Abstract
STATEMENT OF PROBLEM
Many dental clinicians are concerned about immediate loading of inserted implants. However, there have been few clinical studies surveying the success rates of immediate loading, based on Korean implant systems.
PURPOSE
The aim of this study was to evaluate the outcome of immediate functional loading of the implant (SinusQuick™ EB, Neobiotech Co., Seoul, Korea) in partially edentulous maxilla or mandible.
MATERIAL AND METHODS
Total 15 implants were placed. Within 2 weeks after implant insertion, provisional implant-supported fixed partial dentures were delivered to the patients. Quantitatively, marginal bone loss was measured at the time of immediate loading, after 3-months of continued loading and at the last follow-up. The mean follow-up period was 4.8 months.
Traditionally, implant treatment is based on a 2-stage protocol with a healing period of 3-6 months during which the implants are submerged to achieve osseointegration.1 Recently, this clinical suggestion has been challenged. Numerous practitioners now advocate immediate or early loading of implants.2 The advantages of immediately loaded implants are clear: they require shorter treatment periods and allow immediate recovery of function and esthetics.3
High success rate of immediately loaded implants in humans was first documented in the middle 1980s. The 88% cumulative success rate on 1739 immediately loading implants was suggested.4 The clinical performance and prognosis of the single-stage surgical protocol are known to be comparable to the traditional 2-stage method.5 There are some articles reporting a cumulative survival rate of 95%, which investigated immediately loaded single implants.6,7 Results from these studies suggest that immediate loading could achieve equal success rates as those found in delayed loading.
It is also known as a common claim that treatment with immediate loading improved patient satisfaction and was cost effective although no scientific evidence was presented to support.8 However, advantages of early or immediate loading as mentioned may be offset by an increased risk of implant failure. It was reported that immediately loaded implants were approximately 3 times more likely to fail within 1 year of placement.3 Furthermore, there have been few clinical studies investigating the success or failure rates of immediate loading based on Korean implant systems.
The aim of this preliminary prospective study was to evaluate the outcome of immediate functional loading in partial edentulism, using SinusQuick™ EB (Neobiotech Co., Seoul, Korea) implant system.
Four subjects (2 smokers and 2 non-smokers) recruited from a population of patients under routine care at Seoul National Bundang Hospital were enrolled in the study. The patients were selected according to the following inclusion criteria: they were in normal general health with sufficient bone to allow the placement of implants at least 7 mm length. Patients with high masticatory or parafunctional forces were excluded. The mean age of the subjects was 50.3 years (range from 39 to 65 years), with a gender distribution of 100% men. Informed written consent was obtained from all subjects following approved institutional review board guidelines for clinical research.
Surgery was performed under local anesthesia (1 : 100,000 Epinephrine) or conscious intravenous sedation with 1% Propofol solution and Midazolam. After a crestal incision, a mucoperiosteal flap was elevated. Implants were inserted according to the procedures recommended by manufacturers. During the period from April to October 2009 (range from 2 to 6 months), 15 SinusQuick™ EB implants were installed in patients' jaws. Immediate loading was applied to the implants showing implant stability quotient (ISQ) and insertion torque values that were more than 60 and 35 Ncm, respectively. Immediate loading is defined as provisional or final implant-supported restoration delivered within 2 weeks.9 Therefore, provisional implant-supported fixed partial dentures were delivered within 2 weeks (Fig. 1). The patients were instructed in soft diet and thorough oral hygiene care. The definite restoration was performed approximately 12 weeks after implant insertion.
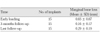
Periapical radiographs were taken using commercially available film holders and a paralleling imaging technique during the investigating period. In each patient, peri-implant marginal bone level was evaluated by IMPAX® (Agfa Co., Mortsel, Belgium) system of periapical radiographs. Measurements were recorded at the time of surgery, immediate loading, after 3-months of continued loading, and at the last follow-up (Fig. 2). Marginal bone height was determined on these images by measuring the distance from a reference point, defined as the platform of the implant (Fig. 2), to the most coronal point of bone-to-implant contact on both the mesial and distal sides of the implant. A single value for marginal bone height was then calculated by obtaining the mean of these two measurements for each implant.
The definition of implant success was based on the following clinical and radiologic criteria: 1) absence of clinically detectable implant mobility, 2) absence of pain or any subjective sensation, 3) absence of recurrent peri-implant infection, and 4) absence of continuous radiolucency around the implant.10
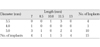
Total 15 implants were placed and were loaded immediately. Table I shows the details of distribution of inserted implants. Marked variability was noted in the implant sizes selected for placement, although implants 11.5 mm length and 5.0 mm diameter were most commonly used. The mean follow-up period was 4.8 months (range, 2 to 6 months). Mean marginal bone loss from implant surgery to immediate loading, 3-months follow-up and last follow-up was found to be 0.03 mm, 0.16 mm and 0.29 mm respectively (Table II). No implant failed up to 6 months after insertion, resulting in a 100% survival rate.
All the inserted implants showed successful integration and stable peri-implant condition up to six months. Primary stability was reported to be the most important determining factor on immediate implant loading.6 Micromovements of more than 100 µm were sufficient to jeopardize healing with direct bone-to-implant contact.6 Szmukler-Moncler et al. indicated that micromotions at the bone-implant interface beyond 150 µm resulted in fibrous encapsulation instead of osseointegration.11 If the primary implant stability could not be achieved or was questionable, it was strongly recommended to follow a conventional treatment protocol.6 Most agreed that an insertion torque of at least 32 Nm and a resonance frequency analysis of at least 60 ISQ was required to achieve a high level of stability.12 In this study, mean ISQ of 15 early loaded implants was 64.9 ± 4.9.
Generally, clinicians agreed that the quality of bone was significant for success in immediate loading. The initial stability of the implant reduces in the first 3-6 weeks after placement due to remodeling and an increased ratio of woven to lamellar bone.12 Barewal et al. indicated that implants placed in areas of high bone quality are relatively stable over the early healing periods.13 However, we reported that both maxillary and mandibular arches showed no failure of implants although the sample size was too small to analyze the data. Horiuchi et al. also reported about no difference in the success rate between arches in immediate loading.14 Further studies are required about the relationship between bone quality and the success rate of immediate loading.
It has been established that there are no absolute contraindications to implant placement although a number of conditions exist, which are associated with an increased risk of failure.12 Tobacco was reported to be only a risk factor for the implant failure.3 However, the results of this investigation showed there was no implant failure in the participating patients who were smokers. Long-term studies about relevance of smoking to early loading are necessary.
There were some limitations associated with this study. The number of investigated implants was insufficient to analyze the data using proper statistics. The follow-up period was also short. Therefore, we could not assess the long-term outcome of immediate loading. Further controlled clinical studies are needed to evaluate the long-term success of early loaded implants.
Within the limitation of this clinical study the preliminary results indicate that immediate loading of the implants in partial edentulism, based on SinusQuick™ EB implant system, may be successful for short period up to six months. Well-controlled long term clinical studies with large sample size are necessary.
Figures and Tables
Fig. 1
(A) Two implants (SinusQuick™ EB, Neobiotech Co., Seoul, Korea) were inserted at #36 and #37 area (black arrows). (B) Provsional restoration (white arrows) was delivered 14 days after implant placement.

Fig. 2
Periapical radiograph was taken at the time of (A) immediate loading and (B) 3-months after continued loading. The platform (black arrows) was a reference point to measure marginal bone loss. Provsional resin restoration was made by polymethylmethacrylate that is radiolucent. Therefore, only temporary cylinders are seen (white arrows).
ACKNOWLEDGEMENTS
The authors appreciate the financial help for this clinical research from Neobiotech Co., Korea.
References
1. Adell R, Lekholm U, Rockler B, Brånemark P. A 15-year study of osseointegrated implants in the treatment of the edentulous jaw. Int J Oral Surg. 1981. 10:387–416.
2. Chiapasco M, Gatti C, Rossi E, Haefliger W, Markwalder TH. Implant-retained mandibular overdentures with immediate loading. A retrospective multicenter study on 226 consecutive cases. Clin Oral Implants Res. 1997. 8:48–57.
3. Susarla SM, Chuang SK, Dodson TB. Delayed versus immediate loading of implants: survival analysis and risk factors for dental implant failure. J Oral Maxillofac Surg. 2008. 66:251–255.
4. Babbush CA, Kent JN, Misiek DJ. Titanium plasma-sprayed (TPS) screw implants for the reconstruction of the edentulous mandible. J Oral Maxillofac Surg. 1986. 44:274–282.
5. Henry P, Rosenberg I. Single-stage surgery for rehabilitation of the edentulous mandible: preliminary results. Pract Periodontics Aesthet Dent. 1994. 6:15–22.
6. Calandriello R, Tomatis M. Immediate Occlusal Loading of Single Lower Molars Using Brånemark System(R) Wide Platform TiUnite Implants: A 5-Year Follow-Up Report of a Prospective Clinical Multicenter Study. Clin Implant Dent Relat Res. 2009. [Epub ahead of print].
7. Maló P, Rangert B, Dvärsäter L. Immediate function of Brånemark implants in the esthetic zone: a retrospective clinical study with 6 months to 4 years of follow-up. Clin Implant Dent Relat Res. 2000. 2:138–146.
8. Attard NJ, Zarb GA. Immediate and early implant loading protocols: a literature review of clinical studies. J Prosthet Dent. 2005. 94:242–258.
9. Misch CE, Wang HL, Misch CM, Sharawy M, Lemons J, Judy KW. Rationale for the application of immediated load in implant dentistry: Part I. Implant Dent. 2004. 13:207–217.
10. Hobo S, Ichida E, Garcia LT. Osseointegration and occlusal rehabilitation. 1989. Tokyo: Quintessence Publishing Co., Ltd..
11. Szmukler-Moncler S, Salama H, Reingewirtz Y, Dubruille JH. Timing of loading and effect of micromotion on bone-dental implant interface: review of experimental literature. J Biomed Mater Res. 1998. 43:192–203.
12. Henry PJ, Liddelow GJ. Immediate loading of dental implants. Aust Dent J. 2008. 53:S69–S81.
13. Barewal RM, Oates TW, Meredith N, Cochran DL. Resonance frequency measurement of implant stability in vivo on implants with a sandblasted and acid-etched surface. Int J Oral Maxillofac Implants. 2003. 18:641–651.
14. Horiuchi K, Uchida H, Yamamoto K, Sugimura M. Immediate loading of Brånemark system implants following placement in edentulous patients: a clinical report. Int J Oral Maxillofac Implants. 2000. 15:824–830.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download