractured restoration surface would affect the bond strength of resin composites to the fractured ceramic surface. Additionally, the other null hypotheses were that the effects of surface treatments and bonding agents would be significant on the shear bond strength values of each fracture type and that thermocycling would affect the shear bond strength negatively.
MATERIALS AND METHODS
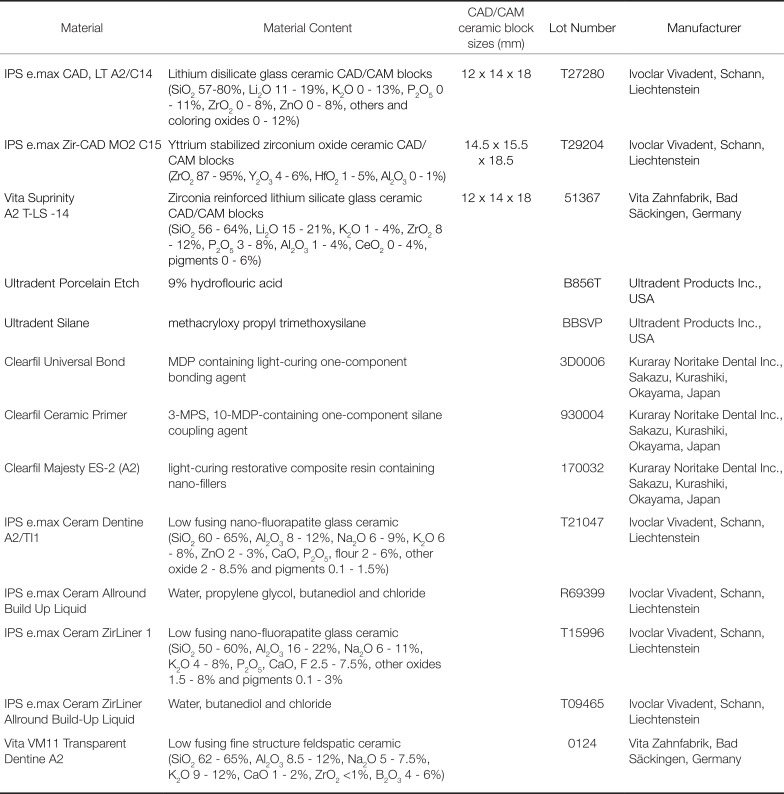
The tested ceramic types and the composition of the tested materials are summarized in
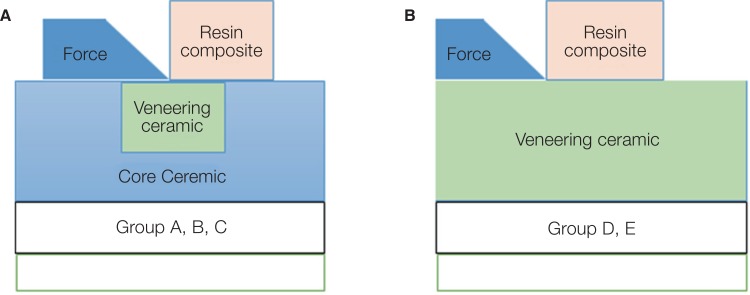
Table 1. Two different surface configurations were prepared in order to simulate the fracture types as follows:
• The fractures that contain core and veneering ceramic together (Groups A, B, and C) (
Fig. 1,
Fig. 2A):
Group A: 50% surface of resin composite bonded to veneering ceramic (IPS e.max Ceram) surface, and the other 50% to lithium disilicate glass ceramic (IPS e.max CAD). Group B: 50% surface of resin composite bonded to veneering ceramic (IPS e.max Ceram) surface, and the other 50% to yttrium stabilized zirconia ceramic (IPS e.max ZirCAD). Group C: 50% surface of resin composite bonded to veneering ceramic (Vita VM11) surface, and the other 50% to ZLS glass ceramic (Vita Suprinity).
• The fractures that contain only veneering ceramic (chipping) (Group D and E) (
Fig. 1,
Fig. 2B):
Group D: resin composite bonded directly onto veneering ceramic (IPS e.max Ceram) surface only, Group E: resin composite bonded directly onto veneering ceramic (Vita VM11) surface only.
A total of 336 blocks were cut from CAD/CAM blocks ceramics using a water-cooled diamond blade (Diamond Wafering Blade, 15LC, 11-4255, 127 × 0.4 mm, Buehler, Lake Bluff, IL, USA) with a low-speed cutting saw (Isomet 1000, Buehler Precision Saw, IL, USA), cutting liquid, and anticorrosive (Cool, Buehler, Düsseldorf, Germany).
The specimens of CAD/CAM glass ceramics (IPS e.max CAD and Vita Suprinity) were prepared with the dimensions of 12 × 12 × 3 mm. Subsequently, a slot cavity measuring 4 × 4 × 1 mm was prepared into each testing surface of glass ceramics. Then, the test specimens were crystallized in the porcelain oven (Ivoclar Vivadent, Programat EP 3000, Schaan, Liechtenstein) according to the manufacturer's recommendations. The veneering ceramic (IPS e.max Ceram) was applied into the prepared slot on the IPS e.max CAD specimens and was fired following the procedures recommended by the manufacturers (Group A). The other veneering ceramic (Vita VM11) was applied into the prepared slot on the Vita Suprinity specimens and fired (Group C).
IPS e.max ZirCAD specimens were prepared with dimensions of 15 × 15 × 3.75 mm. Due to the shrinkage of the IPS e.max ZirCAD specimens, a slot measuring 5 × 5 × 1.25 mm was prepared on each of the testing surfaces of these specimens. The sintering cycle according to the manufacturer's recommendations was completed in the sintering furnace (Sirona Dental Systems GmbH, Fabrikstr Bensheim, Germany). As a result of the 20% to 25% sintering shrinkage, the IPS e.max ZirCAD specimens presented dimensions of approximately 12 × 12 × 3 mm and slot measures of 4 × 4 × 1 mm. The surface of test specimens was cleaned with a steam cleaner (Vap-6; Zhermack technical, Badia Polesine, Italy). IPS e.max Ceram ZirLiner 1 was applied on these specimens as recommended by the manufacturers for increasing the bond strength between IPS e. max ZirCAD and veneering ceramic. The veneering ceramic powder (IPS e.max Ceram) was applied as recommended by the manufacturers on the specimens (Group B).
Due to the shrinkage of the veneering ceramics (20%), a cavity measuring 15 × 15 × 3.75 mm was prepared into an aluminum mold. Veneering ceramic blocks were prepared by mixing veneering ceramic powder with liquid. Then, the test specimens were fired in the porcelain oven according to the manufacturer's recommendations. The test specimens of IPS e.max Ceram (Group D) and Vita VM11 (Group E) measuring 12 × 12 × 3 mm were obtained.
All test specimens were measured with a digital caliper (World Precision Instrument Inc., Sarasota, FL, USA). Then, the surface of all test specimens was cleaned with a steam cleaner.
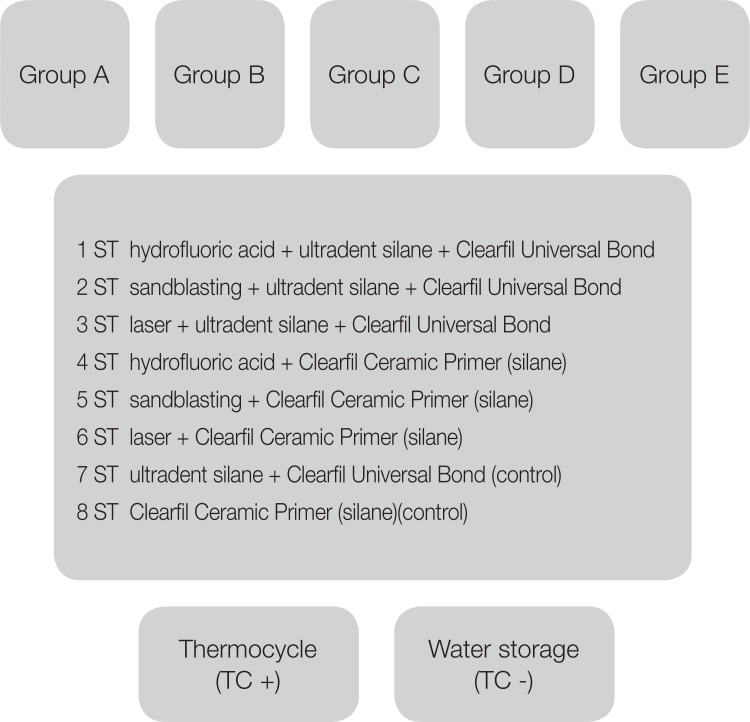
All test specimens were embedded in autopolymerizing acrylic resin using polyethylene mold (with dimensions of 16 × 16 × 10 mm) so that one surface of the test specimens remained uncovered for the bonding procedures. The test surfaces were finished with wet 600, 800, and 1200 grit silicon carbide paper (English Abrasives, London, UK) on a grinder-polisher device (Metkon Gripo 2V Grinder-Polisher, Bursa, Turkey). Then all specimens were cleaned using an ultrasonic bath (Bandelin Sonorex, Bandelin Electronic GmbH & Co. KG, Berlin, Germany) with distilled water at room temperature for 10 minutes, and dried with oil free air spray for 15 s. Subsequently, all specimens were randomly divided into eight subgroups (n = 14 per group) according to the three different surface treatment techniques and two different bonding procedures (
Table 2,
Fig. 1). The abbreviations of surface treatments are given in
Fig. 1. After the surface treatments were applied, all test specimens were subjected to ultrasonic cleaning in distilled water for 5 minutes and then dried. Afterwards, adhesive systems and nano hybrid resin composite (Clearfil Majesty ES-2-A2) were applied onto the treated test surfaces using a thermoplastic night-guard as a mold (4 × 4 × 2 mm).
Then, the resin composite was polymerized with a LED light curing unit (Valo, LED, Ultradent Products Inc., South Jordan, UT, USA; light output: 3200 mW/cm2). The light was directed from the intersection of the bonding area and resin composite. 6 s polymerization from two directions of approximately 45° and one 6 s exposure from the top were applied. A total time of 18 s per specimen was performed to ensure maximum polymerization.
All specimens were stored in 37℃ distilled water for 24 hours before being thermocycled. The specimens were divided into two subgroups based on whether thermocycling was to be done or not. Thermocycling (SD Mechatronik Thermocycler, Julabo GmbH, FT 200, Seelbach, Germany) was performed to half of the specimens (n = 7) for 5000 cycles between 5℃ and 55℃ with 60 s dwell time and 6 s transfer time (TC+). The other half was stored in distilled water (TC-) at 37℃ in an incubator (Kottermann Labortechnik, W. Germany) until thermocycle procedure ended.
Shear bond strength tests for all test specimens were carried out with a universal testing machine (Llyod Universal Testing Machine, AMETEK, Inc., Hampshire, England). A chisel apparatus was prepared to apply a parallel shearing force as close as possible to the resin/ceramic interface. The load was applied at a crosshead speed of 0.5 mm/min until delamination of the resin composite occurred (
Fig. 2). The shear bond strength values were calculated in megapascals (MPa) by the following equation: the failure load (in N) / the bonding area of resin composite (in mm
2).
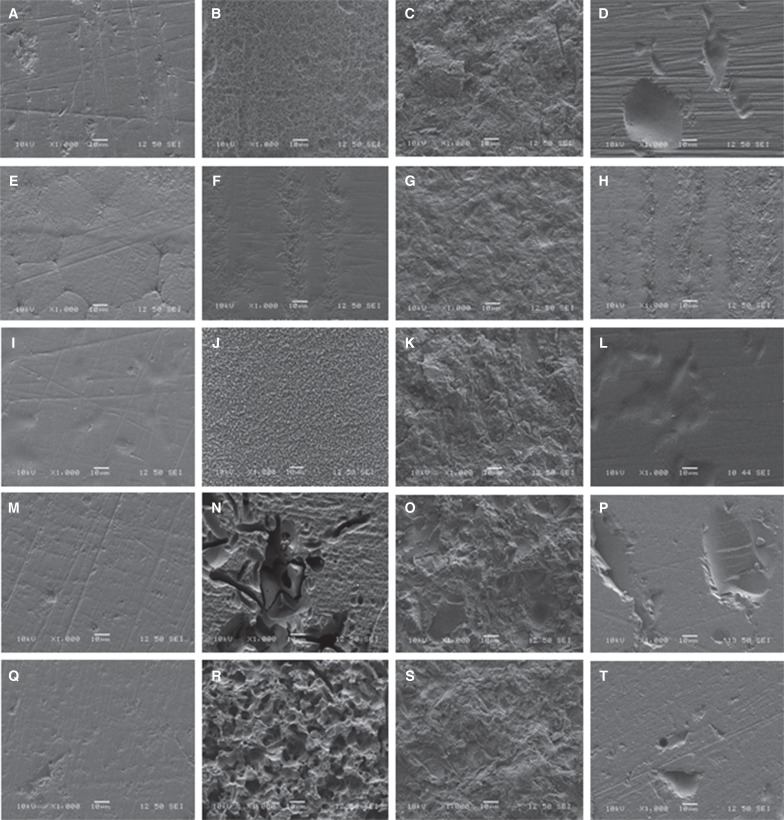
Following shear bond test measurement, all specimens were observed under an optical microscope (Leica MZ 12; Leica Microsystems GmbH, Wetzlar, Germany) at 12.5 X magnification to analyze the fracture pattern. The failure modes were categorized into three types: adhesive failure (Ad: interfacial separation between resin composite and tested surface), cohesive failure (Coh: failures occur in the part of resin composite), and mixture mode of failure (Mix: adhesive and cohesive failure). Two more test specimens were prepared from each type of tested ceramics in order to compare the surface changes after mechanical surface treatments. The specimens were sputter-coated (Sputter Coater SC7620, Polaron, VG Microtech, Uckfield, UK) (10 kV, working distance 12 mm, spot size 50, signal SEI) with gold and observed under a scanning electron microscope (SEM) (JEOL, JSM-6060LV, Tokyo, Japan).
Statistical analysis was conducted using IBM SPSS (version 17.0 software (IBM Corporation, Armonk, NY, USA). Statistical analysis was conducted with Kolmogorov-Smirnov test to evaluate the normal distribution of variables. Then, homogeneity test (Levene test) was used to verify the homogeneity of variance. Data were shown as median (IQR). Mann-Whitney U test was used to detect statistically significant differences in the mean bond strength values between two groups. In addition, statistical analysis was performed by Kruskal-Wallis test to make comparisons among more than two independent groups. When the P value from Kruskal Wallis test statistics were statistically significant, the Conover's multiple comparison tests were applied to determine which group showed significant difference. Unless otherwise indicated, P values less than 0.05 were considered to be statistically significant in all tests. Significance levels were adjusted using Bonferroni Correction for multiple comparisons to control Type I error.
RESULTS
The premature failures (debonding) occurred at 2nd and 3rd days of thermocycle process. Optical microscope analysis demonstrated predominantly adhesive failures.
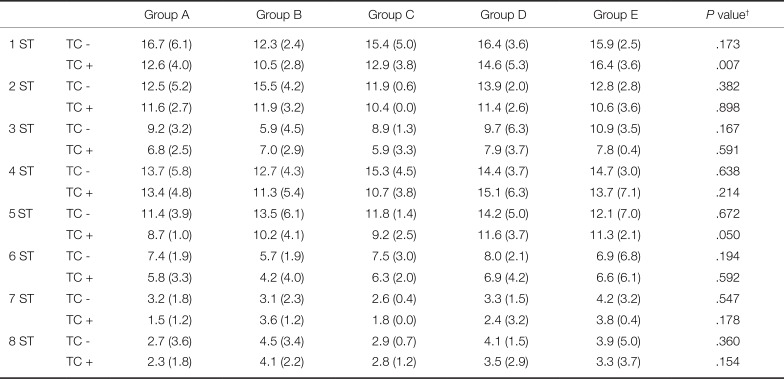
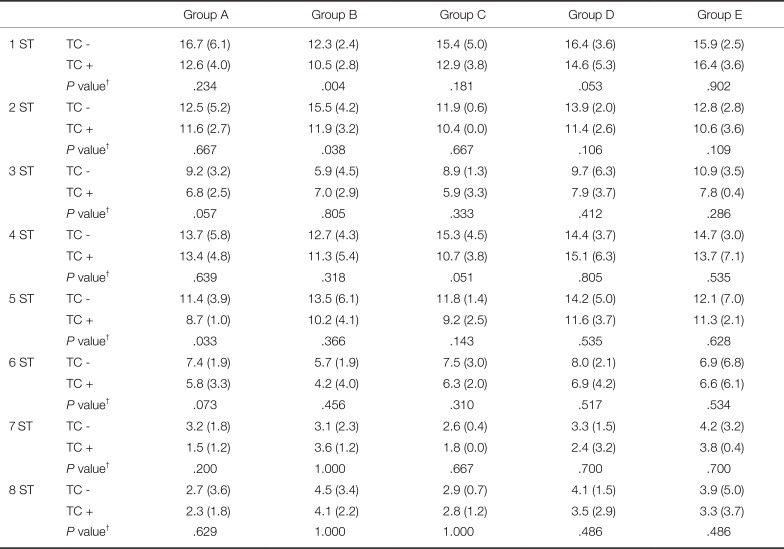
In the present study, the effects of fracture type/configuration, surface treatment, and thermocycling on the shear bond strength were evaluated. The differences in the shear bond strength were not statistically significant among the tested ceramic types (independent of the effect of surface treatment and thermocycle) (
P > .0031) (
Table 3). In addition, thermocycling (TC+) had no statistically significant effect on the shear bond strength of resin composite to any test specimens compared with the water storage groups (TC-) (
P > .00125) (
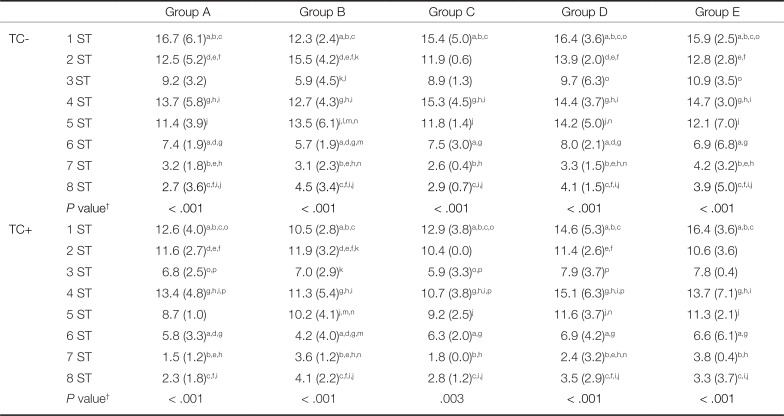
Table 4). However, although insignificant, a slight decrease in shear bond strength values was observed after thermocycling (TC+). The differences in the shear bond strength were statistically significant among the tested surface treatments (independent of the effect of ceramic type and thermocycling) (
P < .005,
Table 5). However, the differences in the shear bond strength were not statistically significant between two different bonding procedures (e.g. between 1 ST and 4 ST).
In Groups A, C, D, and E; HF etching provided higher shear bond strength values than the other tested surface treatments. Generally, there were no statistically significant differences between HF etching and sandblasting (P > .005). In Group B, sandblasting represented higher shear bond strength values than the other tested surface treatments. However, in Group B, the difference in shear bond strength values were not statistically significant between HF etching and sandblasting, independent of the bonding procedures performed (P > .001). Furthermore, shear bond strength values of laser etching were statistically lower than the values of sandblasting in Group B, TC- (P < .005). Additionally, the difference in shear bond strength values were not statistically significant between laser etching and control groups in Group B (P > .001).
Surface characteristics of the test specimens were influenced by surface treatments compared to the polished test specimen's surfaces (
Fig. 3). The surface irregularities were evident in HF etched subgroups of Groups A, C, D, and E (
Fig. 3B, 3J, 3N and 3R). Furthermore, sandblasting increased the roughness of the all test groups compared with those of control specimens (polished, without surface treatment) (
Fig. 3C, 3G, 3K, 3O and 3S). The SEM analyses indicated the inefficacy of laser etching on all test specimens. However, small amounts of porosity and flaws were detected in the laser etched test surfaces (
Fig. 3D, 3H, 3L, 3P and 3T).
DISCUSSION
In the present study, the fracture type and the amount of veneering ceramic on the fractured surface had no effect on the bond strength of resin composite. However, a significant difference in shear bond strength was found among the tested surface treatments in each test groups, leading to the acceptance of the null hypothesis (
Table 4).
Although there are many studies related to the fracture types of veneering ceramics,
2324 only a limited number of studies suggest the surface treatments that can be applied to the different type of fractured surface (only the veneering ceramic or both the veneering and core ceramic).
1223 Ozcan et al.
23 and Lee et al.
12 simulated the fractures in which two different types of ceramics were exposed together. Lee et al.
12 reported that there was not a statistically significant difference between the specimens that include both veneering ceramic and core ceramic on the fracture surface in terms of bonding strength. Similarly, in our results, shear bond strength values showed no statistically significant difference among the tested ceramic types (independent of the surface treatment type and thermocycling effect) (
P = .0031,
Table 3). Accordingly, it is proposed that fractures exposing the core-veneering ceramic or veneering ceramic only in the fracture line did not affect the bond strength of resin composites primarily.
Primers enhance the micromechanical bonding with resin in feldspathic ceramic, leucite, or lithium disilicate glass ceramics. However, it is difficult for zirconia ceramics to increase the bond strength because they do not contain silica.
19 Phosphate ester included in MDP based primers can create a chemical bond to the hydroxyl groups on the surface of zirconia ceramics.
25 Although zirconia ceramic framework was tested in Group B, no inter-group differences were thought to be associated with the usage of MDP based primers in both of bonding procedures.
252627
Valandro et al.
28 proposed the ceramic classification system, which is based on the amount of surface degradation by HF. Feldspathic, leucite, and lithium disilicate based ceramics are called as acid sensitive ceramics. In addition, alumina or zirconia polycrystalline ceramics are referred to as acid resistance ceramics. The ZLS have high content of glass phase (from 8 – 12% zirconia). Therefore, it was thought that the sensitivity of ZLS glass ceramics to roughening procedures could be similar with other glass ceramics.
2 One of the main questions of this study is how increased zirconia content in ZLS will affect sensitivity of this ceramic type to the surface treatments. In the present study, the increased content of zirconia did not result in a significant effect on the repair bond strength of ZLS glass ceramics. Similar surface treatments showed high bond strength values for both of ZLS and lithium disilicate glass ceramics. Etching with HF gel for 90 s (independent of the type of bonding procedure) resulted in the highest shear bond strength of the resin composite to core-veneering ceramic complexes in group A and C, and to veneering ceramics in group D and E (except control groups). When HF etching is applied to the surface of a glass-ceramic, vitreous matrix of glass ceramic is removed and crystalline structure is exposed. This surface topography results in increased surface area that improves ceramic wettability.
2 In a previous study, HF acid etching resulted in significantly higher bond strength in glass ceramics.
29 In addition, Menees et al.
30 concluded that HF etching provided more uniform and better distributed surface changes for the lithium disilicate glass ceramic. Similarly, our SEM analyses for lithium disilicate glass ceramic presented that HF etching resulted in more uniform surface changes than sandblasting.
The laser etching for surface roughening is an alternative method.
17 However, few studies have used Er,Cr:YSGG lasers to modify fractured ceramic surfaces with the purpose of increasing its bond strength to the resin composite.
151731 In previous studies, the effect of Er,Cr:YSGG laser treatments evaluated with various power outputs from 0.5 to 5.0 W.
153132 These studies reported that the microexplosions produce irregular alterations on the laser irradiated surface, thus increasing the micromechanical bonding between the ceramic surface and resin composite.
3233 Eduardo et al.
32 reported that Er,Cr:YSGG laser treatments with various power outputs from 0.5 to 5.0 W showed an acceptable effect on the ceramics. However, Shiu et al.
31 reported that Er,Cr:YSGG laser treatment resulted in low bond strength with regard to the shear bond strength of ceramic to resin cement. Similarly, in the present study, the use of Er:YAG laser irradiation for ceramic surface treatment resulted in lower bond strengths than those seen in the groups treated with HF acid or sandblasting. The SEM images of the Er,Cr:YSGG laser-treated surface showed a smooth, non-retentive surface compared to the treated surface with other surface treatments. Er,Cr:YSGG laser etching caused significant surface damage such as pits on the lithium disilicate glass ceramic and veneering ceramics (
Fig. 3D, 3P and 3T). In addition, the same surface treatment did not adequately roughen the zirconia reinforced lithium silicate glass ceramic and yttrium stabilized zirconium oxide ceramic as seen in SEM analyses results (
Fig. 3H and 3L). These results may be due to the laser irradiation power settings, since only a 3W power setting was used in the present study. Additionally, the shear bond strength values were slightly higher in the Er,Cr:YSGG laser group compared with the control groups. Therefore, the laser etching results of the present study will need to be supported by further studies with different laser parameters.
The sandblasting can induce excessive gaps in the surface of the ceramics or even a significant loss of material.
2 After sandblasting, yttrium stabilized zirconium oxide revealed a characteristic surface with sharp edges (
Fig. 3G). However, HF etching created a relatively smooth surface
Fig. 3F). These observations are identical to findings in other studies.
234 In the present study, HF etching and sandblasting presented higher bond strength than laser etching and control groups in Group B.
Sandblasting provided a significant roughness on the low fusing glass ceramic nano-fluorapatite glass ceramic and feldspathic ceramic (Group D and E) (
Fig. 3O and 3S). On the other hand, the laser etching on these specimens did not produce microporosities, but caused deep surface defects (
Fig. 3P and 3T), as was the case with lithium disilicate glass ceramic test specimens. Brentel et al.
35 demonstrated the effectiveness of HF etching on the feldspathic ceramic surface. However, HF etching may cause deep degradation on the ceramic surface.
135 In our study, HF etching caused fissures and undercuts on the surface of nano-fluorapatite glass ceramics. SEM analysis confirmed this effect with macro crack lines in
Fig. 3N. Similarly, HF etching created irregular macro porosity on the feldspathic ceramics. In the current study, this condition is thought to affect the clinical performance of this type of ceramic negatively. Shiu et al.,
31 in their study that evaluated the bond strength of resin composites to feldspathic ceramics, reported that HF etching and sandblasting showed higher bond strength than laser application (Er:YAG). The SEM analysis and the results of this study are similar to our results (
Fig. 3N, 3O and 3P). Similarly, in our study, 4 ST reported significantly higher bond strength than 6 ST in nano-fluorapatite glass ceramics (Group D, TC− / D, TC+) and feldspathic ceramic (Group E, TC− / E, TC+). Considering the results of the current study, HF etching should be preferred to observe the highest value and the most effective surface roughness for Groups A, C, D, and E. This is followed by sandblasting with high bonding ability and provides significant roughness. However, the laser application provided lower bond strength. This could be related with the insufficient roughening that is examined in the SEM analysis.
Both ceramic primer and some universal bonding agents contain 10-MDP.
36 This agent provides a relatively stable bond due to the hydrophobic property.
37 The one-bottle silane coupling agent (Clearfil ceramic primer) and silane/bond application in the current study contain MDP that chemically bonds to ceramic surfaces. In the current study, there was no statistically significance between two different bonding procedures (
P = .01). These results may be related with the MDP monomer content of the bonding agents. The results of this study demonstrate that the clinical application of ceramic repair can be simplified by using one-bottle silane coupling agent (Clearfil ceramic primer). This primer decreases the clinical application step of ceramic repair compared to silane/bond application.
Failure modes on the bonding surfaces between ceramic and resin composite reflected the results of the shear bond strength values (
Table 5). The failure mode results supported the conclusion that bond strength between ceramic and resin composite was low. Especially in control and laser etching groups, most of the failure types were adhesive. Generally, after thermocycling, the adhesive failure percentage at the resin-ceramic interface increased.
The ceramic restorations function in a moist environment with temperature changes. The degradation of the bonding area by hydrolysis is an important concern.
38 The long-term water storage and thermocycling could be used to investigate its effect on the bond strength of resin composite to ceramics. In the present study, thermocycling was used to reflect the clinical environment.
Thermocycling generally reduces the bond strength between resin composite and ceramics.
23739 Although the number of cycles showed great variation, it has been indicated that it is not essential to increase the number of cycles. This is because the effect of thermocycling on the bond strength occurs in the early phase of aging.
40 Other studies reported that the bond strength decreased with increase in the number of cycles.
241 Based on these reports, this study performed the aging process by 5000 times thermal cycling to investigate bond durability of resin composite. In our study, thermocycling resulted in a reduced bonding strength. However, the decrease was not statistically significant (independent of the effect of surface treatment and ceramic type) (
P = .00125) (
Table 4). It has been reported that applying a MDP-based primer to ceramic surface after thermal cycling did achieve stable bond strength.
42 The results of the present study are in accordance with the fact that this monomer provides stability against the hydrolysis during thermocycling.
4043 In addition, this result may be related with the usage of the nano hybrid resin composites. This type of resin composites have less interparticle gaps than the micro hybrid composite resin.
44 The decreased interparticle gap may result in less water passage through the particles.
Despite the improvements of the surface treatments and bonding agents, the repair in all-ceramic systems is still complex and needs to be developed. Up to now, bond strength studies are not decisive on suggesting the repair protocol for new ZLS glass ceramics, and the studies compare these results with zirconia ceramics and lithium disilicate glass ceramics. Additionally, this study simulated different fracture types such as chipping or bilayer fracture that contain core and veneer ceramics together. According to the results of the present study, the substrate type plays an important role on the stability of the resin composite bonding to the fractured surface. However, the fracture type did not affect the repair bond strength values.
Future studies should focus on the use of different mechanical surface treatments together on the fractured surface in which two type of ceramic exposed. In addition, clinical studies should be conducted to evaluate the nature of the repair bond strength and to verify the result of in vitro studies. The repaired restorations are intraorally subject to different forces such as tensile, shear, compressive, and oblique. The limitation of this study is that only shear force was applied to investigate the bond strength of resin composite to fractured ceramics. Additionally, in vitro test design did not completely mimic the intraoral environment and it has limited clinical comparability.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download