Abstract
STATEMENT OF PROBLEM
Over the years, resin-bonded fixed partial dentures (RBFPDs) have gone through substantial development and refinement. Several studies examined the biomechanics of tooth preparation and framework design in relation to the success rate of RBFPDs and considered retention and resistance form essential for increase of clinical retention. However, these criteria required preparations to be more invasive, which violates not only the original intentions of the RBFPD, but may also have an adverse effect on retention due to loss of enamel, an important factor in bonding.
PURPOSE
The object of this in vitro study was to compare the dislodgement resistance of the new types of RBFPDs, the conventional three-unit fixed partial denture, and conventional design of RBFPD (Maryland bridge).
MATERIAL AND METHODS
Fifty resin mandibular left second premolars and second molars were prepared on dentiforms, according to the RBFPD design. After model fabrication (five group, n = 10), prostheses were fabricated and cemented with zinc phosphate cement. After cementation, the specimens were subjected to tensile loading at a cross head speed of 4 mm/min in a universal testing machine. The separation load was recorded and analyzed statistically using one-way analysis of variance followed by Duncan's multiple range test.
RESULTS
Group V, the pin-retained RBFPDs, had the highest mean dislodgement resistance, whereas specimens of group II, the conventional RBFPDs, exhibited a significantly lower mean dislodgement resistance compared to the other 4 groups (P < .05). There were no significant differences between group I, III, and IV in terms of dislodgement resistance (P > .05). Group V had the highest mean MPa (N/mm2) (P < .05). There was no significant difference between groups I, II, III and IV (P > .05).
CONCLUSION
Within the limits of the design of this in vitro study, it was concluded that: 1. The modified RBFPDs which utilizes the original tooth undercuts and requires no tooth preparation, compared with the conventional design of RBFPDs, has significantly high dislodgement resistance (P < .05). 2. The modified RBFPDs which utilizes the original tooth undercuts and requires minimal tooth preparation, compared with the conventional FPDs, has significantly no difference in retention and dislodgement resistance)(P > .05). 3. The pin-retained FPDs showed a high dislodgement resistance compared to the conventional three-unit FPDs (P < .05).
The recent trend in restorative dentistry concerns fabrication of prosthesis with requirements of esthetic and functional needs on one hand and preserving as much sound tooth structure as possible on the other. The conventional full veneer or partial veneer crown retainers, although esthetic, have the major disadvantage of loss of healthy tooth structure during abutment preparation.
Over the years, resin-bonded fixed partial dentures (RBFPDs) have gone through substantial development and refinement. In 1973, Rochette1 described the use of a perforated gold casting for splinting periodontally weakened mandibular incisors. Later, Howe and Denehy2 used this technique for an anterior fixed partial denture, and Livaditis3 described this technique for posterior tooth replacement.
Although the early RBFPDs were considered as conservative, reversible, and cost-effective procedure for replacing missing teeth4, significant numbers of debonds were observed among many clinical successes.5 The debonding of the early RBFPDs was initially attributed to the weak link of the adhesive interface (metal-to-cement bond).6 To enhance the attachment of the resin cement to the metal surface, several techniques were developed; these included electrolytic or chemical etching of the casting to produce surface microroughness3,7,8 and macromechanical retention devices, such as incorporation of a mesh framework. Micromechanical retention through air abrasion with aluminum oxide, as well as the use of a silicoater, are currently used routinely for inducing surface microroughness of the metal surface.9 Resin cements used for cementation of RBFPDs went through a number of changes. Current chemically active resin cements have superior capabilities of bonding to base metal alloys and to treated or etched dentin, with simplified adhesive techniques.9,10
However, despite the improvements in adhesion, clinical results showed unsatisfactory retention rates for RBFPDs. Several studies examined the biomechanics of tooth preparation and framework design in relation to the success rate of RBFPD and considered retention and resistance form essential to increasing the clinical retention of RBFPDs.5,11,12 Consequently, the original design of RBFPDs went through a number of changes. Starting with no preparation of the abutments or minimal preparation with limited coverage of the abutments, preparations gradually became more and more invasive involving proximal grooves, tube or box-shaped proximal preparations, wraparounds or rest seats on the occlusal surface.13-15 This not only violates the original intentions of the RBFPD, but may also have an adverse effect on retention due to loss of enamel, which is an important factor in bonding.
A new modified type of RBFPD has been introduced and helps to solve the problems of the original undercuts and occlusal surfaces of the abutment teeth for retention. This restoration utilizes the elasticity of the alloy to be engaged in the natural tooth's undercut; also by cementing 3 components with different insertion paths, a high level of retention can be observed despite minimal reduction of tooth structure.
The purpose of this in vitro study was to compare the dislodgement resistance of the new types of RBFPDs, the conventional 3-unit fixed partial denture, and conventional design of RBFPD (Maryland bridge). Another modified RBFPD which uses pins was also evaluated.
According to the designs of the RBFPDs, fifty resin mandibular left second premolars and second molars were prepared on dentiforms. Resin teeth were selected for a couple of reasons. First, resin teeth were selected to obtain a uniform undercut and second, variations in etched enamel of natural teeth could cause differences in bonding strength. The prepared teeth were embedded in resin blocks (Ortho-jet; Lang Dental Mfg. Co., Wheeling, IL, USA) using pattern resin indices. Two pins were inserted at the mesial and distal surface perpendicular to the long axis to prevent tooth dislodgement during measurements. The models were divided equally into five groups.
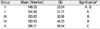
In group I, specimens were prepared to receive conventional three-unit fixed partial dentures(FPDs) with full veneered retainer. The amount of reduction for the functional cusps and for the nonfunctional cusps was 1.5 mm, and 1.0 mm respectively. The axial walls were reduced 0.7 mm with a torpedo diamond bur. A chamfer margin was placed at CEJ. In group II, specimens were prepared to receive conventional RBFPDs. In order to maximize lingual extension, the margins were placed 1 mm above the CEJ with a wing preparation of 0.7 mm. The grooves were placed mesial and distal to the proximolingual line angles with a carbide bur and occlusal rest seats were prepared adjacent to the pontics. In group III, there was no tooth preparation. In group IV, only occlusal rest seats were prepared on the distal of the second premolars and the mesial of the second molars. In group V, specimens were prepared to receive a pin-retained RBFPD, another modified RBFPD, with 1.0 - 1.5 mm occlusal dovetail retention form, proximal box, retention groove & flare and 0.7 - 1.3 mm pin holes (Table I).
Impressions were taken with additional silicone impression material (Aquasil Ultra XLA; Dentsply International Inc., Milford, DE, USA). After model fabrication (n = 10), castings were made in a Type III (75%) gold alloy (Goldenian c-79; Shinhung Co., Seoul, Korea) and cemented with zinc phosphate cement (Fleck's; Mizzy, Inc., Cherry Hill, NJ, USA). A groove was formed under the middle of the pontic to facilitate measuring of dislodging resistance.
In group III and IV, the prosthesis was constructed of 3 parts: two retention parts and a pontic. Each retention part had occlusal fossa coverage, buccal and lingual wing extentions. These extenctions engaged the undercut of the tooth and have an oblique path of insertion. The pontic part and retention part were firmly connected by a male/female structure (Fig. 2).
In group V, the prostheses had two holes. Readymade pins (Bio-pin®; Biodentech Co., Inchon, Korea) were inserted into each hole with 60 degree inclination to the path of insertion during the cementation procedure (Fig. 3).
The 3D digitizer (VIVID 9i; Konica Minolta, Osaka, Japan) was used to form a 3D image (Fig. 4-a), and the surface area was calculated using the Rapidform™ 2006 (Inus Technology, Inc, Seoul, Korea) program.
After cementation, the specimens were subjected to tensile loading at a cross head speed of 4 mm/min in a universal testing machine (Instron 3366; Instron Corporation, Norwood, MA, USA). A wire rope was used to permit the application of the tensile load at a specially made groove on the tissue side of the pontic, which was prepared during casting (Fig. 4-b). Each separating load was recorded.
SPSS V 12.0 for Windows (SPSS Inc., Chicago, IL, USA) was used for statistical analysis. Means and standard deviations for dislodgement resistances were determined, and data were analyzed statistically using one-way analysis of variance (ANOVA) followed by Duncan's multiple range test (Fig. 5).
ANOVA indicated that there was a significant difference in mean dislodgement resistances among the groups. Group V, the pin-retained RBFPDs, had the highest mean dislodgement resistance, whereas specimens of group II, the conventional RBFPDs, exhibited a significantly lower mean dislodgement resistance compared to the other 4 groups (P < .05). There were no significant differences between group I, III, and IV in terms of dislodgement resistance (P > .05). In group I, II, III and IV, mechanical failure occurred at the second premolar (Fig. 6), while in group V, tooth fracture occurred before restoration dislodgement (Table II).
The mean MPa (N/mm2) varied among the groups (Table III). Group V, the pin-retained RBFPDs, had the highest mean MPa (P < .05). Group I, the conventional full veneer 3-unit FPDs, had the lowest mean MPa but there was no significant difference between groups I, II, III and IV (P > .05).
Various changes in the microretentive features and the bonding materials for resin-bonded fixed partial dentures have been proposed throughout the years. However it appears that there is need for further modification of the design of the tooth preparation to incorporate other macromechanical retentive features to enhance the overall retention of the FPD and improve long-term prognosis. Arcoria14 used a retentive cove and El-Mowafy15 added a retentive-slot restoration filled with composite resin for improvement of retention. Chow16 reported an increase in retention using the groove, plate and strut approach. Yi17 reported that by inserting 2 pins at an oblique angle to the tooth's long axis, superior dislodgement resistance could be obtained. In 2004, Shimizu19 suggested a different posterior preparation and retainer design for posterior RBFPD to resist eccentric loading, using a mesiolinguobuccal arm in the molar abutment and a distolinguobuccal arm in the premolar abutment. Though their design is a conservative and esthetic approach, compared to the conventional three-unit FPD; local anesthesia is generally necessary in order to minimize patient pain while an occlusal strut is prepared to keep adequate retainer thickness18, since the enamel layer on premolars and molars is not sufficiently thick (under 0.4 mm).20
The modified design used in this study (group III, IV) utilizes the inherent flexibility of metal and the insertion path of the prosthesis to minimize amount of vital tooth to be prepared while obtaining a high value of retention. Therefore this design may be useful in restoration of a single missing tooth for patients who are uncomfortable with tooth reduction or patients who have anxiety towards dental treatment. Moreover, since no local anesthetics or surgical manipulations are necessary, it may be an excellent alternative for the medically compromised patient. According to the experiment results, the modified RBFPD groups (group III, IV) showed a significantly higher value in dislodgement resistance compared to the conventional RBFPDs; group II (P < .05), compared to group I and the conventional three-unit FPDs showed no significant difference (P > .05). These results may suggest that the RBFPDs which utilizes the original tooth undercuts and requires no tooth preparation, compared with the conventional FPDs, also has clinically acceptable retention and dislodgement resistance.
Group III, the no preparation group, and IV, the group with an occlusal rest seat preparation, had no statistically differences in dislodgement resistance (P > .05). This indicates that in the presence of occlusal clearance, difference in retention with or without occlusal rest preparation would not be significant.
The pin-retained FPD (group V) showed a superior dislodgement resistance compared to the conventional three-unit FPDs in this study and in most of the specimens, tooth fracture occurred before dislodgement of the restoration. This was probably due to the cementation of two pins inserted at an angle different to the path of insertion. However, there may be technical difficulties in preparing an oblique insertion path for the pins in the limited space of the oral cavity, and due to the preparation made at depth of 0.7 mm from the box, so some pulp irritation may occur.
When evaluating prosthesis retention in terms of surface area, there was no significant differences compared to conventional RBFPDs (P > .05). This is because groups III and IV have extensions on both the buccal and lingual sides while the conventional designs have extensions only on the lingual side. Accordingly there was no significant difference when the same vertical force was applied, but in cases of lateral force application, a large difference in retention according to surface area may be anticipated.
In the present study, resin teeth and zinc phosphate cement, which provides only mechanical retention, were used. In modified RBFPDs (groups III and IV), enamel, which has excellent bonding properties, was preserved on every surface without any dentin exposure. Therefore the dislodgement resistance of the restorations may differ when cements with enamel bonding properties are used on natural teeth. The large surface area of enamel may contribute to a larger retention value, if resin cements with bonding properties are used in clinical practice.
In this study we used resin teeth to produce identical test specimens for standardization of the undercut. Due to this limitation, the retention values obtained in this study cannot be compared directly with results obtained in the studies where natural teeth were examined. Also, the debonding of RBFPDs occurred not only due to mechanical dislodging but also by differences in the physiologic movement of natural teeth. Therefore further studies regarding the retention values of conventional three-unit FPDs and modified RBFPDs in natural teeth with various load applications are required.
The new modified type of RBFPD which utilizes original tooth undercut has the advantage of preserving sound tooth structure; however, there may be periodontal effects due to changes in tooth contour and cement wash-out is more likely to occur due to additional cement surfaces. Further research is required to assess the long-term prognosis of this type of RBFPDs.
Within the limitations of the design of this in vitro study, it was concluded that:
1. The modified RBFPDs which utilizes the original tooth undercuts and requires no tooth preparation, compared with the conventional design of RBFPDs, has significantly high dislodgement resistance (P < .05).
2. The modified RBFPDs which utilizes the original tooth undercuts and requires minimal tooth preparation, compared with the conventional FPDs, has significantly no difference in retention and dislodgement resistance) (P > .05).
3. The pin-retained FPDs showed a high dislodgement resistance compared to the conventional three-unit FPDs (P < .05).
Figures and Tables
Fig. 1
Model preparation & prosthesis fabrication. a. Group I: conventional full veneer three-unit FPDs. b. Group II: conventional RBFPDs. c. Group III: Modified RBFPDs with no preparation. d. Group IV: Modified RBFPDs with occlusal rest preparation. e. Group V: pin-retained RBFPDs.

Fig. 2
a. Schematic representation and example of Group III & IV. Two retention parts and middle pontic part. b. Arrows indicate the paths of insertion for each part.

Fig. 3
Schematic representation and example of Group V. Two readymade pins (Bio-pin®; Biodentech Co., Inchon, Korea) are inserted each hole with 60 degree inclination to the path of insertion during the cementation procedure.

Fig. 4
a. 3D image for surface measurement with 3D digitizer (VIVID 9i; Konica Minolta, Osaka, Japan). b. Dislodging resistance test with universal testing machine (Instron 3366; Instron Corporation, Norwood, MA, USA).

References
1. Rochette AL. Attachment of a splint to enamel of lower anterior teeth. J Prosthet Dent. 1973. 30:418–423.
2. Howe DF, Denehy GE. Anterior fixed partial dentures utilizing the acid-etch technique and a cast metal framework. J Prosthet Dent. 1977. 37:28–31.
3. Livaditis GJ. Cast metal resin-bonded retainers for posterior teeth. J Am Dent Assoc. 1980. 101:926–929.
4. Barrack G. A lood back at the adhesive resin-bonded cast restoration. J Esthet Dent. 1995. 7:263–273.
5. Priest G. An 11-year reevaluation of resin-bonded fixed partial dentures. Int J Periodontics Restorative Dent. 1995. 15:238–247.
6. Shaw MJ, Tay WM. Clinical performance of resin-bonded cast metal bridges (Rochette bridges). A preliminary report. Br Dent J. 1982. 152:378–380.
7. Livaditis GJ. A chemical etching system for creating micromechanical retention in resin-bonded retainers. J Prosthet Dent. 1986. 56:181–188.
8. Livaditis GJ, Thompson VP. Etched castings: an improved retentive mechanism for resin-bonded retainers. J Prosthet Dent. 1982. 47:52–58.
9. el-Mowafy OM. Posterior resin-bonded fixed partial denture with a modified retentive design: a clinical report. J Prosthet Dent. 1998. 80:9–11.
10. Botelho M. Resin-bonded prostheses: the current state of development. Quintessence Int. 1999. 30:525–534.
11. Simon JF, Gartrell RG, Grogono A. Improved retention of acid-etched fixed partial dentures: a longitudinal study. J Prosthet Dent. 1992. 68:611–615.
12. Hansson O, Bergström B. A longitudinal study of resin-bonded prostheses. J Prosthet Dent. 1996. 76:132–139.
13. Wiltshire WA. Resin bonded fixed partial dentures utilizing additional pin retention. Quintessence Int. 1986. 17:343–347.
14. Arcoria CJ, Dewald JP, Vitasek BA, Wagner MJ. Effect of undercut placement on crown retention after thermocycling. J Oral Rehabil. 1990. 17:395–402.
15. el-Mowafy O, Rubo MH. Retention of a posterior resin-bonded fixed partial denture with a modified design: an in vitro study. Int J Prosthodont. 2000. 13:425–431.
16. Chow TW, Chung RW, Chu FC, Newsome PR. Tooth preparations designed for posterior resin-bonded fixed partial dentures: a clinical report. J Prosthet Dent. 2002. 88:561–564.
17. Yi JW, Cho IH, Lee JH, Kim SK. A comparative study of the resistance to disloadgement of fixed prostheses using Bio-pin. J Korean Acad Prosthodont. 2005. 43:176–190.
18. Sato Y, Yuasa Y, Abe Y, Akagawa Y. Finite element and Weibull analysis to estimate failure risk in resin-bonded retainers. Int J Prosthodont. 1995. 8:73–78.
19. Shimizu H, Takahashi Y. Retainer design for posterior resin-bonded fixed partial dentures: a technical report. Quintessence Int. 2004. 35:653–654.
20. Stroud JL, English J, Buschang PH. Enamel thickness of the posterior dentition: its implications for nonextraction treatment. Angle Orthod. 1998. 68:141–146.




 PDF
PDF ePub
ePub Citation
Citation Print
Print






 XML Download
XML Download