Abstract
STATEMENT OF PROBLEM
Proper proximal contact is important for maintaining and stabilizing the dental arch. However, the proximal contact strength (PCS) is not a constant value and can be affected by a variety of factors.
MATERIAL AND METHODS
Twelve adults with a normal occlusion and had not undergone prosthetic treatment or proximal restoration were participated in this study. A metal strip was inserted into the proximal surface and removed at a constant velocity. The contact strength was measured in every contact point between canine to second molar in both arches. The PCSs were obtained initially in the upright position, secondly in the supine position and finally in the upright position again. All measurements were repeated after a 2 hour period. Statistical analysis was carried out using the Friedman test (P < .05).
RESULTS
Generally, a decrease in PCS occurred when the posture was changed from the initial upright to supine position, while it increased when the posture was changed from the supine to upright position. A significant change was observed in all areas except for between the canine-first premolar in the maxilla and between the first molarsecond molar in the mandible areas.
Proximal contact is the area of a tooth that is in close association, connection or in touch with an adjacent tooth in the same arch.1 The tooth is stabilized by contact with the adjacent teeth as well as by occlusal contact with the opposite tooth.2 Proper proximal contact plays an important role in maintaining and stabilizing the dental arch.3 However, weak or slightly opened proximal contact causes food impaction, dental caries, periodontal disease, failure of occlusion and an undesirable drift of the teeth. On the other hand, too tight contact can damage the periodontal tissue or cause improper tooth movement or interfere with the physiological displacement of the teeth. Therefore, maintaining the proper proximal contact in natural dentition and in tooth restorations is important.4-11
The proximal contact strength (PCS) during tooth restoration is generally determined by the floss that passes through the contact point. Dentists note the proper contact in clinical treatment as the entry of floss with a snap.12 This method is simple but it is difficult to detect the detailed changes in the PCS.10 The PCS is considered to be too tight if the floss cannot pass through the contact area or tear out during entry, but too weak if the floss passes the contact area too easily.13
Therefore, it is important to investigate the proper PCS. Osborn14 initially reported the concept of a PCS measuring machine using the frictional force that occurs when an inserted thin metal strip escapes from the proximal area. When a metal strip is inserted between the nearby teeth, each tooth is displaced and they produce a force to resist the displacement. The PCS is defined as the force of the teeth resisting the mesio-distal displacement, and the technique of measuring the resistance is based on the concept of frictional force. Many studies have evaluated the PCS by using the frictional force. To measure the PCS, Dörfer et al.15 used a 0.05 mm thick metal strip and Oh et al.16 invented equipment to remove a 0.03 mm thick metal strip parallel to the proximal surface.
Southard et al.17 reported that the anterior portion of an occlusal force made from the posterior molar and the degree of irregularity in the anterior teeth were both related to the contact strength of unrestored posterior teeth. Dörfer et al.15 Suggested that the PCS is not a constant value but can be influenced by a variety of factors. Although the importance of proper contact strength is widely accepted by the dental community, the physiological factors that influence its magnitude have not been clearly defined. Therefore, the purpose of this study was to examine the influence of a postural change on the posterior PCS.
Details of the PCS measuring equipment used in this study are reported elsewhere.18 Briefly, the apparatus consists of a sensor part, motor part, body part and measuring part. The sensor transforms the output voltage from the strain gauge sensor to a digital signal, and the measurement limit is a maximum of 98 N. The motor part is a driving motor. In the measuring part, a metal strip, 2 mm in width and 0.03 mm in thickness, is fixed with a screw and inserted into the proximal surface. When the start button is pushed, the metal strip is removed at a velocity of 8 mm/s. The distal part of the measuring section, which is bent in a right angle, enables easier measurements at the posterior teeth.
Twelve young and healthy adults (male: 8, female: 4), aged between 23 - 33 years (mean age: 25.3 years old), with a class I, normal occlusion consented to participate in the study. All subjects had healthy periodontal tissue and complete dentition from the second molars forward. No subject had a history of prosthetic treatment, proximal restoration or orthodontic treatment over last 1 year. In addition, they did not show any signs or symptoms of food impaction or TMJ disorders.
The subjects were required to remain in the upright position for at least 1 hour before the start of the measurements, and asked to refrain from eating at least 1 hour before the experiment until the end of the experiment. However, occlusal contact or loading that occurs during general swallowing or clenching was allowed. After the subject sat in the upright position, they were asked to remain in a comfortable, muscle relaxed state. After turning on the equipment, the zero point setting was carried out. Before each experiment, the proximal surface was dried with an air syringe and a metal strip was then inserted into the proximal surface (Fig. 1).
The initial PCSs were obtained at the maxillary and mandibular canine - first premolar, first premolar - second premolar, second premolar - first molar and first molar - second molar proximal contact points. After pushing the start button, the metal strip was removed at a constant velocity. The highest value obtained during removal was regarded as the PCS. Each measurement was repeated 4 times. The representative PCS of each space was determined from an average of the 2 intermediate measurements, i.e. the highest and lowest values were excluded. During the measurement, all subjects were restricted not to make an occlusion, and a 2 minute - interval was allowed between each measurement. All experiments were carried out at approximately 7 pm and the subject was allowed sufficient rest after dinner.
After measuring the initial PCS, the subjects were asked to next assume the supine position. After 2 hours had passed, all the measurements were repeated. The subjects then returned to the upright position for an additional 2 hours and the same procedures were repeated.
Statistical analysis of the data was carried out using SPSS ver.12.1 (SPSS, Inc., Chicago, IL, USA). A Friedman test was used to evaluate the changes in the PCS in each proximal surface according to the postural change; initial upright, supine and final upright position. A value of P < .05 was considered significant.
Generally, the contact strength decreased when the posture was changed from an initial upright to a supine position. The contact strength then increased when the position was changed from the supine to upright position. In the maxilla, every other area except between the canine - first premolar showed significant changes (Tables I, II, III, IV). However, in the mandible, the only area showing a significant change was between the first molar - second molar (Tables V, VI, VII, VIII).
When a postural change was made from an initial upright position to a supine position, the maximum decrease was observed between the second premolar - first molar in the maxilla, and the minimum decrease was observed at the canine - first premolar in the mandible. After returning to the upright position, the maximum increase was observed at the second premolar - first premolar in the maxilla, and the minimum increase occurred at the canine - first premolar in the mandible (Figs 2 and 3).
After changing position from initial upright position to supine position, every area except between mandibular canine and first premolar showed statistically significant decrease and after coming back to final upright position, every area except between upper and lower canine and first premolar and between mandibular second premolar and first molar showed significant increase (Tables IX and X).
The equipment used in this study measured the PCS by evaluating the frictional force occurred while pulling a thin metal strip by an electric motor after inserting it into the proximal surface. Southard et al.19 could not measure the PCS between the first and second molars due to the limitation of the measuring equipment. However, the equipment used in the present study enabled measurement during occlusion as well as at between the first and second molars by minimizing the volume of the intraoral part and by bending the tip in a right angle. The frictional force is independent from the surface contact area and velocity at a low velocity, particularly in range of 0.83 - 8.33 mm/s.20,21 Therefore, the metal strip was removed at a constant velocity of 8 mm/s to rule out the effects of the removal velocity on the contact strength.
As the posture was changed from an initial upright to a supine position, the PCS generally decreased in both dental arches and then increased after returning to the final upright position from the supine position. When the posture changed from an initial upright to supine position, there was a significant decrease in all areas except between the canine and first molar area in the mandible, which corresponds to the results reported by Southard et al..19 After returning to the final upright position, significant increases were observed in the remaining area except between canine - first premolar in both arches and second premolar - first molar in the mandible. In contrast, Southard et al.19 reported significant increases only between the second premolar - first molar in the maxilla and mandible. However, they could not measure the value between the first and second molar due to the limitations of their measuring equipment. Dentists generally consider the proximal tooth contact to be a static feature of occlusion. However, this assumption is actually incorrect because the PCS changes with posture.
It appears that the PCS is influenced by a variety of factors, including the place and shape of the teeth, masticatory action, amount of mouth opening and postural changes, such as various positions of the head etc..15 In several studies, general increases in PCS from the anterior to posterior teeth were reported and significant differences were observed between the anterior and posterior teeth.9,15,22 Southard et al.23 insisted that the nearby teeth make contact with slight pressure with each other, and Kasahara et al.11 observed a 3 - 21 εm space between the adjacent teeth using a CCD (Charge Coupled Device) microscope.
Slight contact of the space between the adjacent teeth can be tightened or disappeared by tooth intrusion caused by the vertical portion of the power during its function, and the mesial displacement of the teeth caused by the horizontal portion of the power. These changes increase the PCS.17 The masticatory habits also have effects, and people with a unilateral masticatory habit show a larger increase in the working side after mastication.9 In order to minimize the effects of function, the subjects were asked to refrain from eating from 1 hour before the measurement until all measurements had been taken. However, occlusal contact or occlusal loading that occurred during functions, such as swallowing or speaking, were allowed.
The amount of mouth opening also affects the PCS due to mandibular deflection resulting from activation of the inferior head of the lateral pterygoid muscle.14 As the equipment used in this study removed a metal strip in the parallel direction, there was no need for excessive mouth opening. This is in contrast to other equipment, which removes the metal strip forward to the occlusal plane.15 Hence, the opening range of the subjects was limited to approximately 20 mm. In order to minimize the effect of mouth opening on the PCS, the subjects were asked to be in a comfortable state so every muscle would be relaxed as much as possible. In addition, the frictional force could be changed by the condition of the contact surface. Therefore, the measuring site was dried before each measurement.20
Although the difference is slight, the PCS changed with time. The PCS in the stable state increases in the morning and then decreases in the afternoon.15 This was explained by fatigue and the mucoelastic feature of the periodontal ligament. Because the highest level of masticatory muscle activation occurs during the eating periods in the daytime,24 every measurement was carried out at 7 pm, which is after dinner and sufficient rest. An interval of 2 hours was allowed between each measurement because the changes in contact strength were not observed immediately and we wished to obtain full expression of any effect from the posture.
A change in head position alters the blood flow of the periodontal ligament and gravity acting on the teeth. When a person moves between the upright and supine position, the musculo- skeletal system, neural system and circulatory system cooperate to compensate for the change in blood flow. In the supine position, an increase in cardiac output due to increased venous return up-regulates the diastolic arterial pressure and average arterial pressure.25,26 Furthermore, the increased pressure of the blood vessels produces a force sufficiently large to move the teeth under the physiological state.27 Several studies have reported that teeth undergo pulsatile movements corresponding to the arterial pulse.28,29 Changing posture from an upright to a supine position can increase the level of blood congestion or blood pressure in the periodontal ligament. The fact that these alterations can result in slight extrusion of the teeth from the alveolar socket seems to be quite reasonable. This extrusion can cause a slight decrease in the alveolar bone support for the teeth, and this decreased resistance can decrease the PCS. Opposite actions occurred when returning to the final upright position from the supine position.
There is a change in the direction of gravity functioning on the teeth as the subjects move from the upright to supine position. When one is in the upright position, gravity functions along the long axis of the teeth. However, the gravity changes direction toward the back in the supine position.19 Hence, every tooth experiences dorsal angulation in the bony alveolar socket. Consequently, the more posterior teeth will show a higher level of distal angulation caused by a postural change. The interrelationship between the posterior position of the teeth and the gradually increasing distal angulation would weaken the PCS in the posterior teeth. This is clear from the results of the present study. An opposite reaction was observed when the subject returned to the final upright position from the supine position.
The effects of posture on the PCS should be considered when placing fixed prostheses or restoration in the proximal surface.12,30 The placement of a posterior restoration and subsequent judgment of the contact strength by dentist after the patient is initially seated upright in the dental chair will reflect most accurately the PCS when the patient is functioning during the day. On the other hand, a restored contact that is judged to be of suitable tightness after a long appointment with the patient in the supine position may be excessively tight resulting in undesirable tooth movement.
In this study, the PCS from some subjects did not follow the general changes. An evaluation of the effect of factors other than posture will be needed because the PCS is a physiological feature, influenced by many factors such as position and shape of the teeth, mastication, amount of mouth opening and passage of time.
The effects of posture on the PCS of the posterior teeth were examined by measuring the PCS of 12 adults in the initial upright, supine and final upright position. Generally, there was a decrease in strength at all posterior proximal contacts in the maxilla and mandible when the subjects assumed a supine posture. On the other hand, there was an increase in contact strength after returning to the upright position from the supine position. Overall, the PCS of the posterior teeth, which dentists generally consider to be a static feature of occlusion, was altered significantly by changes in posture.
Figures and Tables
 | Fig. 1Measurement of the proximal contact strength between the first molar and second molar in the right side of the mandible. |
 | Fig. 2Diagrammatic presentation of the changes in proximal contact strength (N) in each region of the maxilla according to the postural change. |
 | Fig. 3Diagrammatic presentation of the changes in proximal contact strength (N) in each region of the mandible according to the postural change. |
Table I
Proximal contact strength (N) between the canine and first premolar in the maxilla according to the posture of the subjects
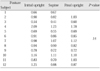
Table II
Proximal contact strength (N) between the first premolar and second premolar in the maxilla according to the posture of the subjects
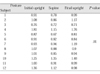
Table III
Proximal contact strength (N) between the second premolar and first molar in the maxilla according to the posture of the subjects
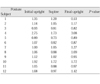
Table IV
Proximal contact strength (N) between the first molar and second molar in the maxilla according to the posture of the subjects
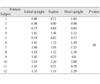
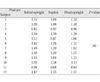
Table V
Proximal contact strength (N) between the canine and first premolar in the mandible according to the posture of the subjects
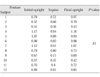
Table VI
Proximal contact strength (N) between the first premolar and second premolar in the mandible according to the posture of the subject
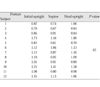
Table VII
Proximal contact strength (N) between the second premolar and first molar in the mandible according to the posture of the subjects
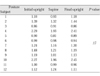
Table VIII
Proximal contact strength (N) between the first molar and second molar in the mandible according to the posture of the subjects
References
1. The academy of prosthodontics. The glossary of prosthodontic terms. 8th ed. J Prosthet Dent. 2005. 94:37. 57.
2. Andrews LF. The six keys to normal occlusion. Am J Orthod. 1972. 62:296–309.
3. Wheeler RC. An atlas of tooth form. 1969. 4th ed. Philadelphia, W.B.: Saunders Co;12.
4. Sluder TB. Studevant CM, editor. Clinical dental anatomy, histology, physiology and occlusion. The art and science of operative dentistry. 1985. 2nd ed. New York: McGraw-Hill;21.
5. Hirschfeld I. Food impaction. J Am Dent Assoc. 1930. 17:1504–1528.
6. Hancock EB, Mayo CV, Schwab RR, Wirthlin MR. Influence of interdental contacts on periodontal status. J Periodontol. 1980. 51:445–449.
7. Nielsen IM, Glavind L, Karring T. Interproximal periodontal intrabony defects. Prevalence, localization and etiological factors. J Clin Periodontol. 1980. 7:187–198.
8. Jernberg GR, Bakdash MB, Keenan KM. Relationship between proximal tooth open contacts and periodontal disease. J Periodontol. 1983. 54:529–533.
9. Vardimon AD, Matsaev E, Lieberman M, Brosh T. Tightness of dental contact points in spaced and non-spaced permanent dentitions. Eur J Orthod. 2001. 23:305–314.
10. Prakki A, Cilli R, Saad JO, Rodrigues JR. Clinical evaluation of proximal contacts of Class II esthetic direct restorations. Quintessence Int. 2004. 35:785–789.
11. Kasahara K, Miura H, Kuriyama M, Kato H, Hasegawa S. Observations of interproximal contact relations during clenching. Int J Prosthodont. 2000. 13:289–294.
12. Campagni WV. The final touch in the delivery of a fixed prosthesis. CDA J. 1984. 12:21–29.
13. Sturdevant JR, Sturdevant CM. Sturdevant C, Barton R, Sockwell C, Strickland W, editors. Gold inlay and gold onlay restoration for Class II cavity preparations. The Art and Science of Operative Dentistry. 1985. St. Louis, MO, USA: C.V. Mosby Co;490.
14. Osborn JW. An investigation into the interdental forces occurring between the teeth of the same arch during clenching the jaws. Arch Oral Biol. 1961. 5:202–211.
15. Dörfer CE, von Bethlenfalvy ER, Staehle HJ, Pioch T. Factors influencing proximal dental contact strengths. Eur J Oral Sci. 2000. 108:368–377.
16. Oh SH, Nakano M, Bando E, Keisuke N, Shigemoto S, Jeong JH, Kang DW. Relationship between occlusal tooth contact patterns and tightness of proximal tooth contact. J Oral Rehabil. 2006. 33:749–753.
17. Southard TE, Behrents RG, Tolley EA. The anterior component of occlusal force. Part 1. Measurement and distribution. Am J Orthod Dentofacial Orthop. 1989. 96:493–500.
18. Choi WJ, Kim KH, Kim JA, Kang DW, Oh SH. Evaluation and development of digital device for measuring proximal tooth contact tightness. J Korean Acad Prosthodont. 2007. 45:687–695.
19. Southard TE, Southard KA, Tolley EA. Variation of approximal tooth contact tightness with postural change. J Dent Res. 1990. 69:1776–1779.
20. Shames IH. Engineering Mechanics. 1966. Vol. 1. Englewood Cliffs, NJ: Prentice-Hall;170–174.
21. Fuhrmann R, Grave C, Diedrich P. In vitro evaluation of a measurement method to analyze the interdental, mesially directed force. J Orofac Orthop. 1998. 59:362–370.
22. Kim KH. Evaluation of proximal tooth contact tightness in permanent dentitions. 2007. Korea: Chosun University School of Dentistry;M.S. Thesis.
23. Southard TE, Southard KA, Tolley EA. Periodontal force: a potential cause of relapse. Am J Orthod Dentofacial Orthop. 1992. 101:221–227.
24. Miyamoto K, Yamada K, Ishizuka Y, Morimoto N, Tanne K. Masseter muscle activity during the whole day in young adults. Am J Orthod Dentofacial Orthop. 1996. 110:394–398.
25. Smith JJ, Kampine JP. Circulatory physiology- the essential. 1984. Baltimore, MD: Waverly Press, Inc.;235–237.
26. Rowell LB, Blackmon JR. Hunyor S, Ludbrook J, Shaw J, McGrath M, editors. Reflex and local control of the splanchnic circulation in humans. The peripheral circulation. 1984. New York: Excerpta Medica;114.
27. Moxham BJ. Davidovitch Z, editor. The role of the periodontal vasculature in tooth eruption. The biological mechanisms of tooth eruption and root resorption. 1988. Birmingham: EBSCO Media;208.
28. Körber KH. Periodontal pulsation. J Periodontol. 1970. 41:382–390.
29. Ng GC, Walker TW, Zingg W, Burke PS. Effects of tooth loading on the periodontal vasculature of the mandibular fourth premolar in dogs. Arch Oral Biol. 1981. 26:189–195.
30. Boice PA, Niles SM, Dubois LM. Evaluation of proximal contacts with shim stock. J Oral Rehabil. 1987. 14:91–94.




 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download