Abstract
Dendrobium moniliforme (L.) Sw., an herb of the Orchidaceae family, has long been used in traditional medicine to strengthen bones, nourish the stomach, and promote the production of bodily fluid. Recently, polysaccharides isolated from Dendrobium have been used in functional foods and nutraceutical products. A traditional method to process Dendrobium is to soak fresh stems in an ethanol solution, which is the most important factor to ensure high yields of aqueous-extractable polysaccharides. The present study was carried out to investigate the potential acute toxicity of D. moniliforme aqueous extract (DMAE), by a single oral dose in Sprague-Dawley rats. The test article was orally administered once by gavage to male and female rats at doses of 0, 2,500, and 5,000 mg/kg body weight (n=5 male and female rats for each dose). Throughout the study period, no treatment-related deaths were observed and no adverse effects were noted in clinical signs, body weight, food consumption, serum biochemistry, organ weight, or gross findings at any dose tested. The results show that a single oral administration of DMAE did not induce any toxic effects at a dose below 5,000 mg/kg in rats, and the minimal lethal dose was considered to be over 5,000 mg/kg body weight for both sexes. With respect to cytotoxicity, the cell viability of human embryonic kidney (HEK293) cells was less than 50% when the cells were treated with 10 mg/mL aqueous extract for 24 h.
Traditional herbal medicines are generally regarded as safe treatments due to the historical evidence regarding various indications in ancient medical texts, however, in practice, this is not always the case. Efficacy is often suspected on the grounds that their traditional remedies contain only very low concentrations of active ingredients and basically rely on magical energetic principles [12]. Therefore, consumers still have questions regarding the efficacy and safety of traditional herbal medicines.
Dendrobium moniliforme (L.) Sw. (Seok-Gok in Korea) is the second largest genus in the family of Orchidaceae [3]. There are 2 to 10 entities in this complex, distributed throughout Eastern Asia and the Himalayan regions such as Korea, Japan, China, Nepal, India, and the alpine regions [456]. Dendrobium herb is a well-known, traditional medicine that is used for the various biological activities including immuno-modulatory, anti-tumor, anti-diabetic and antioxidant properties [7]. Dendrobium extracts have been shown to display neuroprotective effects on oxygen-glucose deprivation/reperfusion neuronal injury in vitro [8]. In China, Dendrobium plants have been used as ingredients for nutraceutical beverages and food products for thousands of years [9]. Thin-layer chromatography (GLC), gas chromatography (GC) and gas chromatography–mass spectrometry (GC-MS) are commonly used methods for identification and quantification of the monosaccharides in Dendrobium polysaccharides [7]. Dendrobium plants are rich in polysaccharides, and the detailed structure of the purified O-acetyl glucomannan fraction (designated as DMP2a-1) isolated from D. moniliforme has been reported [1011]. Another fraction (designated as DMP4a-1) of D. moniliforme polysaccharides has been reported to have an average molecular weight of 3049 Da [12]. Recent studies have reported that polysaccharides from Dendrobium spp. usually consist of glucose, galactose, mannose, xylose, arabinose, rhamnose, glucuronic acid, and galacturonic acid [13141516]. A traditional method to process Dendrobium herbs is to soak fresh stems in an ethanol solution and then dry them in the sun [17]. This method can significantly increase the yield of the hot aqueous-extractable polysaccharide in the processed Dendrobium herbs [18].
As part of the safety evolution studies of the test article, a single oral dose toxicity study was performed in Sprague-Dawley rats. There were no reports dealing with the toxicological aspects of D. moniliforme aqueous extract (DMAE), not even basic single dose toxicities in rodents. The objective of the present study, therefore, was to obtain primary safety information regarding D. moniliforme aqueous extract, and further clarify its safety for clinical use. In order to observe the minimal lethal dose (LD10), test article was orally administered once to male and female Sprague-Dawley rats at dose levels of 0, 2,500, and 5,000 mg/kg body weight according to the recommendations by the KFDA and OECD guidelines [1920].
Twenty-four Sprague-Dawley rats of each sex were obtained from the SAMTAKO Inc. (Osan, Korea) at 5 weeks of age, and used following 2 weeks of quarantine and acclimatization. One animal per cage was housed in a room maintained at a temperature of 21.1~23.5℃ and a relative humidity of 32.3~67.8%, with artificial lighting from 07:00 to 19:00 (150~300 Lux) and 10~15 air changes per hour. Only healthy animals were assigned to the study. The animals were kept in solid-bottomed polycarbonate cages (W 260×L 420×H 180 mm) and allowed sterilized tap water and commercial rodent chow (Altromin 1314 feed, Altromin, Lage, Germany) ad libitum. The animals were maintained in accordance with the Guide for the Care and Use of Laboratory Animals [21].
Dendrobium moniliforme (L.) Sw. was purchased from the Seok-Gok plantation of Jincheon (Chungbuk, Korea) and identified by the National Development Institute for Traditional Korean Medicine as Dendrobium moniliforme (L.) Sw. The D. moniliforme (3 kg) was extracted twice by decoction with distilled water (30 L) for 3 h at 95℃, and the solution was filtered with a 100 mesh sieve. The D. moniliforme aqueous extract (DMAE) freeze-dried powder was concentrated in vacuo (5-10 hPa at 50~60℃) and lyophilized using a freeze-drying system (NE-10001V, Eyela, Tokyo, Japan). Total acquired DMAE powder was 66 g (yield 2.2%). The test article was prepared immediately before treatment by suspending in sterile aqueous solution for injection. The dosing solutions for the lower dose groups were prepared by a stepwise dilution of the high-dose solution.
In a dose-range finding study, there were no dead animals at a dose of 2,500 mg/kg or below. Based on these results, a dose of 2,500 mg/kg, which was the nontoxic baseline, was selected as the medium dose in the present study. A dose of 5,000 mg/kg was selected as the high dose, using a common ratio of 2. In addition, a vehicle control group was added to determine the effects of the vehicle. The high dose selected in the present study corresponds to approximately 2.5 times that of the limit test dose recommended by the OECD Guidelines for the Testing of Chemicals [20]. Five healthy animals at 7 weeks of age were randomly assigned to three experimental groups. Body weight ranges at the beginning of dosing were 197~224 g for males and 149~168 g for females.
The rats were fasted overnight (approximately 16 h, water was not restricted) prior to dosing, and the test article was administered orally by gavage. The test article was administered singly, at dose levels of 2,500 and 5,000 mg/kg. The application volume (20 mL/kg body weight) was calculated according to the fasted body weight on the treatment day. The control rats received an equivalent volume of sterilized distilled water alone. After the test article was administered, the rats were fasted for a further 4 h.
Clinical signs and mortality were observed continuously for the first 1 h after dosing, and every hour for 6 h. Each animal was observed daily throughout the entire 15-day experimental period. Abnormal type and severity of signs, as well as the observation day and time, were recorded.
Individual body weights of the animals were measured on the day of dosing (Day 0) shortly before test article administration and on days 1, 3, 7, 14, and 15 after the treatment. In addition, to reduce the individual body weight differences of the animals at initial dosing, body weight gains during Day -1 (grouping day) to Day 1, Day -1 to Day 7, Day 7 to Day 14, and Day -1 to Day 14 were also calculated.
Food consumption was measured on days 1, 3, 7, and 14 after the treatment. The amount of food was measured before they were assigned to each cage, and food remaining the next day was measured in order to calculate the difference, which was regarded as daily food consumption (g/head/day).
During the necropsy, more than 3 mL blood was collected into a 5-mL Vacutainer tube (SST™ tube, Becton Dickinson, Franklin Lakes, NJ) containing a clot activator. The blood was coagulated by maintaining it at room temperature for 30~40min followed by centrifugation (Hanil Combi-514R, Seoul, Korea) for 10 min. The following parameters were measured with a serum biochemistry analyzer (FUJI DRI-CHEM 4000i, FUJI, Tokyo, Japan): aspartate aminotransferase (AST), alanine aminotransferase (ALT), alkaline phosphatase (ALP), lactate dehydrogenase (LDH), gamma glutamyl transpeptidase (GGT), blood urea nitrogen (BUN), creatinine (CREA), total bilirubin (TBIL), albumin (ALB), total protein (TP), total cholesterol (TCHO), triglycerides (TG), creatine phosphokinase (CPK), and calcium (Ca2+).
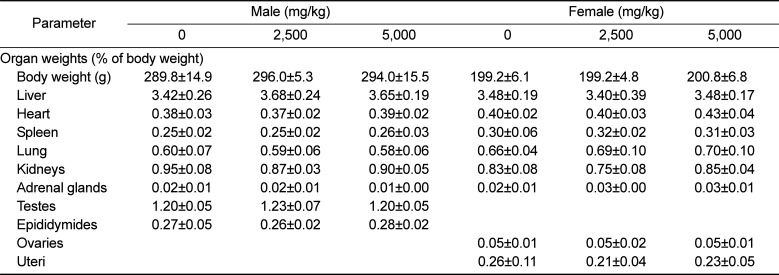
Prior to the scheduled necropsy, all animals were fasted overnight (for 16~20 h). After anesthesia was confirmed, blood was taken from the posterior vena cava for serum biochemistry. The abdominal aorta and posterior vena cava were cut for sacrifice. All organs of the body surface, subcutis, head, and all internal organs of the abdominal and thoracic cavities were observed grossly. Subsequently, the liver, heart, spleen, lung, kidneys, adrenal gland, ovaries, uteri, testes, and epididymides were removed and weighed using an electronic balance (EX224G, Ohaus, Florham Park, NJ), and all paired organs were measured separately. The absolute organ weights were converted to relative organ weights based on the organ-to-fasted body weight ratio (%).
The human embryonic kidney cell line (HEK293) was purchased from the Korean Cell Line Bank for Biological Sciences (KCLB, Seoul, Korea). 3-(4,5-dimethylthiazol-2-yl)-2,5-diphenyltetrazolium bromide (MTT) was obtained from Sigma (St. Louis, MO). Roswell Park Memorial Institute (RPMI) 1640 medium, phosphate-buffered saline (PBS), fetal bovine serum, penicillin/streptomycin, and trypan blue were purchased from Invitrogen Molecular Probes (Carlsbad, CA). The proliferation of HEK293 cells was measured using a colorimetric MTT assay. HEK293 cells were seeded onto a 96-well plate at a density of 1.0×104 cells/well. Briefly, the cells were incubated with different concentrations of samples for 24 h, followed by the addition of 20 µL MTT solution to each well at a final concentration of 0.5 mg/mL in PBS (pH 7.4). The plates were incubated for an additional 4 h at 37℃ in the dark. Following removal of the medium, the dye crystals were dissolved in 100 µL dimethyl sulfoxide, and the absorbance of each well was measured at 570 nm using a microplate reader (Infinite 200 pro, TECAN Ltd., Mannedorf, Switzerland). The cell viability was expressed as a percentage of the ratio of absorbance between treated and untreated groups.
Data are presented as the mean±standard deviation. Body weight, food consumption, serum biochemistry, absolute and relative organ weights, and cell viability were compared by a Student's t-test using the SPSS program (SPSS version 18.0, Chicago, IL). Since no mortality was observed in the present study, statistical analysis for the calculation of the LD50 value was not performed.
No animals of either sex were found dead following treatment with the test item during the testing period. Therefore, it was estimated that the minimal lethal dose of the test article is over 5,000 mg/kg in both sexes. In addition, no DMAE treatment-related abnormal clinical signs were observed during the observation period, regardless of sex (data not shown).
No significant changes were observed in body weight or weight gains during the experimental period (Table 1).
Blood urea nitrogen (BUN) in males of the 2,500 and 5,000 mg/kg groups were increased significantly (P<0.05) when compared with that in the vehicle control group. No significant differences in females were observed between the groups (Table 2).
At necropsy on day 15 following treatment, no treatment-related effects were found in any dose group (data not shown).
HEK293 cells were incubated with DMAE at concentrations of 1.25, 2.5, 5, 6, 7, 8, 9, and 10 mg/mL for 24 h. Cell death (cytotoxicity) was observed at concentrations above 6mg/mL. The IC50 value (concentration inducing 50% cell death) was found to be 10 mg/mL (Figure 2).
Dendrobium plants are the second largest genus in the Orchidaceae family [3], consisting of approximately 1100 species, which are mainly distributed in the subtropical and tropical regions of Asia and Oceania [22]. Starch granules have been shown by scanning electron microscopy to be present in the stem vascular bundles of 8 Dendrobium species, namely, Dendrobium moniliforme, D. tosaense, D. cumulatum, D. linawianum, D. aurantiacum, D. huoshanense, D. nindii, and D. officinale [23]. Since ancient times, many Dendrobium plants have been used as ingredients for nutraceutical beverages and food products [9]. A traditional method to process Dendrobium herbs is to soak fresh stems in an ethanol solution [17].
The present study was conducted to investigate the potential acute toxicity of an aqueous extract of dendrobium moniliforme (L.) Sw., DMAE, administered by gavage to Sprague-Dawley rats at dose levels of 0, 2,500, and 5,000 mg/kg body weight. The results show that a single oral dose of DMAE did not cause any adverse effects on mortality rate, clinical signs, body weight change, food consumption, serum biochemistry, organ weights, or necropsy finding in rats.
Food consumption in males of the 5,000 mg/kg group increased significantly on Day 1 after dosing compared with that in the vehicle control group. Both food consumption and body weight gain in all test substance-treated groups were shown to have an increasing tendency on Day 1 after dosing compared with the control group. The increased food consumption and body weight were not considered to be toxicologically significant, since they were within the limits of normal biological variation [242526]. However, these observations suggest the need for further identification of an increasing effect through repeated dose studies, since similar results have been reported in other studies that Dendrobium extract significantly increased body weight in hypertensive and diabetic rats [2728]. Dendrobium plants are rich in polysaccharides, and contain nutrients such as protein, amino acids, Ca, Mg, P, and other inorganic elements [10].
The significant increase in blood urea nitrogen (BUN) in the males of the 2,500 and 5,000 mg/kg groups was not considered toxicologically significant due to the fact that there were no changes detected in the females, and the values were within the normal range of laboratory reference data [24]. However, further studies are required to identify histopathology changes after repeated administration of DMAE.
No toxic effects were detected in rats following ingestion of D. Nobile extract at a dose level of 10 g/kg body weight [29]. Furthermore, no toxic effects were detected in mice or rats following ingestion of D. Candidum extract at a dose level of 4 g/kg/day for thirty days [30]. These studies consistently suggest the safety of Dendrobium herb administration, and are in accordance with the present study. In the case of normal mouse bone marrow cells, the ethanolic extract of Dendrobium formosum did not induce cytotoxicity, since an IC50 value was not obtained even with a higher dose of 2 mg/mL [31].
With respect to cytotoxicity, exposure of DMAE was investigated in cultured human embryonic kidney (HEK293) cells. Cell death was observed with concentrations above 6 mg/mL. Moreover, the cell viability of HEK293 cells was less than 50% following treatment with 10 mg/mL aqueous extract for 24 h. The results of the present study show that exposure of HEK293 cells to DMAE produced a dose-dependent cytotoxicity as revealed by an MTT assay.
Based on the results of the present study, it can be concluded that a single oral dose of DMAE did not induce any adverse effects in Sprague-Dawley rats at a dose level of 5,000 mg/kg or less, and that the minimal lethal dose (LD10) can be considered to be over 5,000 mg/kg body weight for both sexes.
Acknowledgments
This study was supported by a grant from the Joint Research Project (Project Number: PJ009470), Rural Development Administration (RDA), Republic of Korea.
References
1. Firenzuoli F, Gori L. Herbal medicine today: clinical and research issues. Evid Based Complement Alternat Med. 2007; 4(S1):37–40. PMID: 18227931.

2. Jordan SA, Cunningham DG, Marles RJ. Assessment of herbal medicinal products: challenges, and opportunities to increase the knowledge base for safety assessment. Toxicol Appl Pharmacol. 2010; 243(2):198–216. PMID: 20018204.

3. Puchooa D. Comparison of different culture media for the in vitro culture of Dendrobium (Orchidaceae). Int J Agric Biol. 2004; 6:884–888.
4. Garay LA, Sweet HR. Orchids of Southern Ryukyu Islands. Cambridge: Botanical Museum, Harvard University;1974. p. 180.
5. Pearce NR, Cribb PJ. The Orchids of Bhutan. Huddersfield, United Kingdom: Charlesworth Group;2002. p. 195–212.
6. Tsi ZH. Tsi ZH, editor. Flora Reipublicae Popularis Sinicae Tomus. vol. 19. Beijing: Sciences Press;1999. p. 339–420.
7. Xing X, Cui SW, Nie S, Phillips GO, Goff HD, Wang Q. A review of isolation process, structural characteristics, and bioactivities of water-soluble polysaccharides from Dendrobium plants. Bioact Carbohyd Diet Fibre. 2013; 1:131–147.
8. Wang Q, Gong Q, Wu Q, Shi J. Neuroprotective effects of Dendrobium alkaloids on rat cortical neurons injured by oxygenglucose deprivation and reperfusion. Phytomedicine. 2010; 17(2):108–115. PMID: 19577451.

9. Bao X, Shun Q, Chen L. The Medicinal Plants of Dendrobium (Shi-Hu) in China. A Coloured Atlas. Shanghai: Press of Fudan University and Press of Shanghai Medical University;2001.
10. Li NY, Gao PY, Wang Z. Determination of polysaccharide and amino acid contents in some species of Dendrobium and Flickingeria. J Plant Resour Environ. 2004; 13(4):57–58.
11. Xu C, Chen YL, Zhang M. Structural characterization of the polysaccharide DMP2a-1 from Dendrobium moniliforme. Chinese Pharmaceut J. 2004; 39:900–902.
12. Chen ZH, Chen YL, Wu T, Hua YF, Zhang M. Study on structural characteristics and immunomodulatory activity of polysaccharide DMP4a-1 from Dendrobi-um moniliforme. Chinese Pharmaceut J. 2005; 40:1781–1784.
13. Hsieh YS, Chien C, Liao SK, Liao SF, Hung WT, Yang WB, Lin CC, Cheng TJ, Chang CC, Fang JM, Wong CH. Structure and bioactivity of the polysaccharides in medicinal plant Dendrobium huoshanense. Bioorg Med Chem. 2008; 16(11):6054–6068. PMID: 18467102.

14. Huang MQ, Ruan JY. Monosaccharide composition analysis of 6 water-soluble polysaccharides from Dendrobium species. Zhongguo Zhong Yao Za Zhi. 1997; 22:77–115. PMID: 10743196.
15. Fan Y, He X, Zhou S, Luo A, He T, Chun Z. Composition analysis and antioxidant activity of polysaccharide from Dendrobium denneanum. Int J Biol Macromol. 2009; 45(2):169–173. PMID: 19414030.

16. Wang JH, Luo JP, Zha XQ, Feng BJ. Comparison of antitumor activities of different polysaccharide fractions from the stems of Dendrobium nobile Lindl. Carbohydr Polym. 2010; 79:114–118.
17. Qu WL, Liu HL, Shang ZY. Systematic philological research on the development of Dendrobium in traditional chinese medicine. Asia-Pacific Tradit Med. 2011; 7:133–134.
18. Chen ZR, Lai PF, Lin Q. Effects of different herbal processing methods on levels of water-extractable Dendrobium alkaloids and polysaccharides. J Zhejiang Coll Tradit Chinese Med. 2002; 26:79–81.
19. Korea Food and Drug Administration. Testing Guidelines for Safety Evaluation of Drugs. Cheongju: KFDA;2014.
20. OECD. Guidelines for Testing of Chemicals. Guideline 423. Acute Oral Toxicity-Acute Toxic Class Method. Paris: Organisation for Economic Co-operation and Development;2001.
21. NRC (National Research Council). Guide for the Care and Use of Laboratory Animals. National Academy, Washington, USA: National Research Council;1996.
22. Wang XK, Zhao TF. A discussion of the chemical constituents of Dendrobium plants and of the Chinese herbal drug Shi-Hu. Int J Orient Med. 1990; 15:146–155.
23. Wu SJ, Liu YS, Chen TW, Ng CC, Tzeng WS, Shyu YT. Differentiation of Medicinal Dendrobium Species (Orchidaceae) Using Molecular Markers and Scanning Electron Microscopy. J Food Drug Anal. 2009; 17:474–488.

24. Han ZZ, Xu HD, Kim KH, Ahn TH, Bae JS, Lee JY, Gil KH, Lee JY, Woo SJ, Yoo HJ, Lee HK, Kim KH, Park CK, Zhang HS, Song SW. Reference Data of the Main Physiological Parameters in Control Sprague-Dawley Rats from Pre-clinical Toxicity Studies. Lab Anim Res. 2010; 26(2):153–164.

25. Lee JM, Lee MA, Do HN, Song YI, Bae RJ, Lee HY, Park SH, Kang JS, Kang JK. Historical control data from 13-week repeated toxicity studies in Crj:CD (SD) rats. Lab Anim Res. 2012; 28(2):115–121. PMID: 22787485.

26. Petterino C, Argentino-Storino A. Clinical chemistry and haematology historical data in control Sprague-Dawley rats from pre-clinical toxicity studies. Exp Toxicol Pathol. 2006; 57(3):213–219. PMID: 16343876.

27. Luo JP, Deng YY, Zha XQ. Mechanism of Polysaccharides from Dendrobium huoshanense. on Streptozotocin-Induced Diabetic Cataract. Pharmaceut Biol. 2008; 46:243–249.
28. Lv GY, Xia CQ, Chen SH, Su J, Liu XP, Li B, Gao JL. Effect of Dendrobium officinale granule on long-term-alcohol-induced hypertension rats. Zhongguo Zhong Yao Za Zhi. 2013; 38(20):3560–3565. PMID: 24490573.
29. Jiang MD. Study on a natural health drink: Dendrobium nobile juice. J Zhejiang Agricultural University;1997. p. S1.
30. Fu Y, Mei S, Liu DY, Lai WQ, Chen JG, Wang Y. A toxicological security study of dendrobium candidum capsule. Chinese J Health Lab Technol. 2010; 11:045.
31. Prasad R, Koch B. Antitumor activity of ethanolic extract of Dendrobium formosum in T-cell lymphoma: an in vitro and in vivo study. Biomed Res Int. 2014; 2014:753451. PMID: 24959588.
Figure 1
Daily mean food consumption during 14 days of observation in male (A) and female (B) rats after a single oral treatment of DMAE. Values are presented as the mean±standard deviation of five rats. Significant differences as compared with a control, *P<0.05.
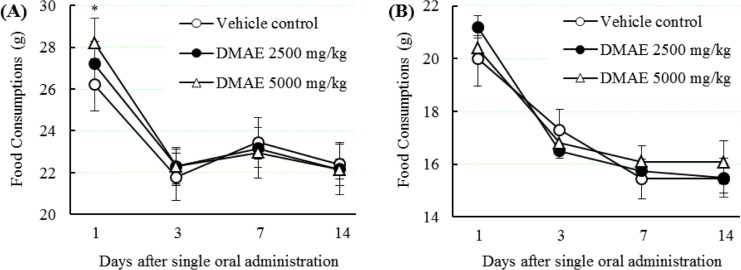
Figure 2
HEK293 cells were incubated with D. moniliforme aqueous extract (DMAE) at concentrations of 1.25, 2.5, 5, 6, 7, 8, 9, and 10 mg/mL for 24 h. Dose dependent toxicity of DMAE in HEK293 cells. Values are presented as the mean±standard deviation of six wells. Significant differences as compared with a control, *P<0.05 and **P<0.01.
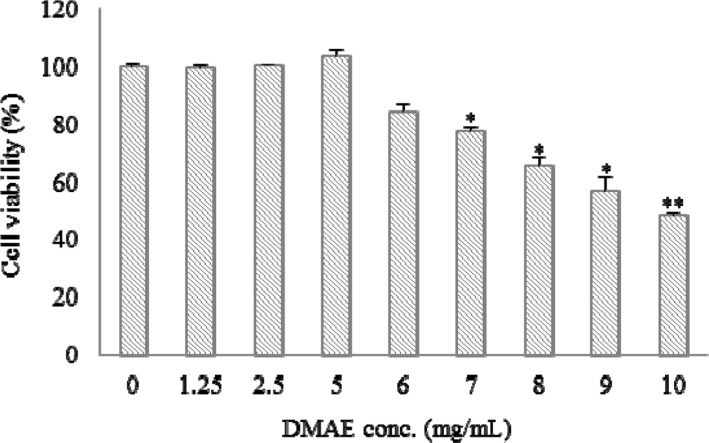
Table 1
Body weight and weight gains of animals exposed with DMAE in the acute toxicity study
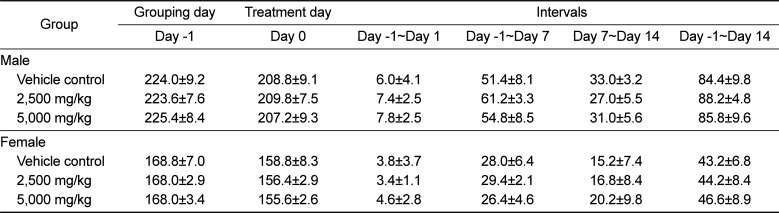
Table 2
Serum biochemical values of animals exposed with DMAE in the acute toxicity study
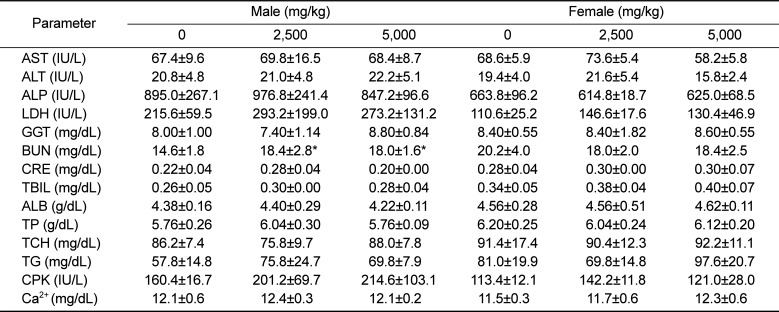
Values are presented as the mean±SD of five rats.
Significant differences were compared with a control, *P<0.05.
AST, aspartate aminotransferase; ALT, alanine aminotransferase; ALP, alkaline phosphatase; LDH, lactate dehydrogenase; GGT, gamma glutamyl transpeptidase; BUN, blood urea nitrogen; CRE, creatinine; TBIL, total bilirubin; ALB, albumin; TP, total protein; TCH, total cholesterol; TG, triglycerides; CPK, creatine phophokinase; and Ca2+, calcium.
Table 3
Absolute organ weights of animals exposed with DMAE in the acute toxicity study
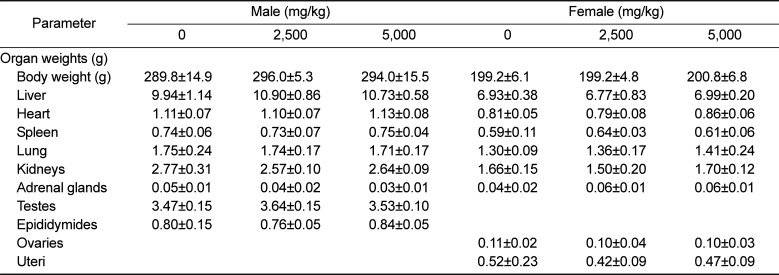
Table 4
Relative organ weights of animals exposed with DMAE in the acute toxicity study




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download