Abstract
STATEMENT OF PROBLEM
Poor wettability of denture relining materials may lead to retention problems and patient discomfort.
PURPOSE
Purpose of this study is to compare and evaluate wettability of nine denture relining materials using contact angle measurements under air and water storage over time.
MATERIAL AND METHODS
Nine denture relining materials were investigated in this study. Two heat-curing polymethyl-methacrylate (PMMA) denture base materials: Vertex RS, Lang, one self-curing polyethyl-methacrylate (PEMA) chairside reline resin: Rebase II, six silicone relining materials: Mucopren soft, Mucosoft, Mollosil® plus, Sofreliner Touch, GC Reline™ Ultrasoft, Silagum automix comfort were used in this experiment. Contact angles were measured using high-resolution drop shape analysis system (DSA 10-MK2, KRUESS, Germany) under three conditions (in air after setting, 1 hour water storage, and 24 hours water storage). Nine materials were classified into three groups according to material composition (Group 1: PMMA, Group 2: PEMA, Group 3: Silicone). Mean values of contact angles were compared using independent samples t-test and one-way ANOVA, followed by a Scheffe's post hoc analysis (α= 0.01).
RESULTS
Contact angles of materials tested after air and water storage increased in the following order: Group 1 (PMMA), Group 2 (PEMA), Group 3 (Silicone). Heat-cured acrylic denture base resins had more wettability than silicone relining materials. Lang had the highest wettability after 24 hours of water storage. Silicone relining materials had lower wettability due to their hydrophobicity. Wettability of all denture relining materials, except Rebase II and Mollosil® plus, increased after 24 hours of water storage.
Relining a complete denture may be required due to soft tissue changes arising from bone resorption. Denture relining materials absorb occlusal force and distribute to underlying alveolar ridge widely and enhance patient comfort.1
Relining a denture is performed directly in the mouth using auto-polymerizing denture relining materials and indirectly in the laboratory by heat-cured denture relining materials.2 Direct relining method is not only simple and practical but also time and cost effective. Advantages of the hard chairside relining resins include ease of manipulation and low exothermic heat of reaction.3 Disadvantages are that it shows much irritation and burning sensation of the mucosa, porosities, odor, color instability, and poor bonding of the relining material to the denture base material.4
Because clinically applied soft liners can lose their resiliency or fail to adhere to the denture base, they may be replaced with a more durable laboratory-processed liner.5 Loss of resiliency in soft liners may result from continued material polymerization over time, from material degradation caused by salivary or chemical compounds in the oral environment, or from leaching of the resin's plasticizing agent into the saliva.6
The method of polymerization may influence the properties of denture relining materials.7 Heat-cured PMMA denture base materials demonstrate greater abrasion resistance and bond strength, but lose elasticity and dimensional stability as the plasticizing agent leaches from the denture relining material.8,9 Self-cured reline resins are not subject to elevated temperatures and pressures, the physical properties of these materials are often lower than those that are laboratory-processed.10 Generally, silicones demonstrate greater resistance to change in physical properties when exposed to solid or liquid chemical components and are more elastic. The silicones do not actually bond to the acrylic resin of the denture, so an adhesive needs to be employed.
Wettability of denture base and denture relining materials is one of the most important properties for denture retention, because it provides a condition in which saliva will spread over the surfaces with ease.11,12 Contact angle has been highlighted as the most important parameter concerning wettability of denture relining materials. This angle is characteristic of the substances in the system due to the surface tension of the liquid and the surface energy of the solid. Low contact angle indicates good wettability. As the contact angle increases, the wettability decreases. The problem of poor wettability has been particularly associated with silicone soft lining materials and then may lead to frictional problems and patient discomfort.
The purpose of this study was to compare and evaluate the wettability of two acrylic denture base materials and one hard chairside reline resin and six silicone relining materials using contact angle measurements under air and water storage over time.
The materials used in this study are listed in Table I. Nine denture relining materials were used in the study: two heat-cured acrylic denture base materials, one hard chairside reline resin, six silicone relining materials were evaluated. Two heat-cured acrylic denture base materials: Lang (Lang Dental MFG Co., Wheeling, IL, USA), Vertex RS (Vertex Dental, Zeist, The Netherland) were prepared in the dental laboratory. One hard chairside reline resin: Rebase II (Tokuyama, Tokyo, Japan) was mixed with powder/liquid in room temperature. Six silicone relining materials: GC Reline™ Ultrasoft (GC Dental Products Co., Tokyo, Japan), Mollosil® plus (Detax, Ettlinghen, Germany), Mucosoft (Parkell, NY, USA), Mucopren soft (Kettenbach, Eschenburg, Germany), Silagum automix comfort (DMG, Hamburg, Germany), Sofreliner touch (Tokuyama, Tokyo, Japan) were automatically mixed and self-cured in room temperature. All procedures were followed according to the manufacturer's instructions.
Metal mold (100 × 55 × 10 mm) and two glass plates were prepared. Bar-shaped specimens (80 × 15 × 10 mm) were fabricated in metal molds. To obtain flat surface, specimens in metal mold were placed between two glass plates.
Static sessile water drops were observed as a function of time using the drop shape analysis (DSA) system (DSA10-MK2, KRUESS, Germany) (Fig. 1) combined with the analytical software (DSA1, KRUESS, Germany). The sessile drop technique, an optical contact angle method, is generally used to estimate wetting properties of a localized region on a solid surface.13
The angle between the baseline of the drop and the tangent at the three-phase-line solid/liquid/vapor is measured. At thermodynamic equilibrium, there is a balance of forces in the plane of the surface, expressed by the fundamental Young equation.14 The DSA system uses a high-speed camera to record changes of the drop contour and a software controlled multi-dosing system for generating reproducible droplets.
The volume of each water drop syringed on the flat impression material surfaces was 8 µl. The drop shapes have been recorded every second during an evaluation period of 20 s, respectively. The drop shape video recording was started just before droplet application. Identical set-up conditions were used for all measurements at a temperature of 37 ± 2℃. Each single measurement has been repeated eight times.
All samples were measured at instance after setting, 1 hour, and 24 hours. The specimens were stored in distilled water at 37 ± 2℃ for 1 hour and 24 hours. Specimens were divided into three groups according to material composition (Table II).
The means and standard deviations (SD) were calculated with computer. All data were statistically analyzed using independent samples t-test and one-way ANOVA. Significant differences among the groups were determined by a Scheffe's post hoc analysis. All analyses were computed with the SPSS for Windows Software (SPSS 13.0; SPSS Inc, Chicago, IL, USA) at the significance level of 0.01.
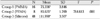
Means and standard deviations of contact angles of nine denture relining materials are presented in Fig. 2 and 3. After air setting, Vertex RS (72.55°) had the smallest contact angle and GC Reline™ Ultrasoft (114.95°) had the largest contact angle. The values of the contact angles were significantly different between the two materials (P < .01). Mean values of contact angles of Group 1, 2, and 3 were 75.36°, 85.63°, and 111.99°, respectively. The Scheffe's post hoc test demonstrated that contact angles were significantly different between groups (P < .01) (Table III).
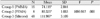
At 1 hour water storage at 37 ± 2℃, Vertex RS (73.53°) had the smallest contact angle and GC Reline™ Ultrasoft (115.31°) had the largest contact angle. The values of the contact angles were significantly different between the two materials (P < .01). Mean values of contact angles of Group 1, 2, and 3 were 74.12°, 89.33°, and 111.99°, respectively. The Scheffe's post hoc test demonstrated that contact angles were significantly different between groups (P < .01) (Table IV).
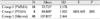
At 24 hours water storage at 37 ± 2℃, Lang (69.73°) had the smallest contact angle and Mucopren soft (111.93°) had the largest contact angle. The values of the contact angles were significantly different between the two materials (P < .01). Mean values of contact angles of Group 1, 2, and 3 were 70.73°, 88.69°, and 107.88°, respectively. The Scheffe's post hoc test demonstrated that contact angles were significantly different between groups (P < .01) (Table V).
The heat-cured acrylic denture base materials (Vertex RS, Lang) had a significantly lower contact angle than silicone relining materials over all three storage conditions (P < .01).
Wettability of the denture base and denture relining materials are important, because it is suggested that saliva will spread over their surfaces, forming a lubrication layer for extra comfort. Reduced wettability will have disadvantage in terms of comfort and retention. Contact angles are the characteristic constants of liquid/solid systems and provide valuable information on the surface energies of solids.15
Relining can be achieved either by laboratory procedures with heat-cured acrylic resin or by chairside procedures with self-cured acrylic resin or silicones. Acrylic denture base materials are usually supplied in powder/liquid form with the powder consisting of a higher methacrylate polymer (usually polyethyl methacrylate) and a liquid consisting of a higher methacrylate monomer (eg, ethyl, n-butyl). In addition, there is a plasticizer (commonly phthalate).16 These materials undergo 2 processes when immersed in water with leaching of plasticizers and other soluble materials into the water and water imbibition by the polymer.
Due to the polar nature of the resin molecules, polymethyl methacrylate will absorb water. This water sorption is typically 1 - 2% by weight. As a result, the physical and mechanical properties of the materials change with time in the patient's mouth.17,18 Softness is primarily affected by the leaching of plasticizer with a consequent hardening of the material, limiting its usefulness.9,19 The plasticiser acts as a lubricant for the polymer chains, making it easier for them to slide past one another, allowing the material to deform more easily and giving it a lower elastic modulus. A resin matrix that is polymerized to a greater degree would have less water sorption, because the greater resin density reduces diffusion of water into the matrix.20
Wright investigated the clinical success of soft lining materials and reported that the most common reasons for replacement were failure of adhesion between the lining and denture, hardening or roughening of the lining, and discoloration.21 Acrylic denture base materials demonstrate greater abrasion resistance and bond strength, but lose elasticity and dimensional stability as the plasticizing agent leaches from the denture relining materials. 8,22
A laboratory-processed denture relining materials exhibits more complete polymerization than a chairside denture relining materials, providing increased resistance to solubility in oral fluids and improved physical and mechanical properties.7,10 In the present study, Vertex RS and Lang which are heat-cured acrylic resins showed higher wettability than other materials. Wettability of denture relining materials indicate the degree of salivary lubricating effect which promotes denture retention and patient's comfort.
The silicone materials are quick, clean and easy to use being supplied in a form which allows direct injection of the automixed material onto the prepared denture fitting surface. Silicone materials demonstrate greater resistance to change in physical properties when exposed to solid or liquid chemical components and are more elastic. A drawback of silicone materials is their greater propensity for bond failure between the denture relining materials and the acrylic denture base. Slicone relining materials are the best materials for maintaining resiliency over time and resisting initial water absorption. Resilient liners are viscoelastic materials; as they age and absorb water, they may become more elastic and less viscous, which can lead to failure.23 Silicone materials are composed of polymers of dimethyl siloxane, a viscous liquid crosslinked with good elastic properties. The material is solidified by a crosslinking process rather than by a polymerization process, as the material is already a polymer. This crosslinking can be achieved either by heat, using benzoyl peroxide, or at room temperature, using tetraethylsilicate.
A major limitation of silicone materials is hydrophobicity. 24,25 The hydrophobic properties are related to the material' s chemical structure, which contains hydrophobic, aliphatic hydrocarbon groups surrounding the siloxane bond.26,27 Silicone materials are especially resistant to initial water absorption.28 In general, the silicone and natural rubber materials demonstrate a significantly poorer wettability than polymethyl methacrylate. Therefore, these materials will cause frictional damage to the oral mucosa if saliva flow is reduced.29,30 In this study, silicones showed the highest contact angle.
High water sorption and solubility, and a gradual hardening due to plasticiser leaching out, are the main drawbacks of plasticized acrylics.31 Silicone materials have a longer duration of resilience, but have always been criticized for lacking sufficient adhesion to acrylic denture base materials.32 Hydrophobicity of the silicone materials reduces water sorption, but simultaneously inhibits good affinity to the supporting tissues.33 The clinical suitability of these results should be tested further by in vivo studies. It may then be possible to correlate the results of this with clinical applications. It will also be informative to study the effect of different surface treatments on the wettability of denture relining materials. Also, surface treatment techniques to improve the bond strength of denture base resin and lining material need to be more developed and investigated.
This study demonstrated that conventional heat-cured PMMA denture relining materials are more wettable than other materials, therefore, it can be suggested that the heat-cured PMMA denture relining materials, is a good choice as denture relining material.
Within the limitations of this in vitro study, the following conclusions were drawn:
1. Contact angles of materials tested both in air and water storage increased in the following order: Group 1 (PMMA), Group 2 (PEMA), Group 3 (Silicone).
2. Wettability of denture relining materials except Rebase II and Mollosil® plus were increased after 24 hours of water storage at 37 ± 2℃.
3. Heat-cured PMMA denture base resin showed the highest wettability, therefore, it can be suggested that heat-cured PMMA resin should provide superior denture retention and patient comfort to self-cured PEMA and silicone denture relining material.
Figures and Tables
 | Fig. 1Schematic illustration of high-resolution Drop Shape Analysis System. A. Table, B. Specimen, C. Liquid Syringe System, D. Liquid Container, E. Light, F. High-resolution Video Camera, G. Computer, H. Monitor. |
References
1. Kawano F, Tada N, Nagal K, Matsuomoto N. Influence of soft lining materials on pressure distribution. J Prosthet Dent. 1991. 65:567–575.
2. Haywood J, Basker RM, Watson CJ, Wood DJ. A comparison of three hard chairside denture reline materials. Part I. Clinical evaluation. Eur J Prosthodont Restor Dent. 2003. 11:157–163.
3. Matsumura H, Tanoue N, Kawasaki K, Atsuta M. Clinical evaluation of a chemically cured hard denture relining material. J Oral Rehabil. 2001. 28:640–644.
4. Arima T, Murata H, Hamada T. Analysis of composition and structure of hard autopolymerizing reline resins. J Oral Rehabil. 1996. 23:346–352.
5. Wright PS. The success and failure of denture soft-lining materials in clinical use. J Dent. 1984. 12:319–327.
6. Barsby MJ, Braden MJ. A hydrophilic denture base resin. J Dent Res. 1979. 58:1581–1584.
7. Qudah S, Harrison A, Huggett R. Soft lining materials in prosthetic dentistry: A review. Int J Prosthodont. 1990. 3:477–483.
8. Ellis B, Lamb DJ, McDonald MP. A study of the composition and diffusion characteristics of a soft liner. J Dent. 1979. 7:133–140.
9. Jones DW, Sutow EJ, Hall GC, Tobin WM, Graham BS. Dental soft polymers, plasticizer composite and leachability. Dent Mater. 1988. 4:1–7.
10. Craig RG, Gibbons P. Properties of resilient denture liners. J Am Dent Assoc. 1961. 63:382–390.
11. Monsénégo P, Baszkin A, Costa ML, Lejoyeux J. Complete denture retention. Part II: Wettability studies on various acrylic resin denture base materials. J Prosthet Dent. 1989. 62:308–312.
12. Wright PS. Soft lining materials: their status and prospects. J Dent. 1976. 4:247–256.
13. Kwok D, Gietzelt T, Grundke K, Jacobash H, Neumann A. Contact angle measurements and contact angle interpretation. 1. Contact angle measurements by axisymmetric drop shape analysis and a goniometer sessile drop technique. Langmuir. 1997. 13:2880–2894.
14. Good RJ. Mittal KL, editor. Contact angle, wetting, and adhesion a critical review. Contact angle, wettability and adhesion. 1993. Utrecht, The Netherlands: VSP;3–36.
15. Anusavice KJ. Phillip's science of dental materials. 1996. 10th ed. Philadelphia, PA: Saunders;28–29.
16. Wright PS. Composition and properties of soft lining materials for acrylic dentures. J Dent. 1981. 9:210–223.
17. Kalachandra S, Turner DT. Water sorption of plasticized denture acrylic lining material. Dent Mater. 1989. 5:161–164.
18. Parker S, Martin D, Braden M. Soft acrylic resin materials containing a polymerizable plasticizer I: Mechanical properties. Biomaterials. 1998. 19:1695–1701.
19. Kazanji MNM, Watkinson AC. Influence of thickness, boxing and storage on the softness of resilient denture lining materials. J Prosthet Dent. 1988. 59:677–680.
20. Parr GR, Rueggeberg FA. Physical-property comparison of a chairside- or laboratory-polymerized permanent soft-liner during 1 year. J Prosthodont. 1999. 8:92–99.
21. Jepson NJA, McCabe JF, Storer R. The clinical serviceability of two permanent denture soft linings. Br Dent J. 1994. 177:11–16.
22. Combe EC, Burke FJT, Douglas WH. Dental Biomaterials. 1999. Boston: Kluwer Academic;396–400.
23. Emmer TJ Jr, Emmer TJ Sr, Vaidynathan J, Vaidynathan TK. Bond strength of permanent soft denture liners bonded to the denture base. J Prosthet Dent. 1995. 74:595–601.
24. Boening KW, Walter MH, Schuette U. Clinical significance of surface activation of silicone impression materials. J Dent. 1998. 26:447–452.
25. Mandikos MN. Polyvinylsiloxane impression materials: an update on clinical use. Aust Dent J. 1998. 43:428–434.
26. McMurry J. Fundamentals of organic chemistry. 1998. 4th ed. Pacific Grove, CA: Brooks/Cole Publishing Co.;36–45.
27. Anusavice KJ. Phillips' science of dental materials. 2003. 11th ed. Philadelphia, PA: Saunders;205–231.
28. Villar A, Pesun IJ, Brosky ME, Fines C, Hodges JS, DeLong R, Lai JH. Clinical evaluation of a new resilient denture liner. part 1: Compliance and color evaluation. J Prosthodont. 2003. 12:82–89.
29. Veres EM, Wolfaardt JF, Becker PJ. An evaluation of the surface characteristics of a facial prosthetic elastomer. Part III: wettability and hardness. J Prosthet Dent. 1990. 63:466–471.
30. Kawano F, Dootz ER, Koran A III, Craig RG. Sorption and solubility of 12 soft denture liners. J Prosthet Dent. 1994. 72:393–398.
31. Jones DW, Hall GC, Sutow EJ, Langman MF, Robertson KN. Chemical and molecular weight analyses of prosthodontic soft polymers. J Dent Res. 1991. 70:874–879.
32. O'Brien WJ. Dental materials and their selection. 1997. Chicago: Quintessence Publishing Co.;90.
33. Waters MG, Jagger RG, Polyzois GL. Wettability of silicone rubber maxillofacial prosthetic materials. J Prosthet Dent. 1999. 81:439–443.




 PDF
PDF ePub
ePub Citation
Citation Print
Print






 XML Download
XML Download