1. Guzman RE, Evans MG, Bove S, Morenko B, Kilgore K. Monoiodoacetate-induced histologic changes in subchondral bone and articular cartilage of rat femorotibial joints: an animal model of osteoarthritis. Toxicol Pathol. 2003; 31(6):619–624. PMID:
14585729.

2. Bove SE, Calcaterra SL, Brooker RM, Huber CM, Guzman RE, Juneau PL, Schrier DJ, Kilgore KS. Weight bearing as a measure of disease progression and efficacy of anti-inflammatory compounds in a model of monosodium iodoacetate-induced osteoarthritis. Osteoarthritis Cartilage. 2003; 11(11):821–830. PMID:
14609535.

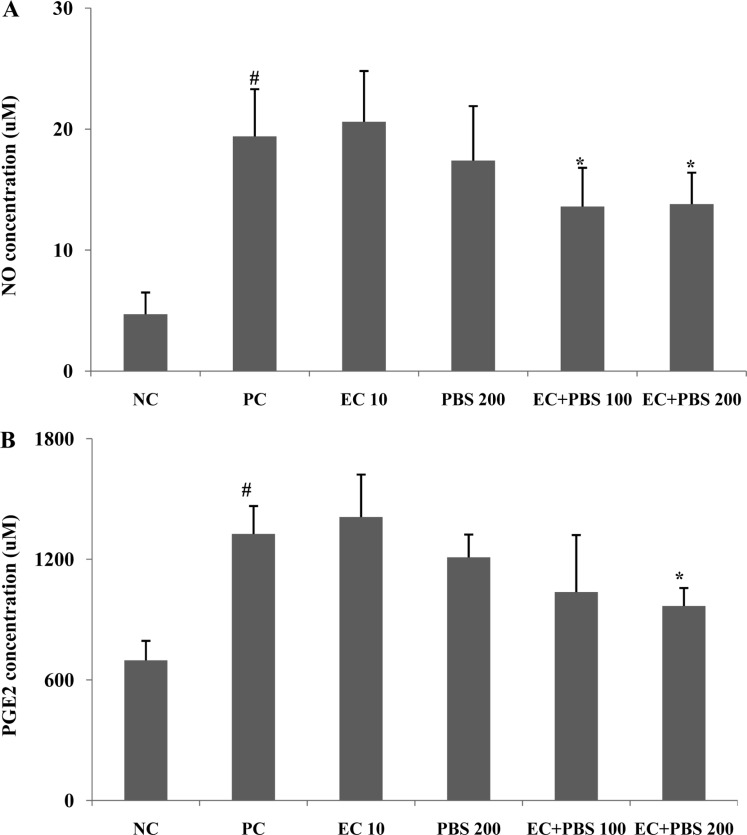
3. Studer R, Jaffurs D, Stefanovic-Racic M, Robbins PD, Evans CH. Nitric oxide in osteoarthritis. Osteoarthritis Cartilage. 1999; 7(4):377–379. PMID:
10419772.

4. Herrington C, Hall PA. Molecular and cellular themes in inflammation and immunology. J Pathol. 2008; 214(2):123–125. PMID:
18161749.

5. Bove SE, Calcaterra SL, Brooker RM, Huber CM, Guzman RE, Juneau PL, Schrier DJ, Kilgore KS. Weight bearing as a measure of disease progression and efficacy of anti-inflammatory compounds in a model of monosodium iodoacetate-induced osteoarthritis. Osteoarthritis Cartilage. 2003; 11(11):821–830. PMID:
14609535.

6. Woo YJ, Joo YB, Jung YO, Ju JH, Cho ML, Oh HJ, Jhun JY, Park MK, Park JS, Kang CM, Sung MS, Park SH, Kim HY, Min JK. Grape seed proanthocyanidin extract ameliorates monosodium iodoacetate-induced osteoarthritis. Exp Mol Med. 2011; 43(10):561–570. PMID:
21795829.

7. Im HJ, Kim JS, Li X, Kotwal N, Sumner DR, van Wijnen AJ, Davis FJ, Yan D, Levine B, Henry JL, Desevre J, Kroin JS. Alteration of sensory neurons and spinal response to an experimental osteoarthritis pain model. Arthritis Rheum. 2010; 62(10):2995–3005. PMID:
20556813.

8. Kim HY, Lee ES, Jeong JY, Choi JH, Choi YS, Han DJ, Lee MA, Kim SY, Kim CJ. Effect of bamboo salt on the physicochemical properties of meat emulsion systems. Meat Sci. 2010; 86(4):960–965. PMID:
20826069.

9. Zhao X, Jung OS, Park KY. Alkaline and antioxidant effects of bamboo salt. J Korean Soc Food Sci Nutr. 2012; 41(9):1301–1304.

10. Shin HY, Lee EH, Kim CY, Shin TY, Kim SD, Song YS, Lee KN, Hong SH, Kim HM. Anti-inflammatory activity of Korean folk medicine purple bamboo salt. Immunopharmacol Immunotoxicol. 2003; 25(3):377–384. PMID:
19180800.

11. Zhao X, Song JL, Kil JH, Park KY. Bamboo salt attenuates CCl4-induced hepatic damage in Sprague-Dawley rats. Nutr Res Pract. 2013; 7(4):273–280. PMID:
23964314.

12. Zhao X, Deng X, Park KY, Qiu L, Pang L. Purple bamboo salt has anticancer activity in TCA8113 cells in vitro and preventive effects on buccal mucosa cancer in mice in vivo. Exp Ther Med. 2013; 5(2):549–554. PMID:
23403521.

13. Kim SH, Kang SY, Jung KK, Kim TG, Han HM, Rheu HM, Moon A. Characterization and anti-gastric ulcer activity of bamboo salt. J Food Hyg Saf. 1998; 13:252–257.
14. Jhun HJ, Ahn K, Lee SC. Estimation of the prevalence of osteoarthritis in Korean adults based on the data from the fourth Korea national health and nutrition examination survey. Anesth Pain Med. 2010; 5(3):201–206.
15. Henrotin Y, Kurz B. Antioxidant to treat osteoarthritis: dream or reality? Curr Drug Targets. 2007; 8(2):347–357. PMID:
17305512.

16. Dunham J, Hoedt-Schmidt S, Kalbhen DA. Prolonged effect of iodoacetate on articular cartilage and its modification by an anti-rheumatic drug. Int J Exp Pathol. 1993; 74(3):283–289. PMID:
8334078.
17. Choi EA, Park HY, Yoo HS, Choi YH. Anti-inflammatory effects of egg white combined with chalcanthite in lipopolysaccharide-stimulated BV2 microglia through the inhibition of NF-êB, MAPK and PI3K/Akt signaling pathways. Int J Mol Med. 2013; 31(1):154–162. PMID:
23128312.

18. Janusz MJ, Hookfin EB, Heitmeyer SA, Woessner JF, Freemont AJ, Hoyland JA, Brown KK, Hsieh LC, Almstead NG, De B, Natchus MG, Pikul S, Taiwo YO. Moderation of iodoacetateinduced experimental osteoarthritis in rats by matrix metalloproteinase inhibitors. Osteoarthritis Cartilage. 2001; 9(8):751–760. PMID:
11795995.

19. Choi EA, Kim KH, Yoo BC, Yoo HS. Induction of apoptotic cell death by egg white combined-chalcanthite on NCI-H460 human lung cancer cells. J Korean Pharmacopuncture Inst. 2009; 12(3):49–59.

20. Gencosmanoglu BE, Eryavuz M, Dervisoglu S. Effects of some nonsteroidal anti-inflammatory drugs on articular cartilage of rats in an experimental model of osteoarthritis. Res Exp Med (Berl). 2001; 200(3):215–226. PMID:
11426673.
21. Natchus MG, Bookland RG, De B, Almstead NG, Pikul S, Janusz MJ, Heitmeyer SA, Hookfin EB, Hsieh LC, Dowty ME, Dietsch CR, Patel VS, Garver SM, Gu F, Pokross ME, Mieling GE, Baker TR, Foltz DJ, Peng SX, Bornes DM, Strojnowski MJ, Taiwo YO. Development of new hydroxamate matrix metalloproteinase inhibitors derived from functionalized 4-aminoprolines. J Med Chem. 2000; 43(26):4948–4963. PMID:
11150165.

22. Mankin HJ, Dorfman H, Lippiello L, Zarins A. Biochemical and metabolic abnormalities in articular cartilage from osteo-arthritic human hips. II. Correlation of morphology with biochemical and metabolic data. J Bone Joint Surg Am. 1971; 53(3):523–537. PMID:
5580011.
23. Thomas CM, Fuller CJ, Whittles CE, Sharif M. Chondrocyte death by apoptosis is associated with cartilage matrix degradation. Osteoarthritis Cartilage. 2007; 15(1):27–34. PMID:
16859932.

24. Goldring SR, Goldring MB. The role of cytokines in cartilage matrix degeneration in osteoarthritis. Clin Orthop Relat Res. 2004; (427 Suppl):S27–S36. PMID:
15480070.

25. Zamli Z, Sharif M. Chondrocyte apoptosis: a cause or consequence of osteoarthritis? Int J Rheum Dis. 2011; 14(2):159–166. PMID:
21518315.

26. Goldring MB, Otero M, Tsuchimochi K, Ijiri K, Li Y. Defining the roles of inflammatory and anabolic cytokines in cartilage metabolism. Ann Rheum Dis. 2008; 67(Suppl 3):iii75–iii82. PMID:
19022820.

27. Carames B, Lopez-Armada MJ, Cillero-Pastor B, Lires-Dean M, Vaamonde C, Galdo F, Blanco FJ. Differential effects of tumor necrosis factor-alpha and interleukin-1beta on cell death in human articular chondrocytes. Osteoarthritis Cartilage. 2008; 16(6):715–722. PMID:
18054255.
28. Abramson SB, Attur M. Developments in the scientific understanding of osteoarthritis. Arthritis Res Ther. 2009; 11(3):227. PMID:
19519925.

29. Pelletier JP, DiBattista JA, Roughley P, McCollum R, Martel-Pelletier J. Cytokines and inflammation in cartilage degradation. Rheum Dis Clin North Am. 1993; 19(3):545–568. PMID:
8210574.

30. Guerne PA, Sublet A, Lotz M. Growth factor responsiveness of human articular chondrocytes: distinct profiles in primary chondrocytes, subcultured chondrocytes, and fibroblasts. J Cell Physiol. 1994; 158(3):476–484. PMID:
8126071.

31. Hashimoto J, Yoshikawa H, Takaoka K, Shimizu N, Masuhara K, Tsuda T, Miyamoto S, Ono K. Inhibitory effects of tumor necrosis factor alpha on fracture healing in rats. Bone. 1989; 10(6):453–457. PMID:
2624827.

32. Webb GR, Westacott CI, Elson CJ. Chondrocyte tumor necrosis factor receptors and focal loss of cartilage in osteoarthritis. Osteoarthritis Cartilage. 1997; 5(6):427–437. PMID:
9536291.

33. Nam SY, Oh HA, Choi Y, Park KY, Kim HM, Jeong HJ. Inhibition of IL-32 signaling by bamboo salt decreases proinflammatory responses in cellular models of allergic rhinitis. J Med Food. 2014; 17(9):939–948. PMID:
25089715.

34. Carames B, Lopez-Armada MJ, Cillero-Pastor B, Lires-Dean M, Vaamonde C, Galdo F, Blanco FJ. Differential effects of tumor necrosis factor-alpha and interleukin-1beta on cell death in human articular chondrocytes. Osteoarthritis Cartilage. 2008; 16(6):715–722. PMID:
18054255.
35. Stadler J, Stefanovic-Racic M, Billiar TR, Curran RD, McIntyre LA, Georgescu HI, Simmons RL, Evans CH. Articular chondrocytes synthesize nitric oxide in response to cytokines and lipopolysaccharide. J Immunol. 1991; 147(11):3915–3920. PMID:
1658153.
36. Amin AR, Attur M, Patel RN, Thakker GD, Marshall PJ, Rediske J, Stuchin SA, Patel IR, Abramson SB. Superinduction of cyclooxygenase-2 activity in human osteoarthritis-affected cartilage. Influence of nitric oxide. J Clin Invest. 1997; 99(6):1231–1237. PMID:
9077531.

37. Rahmati M, Mobasheri A, Mozafari M. Inflammatory mediators in osteoarthritis: A critical review of the state-of-the-art, current prospects, and future challenges. Bone. 2016; 85:81–90. PMID:
26812612.

38. Notoya K, Jovanovic DV, Reboul P, Martel-Pelletier J, Mineau F, Pelletier JP. The induction of cell death in human osteoarthritis chondrocytes by nitric oxide is related to the production of prostaglandin E2 via the induction of cyclooxygenase-2. J Immunol. 2000; 165(6):3402–3410. PMID:
10975859.

39. Barve RA, Minnerly JC, Weiss DJ, Meyer DM, Aguiar DJ, Sullivan PM, Weinrich SL, Head RD. Transcriptional profiling and pathway analysis of monosodium iodoacetate-induced experimental osteoarthritis in rats: relevance to human disease. Osteoarthritis Cartilage. 2007; 15(10):1190–1198. PMID:
17500014.

40. Lee SW, Song YS, Shin SH, Kim KT, Park YC, Park BS, Yun I, Kim K, Lee SY, Chung WT, Lee HJ, Yoo YH. Cilostazol protects rat chondrocytes against nitric oxide-induced apoptosis in vitro and prevents cartilage destruction in a rat model of osteoarthritis. Arthritis Rheum. 2008; 58(3):790–800. PMID:
18311796.





 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download