Abstract
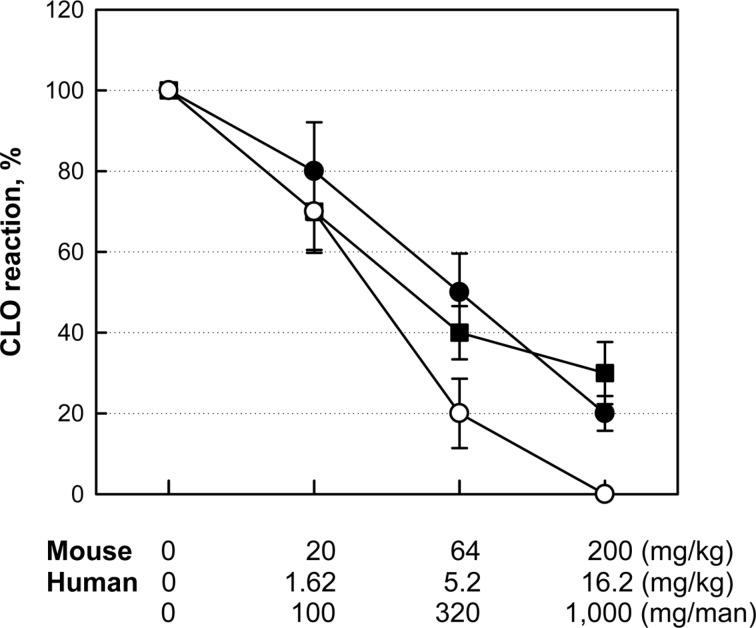
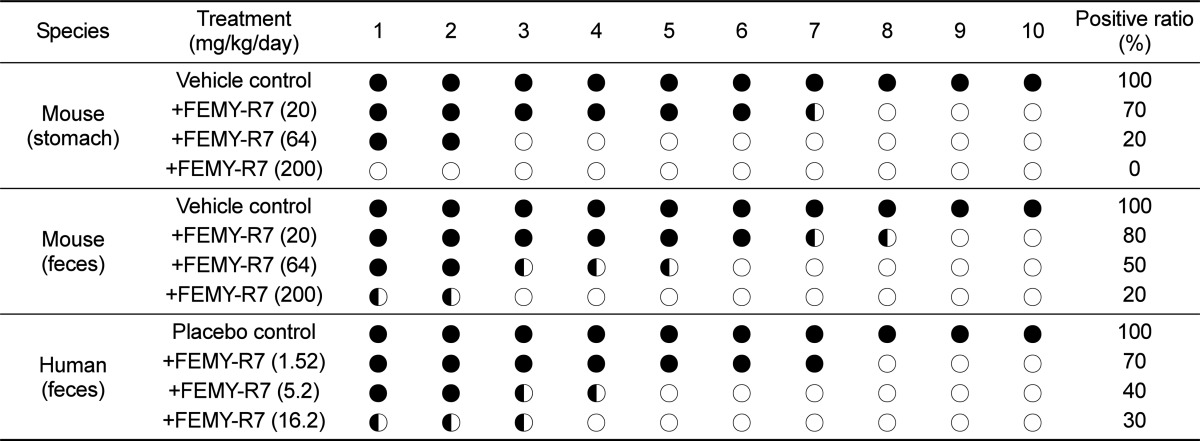
Helicobacter pylori-eliminating effects of FEMY-R7, composed of Laminaria japonica and Oenothera biennis extracts, were investigated in mice and humans. Male C57BL/6 mice were infected with the bacteria by intragastric inoculation (1×109 CFU/mouse) 3 times at 2-day intervals, and simultaneously, orally treated twice a day with total 20, 64 or 200 mg/kg/day FEMY-R7 for 2 weeks. In Campylobcter-like organism (CLO)-detection tests on gastric mucosa and feces, FEMY-R7 reduced the urease-positive reactivity in a dose-dependent manner; i.e., the positivity ratios were decreased to 70, 20, and 10% for gastric mocosa and to 80, 50, and 20% for feces. In a clinical sudy, human subjects, confirmed to be infected with Helicobacter pylori, were orally administered twice a day with capsules containing total 100, 320 or 1,000 mg/man/day FEMY-R7 (matching doses for 20, 64 or 200 mg/kg/day, respectively, in mice from a body surface area-based dose translation) for 8 weeks. FEMY-R7 decreased the positivity ratios in feces to 70, 40, and 30%, respectively. In bacterial culture, H. pylori was identified from the CLO-positive stools of mice and humans. The bacterial identification ratios exhibited a good correlation between the matching doses in mice and humans. It is suggested that FEMY-R7 could be a promising functional food without tolerance as an adjunct to reduce the dosage of antibiotics for the treatment of recurrent H. pylori infection.
Peptic ulcers are one of the common gastric illnesses in modern societies. Gastric erosions and ulcers are caused by various factors including over-secretion and retention of gastric acid, depletion of protective mucin layers, disturbances in focal blood flow, and local inflammation [1,2,3,4]. Ulcer-inducing agents cover nonsteroidal anti-inflammatory drugs [5,6,7,8,9], alcohols [7,8,10], stresses [4,7,8], gastric retention [7,8], gastric hypermotility and acetic acid accumulation [8,11,12,13,14], and Helicobacter pylori infection [1,2,15,16,17].
Since H. pylori infection is related to inflammations, the bacteria are detected in gastric ulcer (70%), gastritis (50-60%), and duodenal ulcer (90%) patients. It has been confirmed that H. pylori is a key factor for chronic active gastritis as well as development to gastric malignancies [18,19,20]. It is well known that H. pylori exacerbates erosions and ulcers by stimulating gastric secretion and retention [21,22]. Accordingly, it is believed that eradication of H. pylori is the most important for effective ulcer treatment in patients exhibiting chronic and repetitive incidence of gastritis [1,2,15,16,17,23].
In order to eliminate H. pylori and treat gastric ulcers, triple therapies composed of proton-pump inhibitors, such as pantoprazole and omeprazole, and antibiotics, such as clarithromycin, metronidazole, and amoxicillin, have been recommended [2]. However, it was recently confirmed that H. pylori exhibits a high tolerance to the antibiotics [24]. Therefore, in spite of relatively-weak potency compared with the antibiotics, natural products without tolerance during repeated treatments may contribute to the eradication of H. pylori from the stomachs.
Extracts of Laminaria japonica and Cladosiphon okamuranus has been widely used in Oriental medicine. Extensive researches demonstrated that the extracts of L. japonica and C. okamuranus contain fucoidan, a sulfate polysaccharide complex, as an active ingredient, that has anti-oxidative, anti-coagulative, and anti-inflammatory activities [25,26]. In addition, the beneficial effects of fucoidan on inflammatory diseases, ischemia, and immune dysfunction are reported [27,28]. Recently, investigators showed that fucoidan interfere with the attachment of H. pylori to gastric cells in animals and in humans [29,30]. On the other hand, tannins from Oenothera biennis seed also have anti-H. pylori activity [31]. Moreover, L. japonica extract (LJE) was confirmed to inhibit bacterial growth in vitro and to block adhesion and colonization of H. pylori in the gastric walls [32]. We also demonstrated that a combinational treatment with LJE and O. biennis seed extract (OBE) killed H. pylori and eliminated the bacteria from the mouse stomachs in vitro and in vivo [33]. Also, effectiveness of the combinational therapy in reducing H. pylori was confirmed by indirect analytical methods; i.e., urea breath test (UBT) and serum pepsinogen I/II levels, in human patients [34].
In the present study, we investigated the comparative H. pylori-eliminating activities of FEMY-R7, a combinational preparation of LJE and OBE in mice and in humans by directly analyzing the presence of bacteria in feces through a Campylobcter-like organism (CLO)-detection test and bacterial identification.
FEMY-R7 containing LJE and OBE (1:1) was obtained from Misuba RTech Co. (Asan, Korea). After washing, drying and grinding, L. japonica was extracted with a hot water extraction method at 60℃ for 24 hours [33,34]. Subsequently, the extract was filtered through a 0.45 µm membrane, and concentrated in a vacuum evaporator. After sterilization, the extract was spray-dried. The O. biennis seeds were extracted with 60% ethanol, filtered, and concentrated. After sterilization, 67% maltodextran was added to the extract and spray-dried.
H. pylori (ATCC49503) was obtained from American Type Culture Collection (Manassas, VA, USA), and cultured on brain heart infusion (BHI) broth in an anaerobic chamber with 10% CO2, 5% O2, and 85% N2 at 37℃ with enough humidity [35].
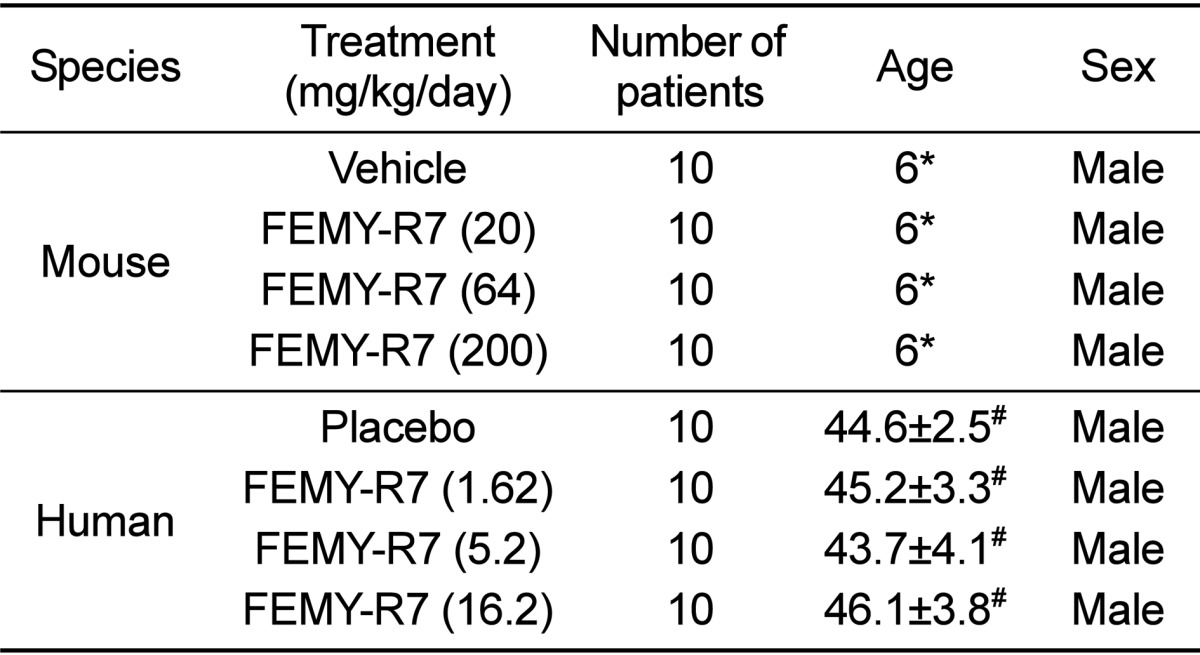
Male C57BL/6 mice (body weights 25-27 g; Table 1) were procured from Daehan Biolink (Eumseong, Korea), and housed in a room with constant environmental conditions (23±2℃; 55±10% relative humidity; 12-hour light-dark cycle; 150-300 lux brightness). Pellet feed and purified water were available ad libitum. All the animal experiments were conducted according to the Standard Operation Procedures (SOP), and approved by the Institutional Animal Care and Use Committee of Chungbuk National University, Korea (Approval No. CBNUR-284-11).
After 12-hour fasting, the mice (n=10/group) were orally inoculated with H. pylori (1×109 CFU/1 mL/mouse) 3 times at 2-day intervals [34], and simultaneously, orally treated twice a day with FEMY-R7 (total 20, 64 or 200 mg/kg/day) for 2 weeks.
Among total of 58 male patients (30-60 years old) who visited the Gastroenterology Department of the Catholic University Medical Center in Daegu, 40 patients were enrolled in the present study (Table 1). Enrollment criteria included infection of H. pylori which was confirmed by CLO test on the feces of patients without experience of H. pylori treatment with antibiotics within 4 weeks [34]. The study protocol was approved by the Institutional Review Board (IRB) of the Catholic University Medical Center in Daegu (Approval No. CR-10-074-RES-01-R), and written informed consent was obtained from all patients.
We designed a randomized, double-blind, placebo-controlled clinical trial for eradication therapy of H. pylori. The patients in treatment group were given twice a day FEMY-R7 capsules containing 1:1 mixture of LJE and OBE (total 1.62, 5.2 or 16.2 mg/kg/day: 100, 320, and 1,000 mg/man/day) before a meal for 8 weeks [34]. The patients in placebo control group were given only the capsules containing 1,000 mg microcrystalline cellulose. During the treatment period, the patients were requested to keep their own dietary lifestyle.
Three hours after the final administration, the mice were sacrificed, and their gastric mucosa (3×3 cm) from the pylorus was biopsied and minced. Additionally, 0.5 g feces of mice (from rectum and colon) and humans (after defecation) were collected, and suspended in the same volume of distilled water and filtered. The gastric mucosal and fecal samples were applied to CLO kits (Kimberly-Clark, Roswell, GA, USA), and incubated at 35℃ for 24 hours to examine urease activity. The reaction (color change) was determined as negative for bright yellow, false (partially) positive for thick yellow, or positive for thick (dark) red [16,17,33,34,35].
Additional feces samples were centrifuged at 500×g for 3 min, and inoculated to a medium containing 20% glycerol for identification of H. pylori as follows [35]:
Oxidase: A colony was collected with a platinumloop, and moved to a filter paper. After dropping p-phenylenediamine dihydrochloride solution, blue change following indolphenol blue production was determined as positive reaction.
Catalase: The colony grown in selective medium was placed on a slide, and bubbling following dropping 3% H2O2 was determined as positive reaction.
Nitrate reduction: Cultured colony was inoculated to nitrate broth, and incubated at 35℃ for 48 hours. Reddish purple change by adding α-naphthylamine and sulfanilic acid was determined as positive reaction.
H2S formation: The central portion of a colony was collected with a platinum-loop, and spread on the slant Triple sugar iron (TSI) medium. Black change following incubation at 37℃ for 24 hours with the lead open was determined as positive reaction producing H2S.
Repeated intragastric inoculation (1×109 CFU/mouse, 3 times) of H. pylori to C57BL/6 mice revealed positive reaction (red color) in CLO test on the gastric mucosa (Table 2). The stomachs of mice orally treated with 20, 64 or 200 mg/kg/day FEMY-R7 for 2 weeks displayed positive reaction in 70% (including partial positivity), 20%, and 0% mice, respectively. By comparison, the CLO positive reactions from feces of the same mice were 80, 50, and 20% with 20, 64 and 200 mg/kg/day FEMY-R7, respectively, although there were several partially-positive mice. On the other hand, treatment of human patients with 1.62, 5.2 or 16.2 mg/kg/day (100, 320 or 1,000 mg/man/day) FEMY-R7 led to 70, 40, and 30% CLO-positive reaction in feces, respectively. Collectively, there was a good dose-response relationship in feces between mice and humans (Figure 1). However, the dose dependency in CLO reaction on mouse gastric mucosa was somewhat different from that of feces.
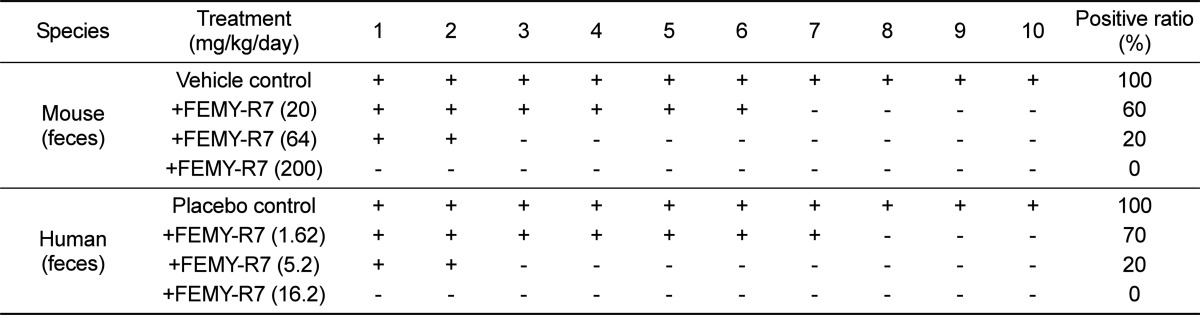
Because of the difference in the CLO test results between stomach and fecal samples of mice, we cultured and identified H. pylori from feces of mice and humans. H. pylori was identified from the stools of all (100%) the mouse and human patients treated with vehicle or placebo preparation (Table 3). However, FEMY-R7 treatment at 20, 64, and 200mg/kg/day decreased the bacterial detection from the mouse feces to 60, 20, and 0%, respectively. Similarly, 1.62, 5.2, and 16.2 mg/kg/day FEMY-R7 in humans reduced the H. pylori-identification ratio to 70, 20, and 0%, respectively.
It is well known that H. pylori secretes urease to survive in acidic environment and to invade gastric mucosa, inducing gastritis, ulcers, and sometimes stimulation of gastric cancers. In a previous investigations [33,34], we demonstrated that FEMY-R7 has an anti-bacterial activity against H. pylori. In CLO test, treatment with FEMY-R7 for 2 weeks eliminated H. pylori from the stomach of mice in a dose-dependent manner, displaying a near-full efficacy at 200 mg/kg/day. In the present study, such a bacteria-eradicating efficacy of FEMY-R7 was confirmed again as analyzed with CLO kits on the mouse gastric mucosa. However, the CLO reaction from mouse feces did not match that of gastric mucosa; i.e., there were several partially-positive reactions in feces of mice that displayed negative reaction in the stomach.
We administered FEMY-R7 to naturally-infected human patients at doses of 1.62, 5.2 or 16.2 mg/kg/day (100, 320 and 1,000 mg/man/day for 60 kg men) to match the doses in mice, according to the body surface area-based dose translation (extrapolation) [36]. Notably, the dose dependency in the CLO reaction from human feces was in parallel with that from mouse feces. More interestingly, the bacterial identification ratios exhibited a good correlation between the matching doses in mice and humans. It was also observed that bacteria was not identified from the feces showing partially-positive reaction in CLO test. Therefore, it is inferred that the partially-positive reaction may be due to the urease enzyme released from dead H. pylori remaining in the stools.
In our recent study, the effectiveness of FEMY-R7 was also confirmed in humans; i.e., daily intake of 300 mg/man/day FEMY-R7 for 8 weeks significantly lowered Delta over baseline-value (BOD) in the expiratory breath in UBT [34]. Although treatment with 300-320 mg/man FEMY-R7 for 8 weeks was not enough to fully eliminate the bacteria in our previous and present studies as analyzed by UBT and feces CLO test, it was confirmed that longer periods (>8 weeks) or higher doses (>320 mg/man) should fulfill the requirement for full clearance of H. pylori from the stomach.
Although triple therapies (for example, omeprazole+clarithromycin+amoxicillin or omeprazole+clarithromycin+metronidazole) consisting of two antibiotics had been recommended as a standard treatment for H. pylori [2], it has been recently demonstrated that the widespread use of antibiotics led to a rapidly-increasing bacterial resistance [24,37]. Thus, there is a strong rationale for the development of novel anti-bacterial agents without resistance and adverse-effects. In the present study, we showed the efficacy of FEMY-R7 in eliminating H. pylori from mice and humans by analyzing the correlations between gastric mucosal and fecal samples from mice as well as between fecal samples from mice and humans. In conclusion, it is suggested that FEMY-R7, a combinational regimen composed of LJE and OBE, could be a promising candidate overcoming tolerance of antibiotics or an adjunct to reduce the dosage of antibiotics for the treatment of recurrent H. pylori infection.
Acknowledgments
This research was supported by High Value-added Food Technology Development Program, Ministry of Agriculture, Food and Rural Affairs (MAFRA; grant number 113034-3).
References
1. Wallace JL, Granger DN. The cellular and molecular basis of gastric mucosal defense. FASEB J. 1996; 10(7):731–740. PMID: 8635690.

2. Neal MJ. Medical Pharmacology at a Glance. 3rd ed. London: Blackwell Publishing Inc;2003. p. 30–31.
3. Isobe H, Okajima K, Harada N, Liu W, Okabe H. Activated protein C reduces stress-induced gastric mucosal injury in rats by inhibiting the endothelial cell injury. J Thromb Haemost. 2004; 2(2):313–320. PMID: 14995995.

4. Byun SK, Lee YE, Shin SH, Jang JY, Choi BI, Park DS, Jeon JH, Nahm SS, Hwang SY, Kim YB. The role of corticosteroids in stress-induced gastric ulceration in rats. Lab Anim Res. 2007; 23(2):127–131.
5. Slomiany BL, Piotrowski J, Slomiany A. Induction of tumor necrosis factor-alpha and apoptosis in gastric mucosal injury by indomethacin: effect of omeprazole and ebrotidine. Scand J Gastroenterol. 1997; 32(7):638–642. PMID: 9246701.
6. Filaretova L, Tanaka A, Miyazawa T, Kato S, Takeuchi K. Mechanisms by which endogenous glucocorticoid protects against indomethacin-induced gastric injury in rats. Am J Physiol Gastrointest Liver Physiol. 2002; 283(5):1082–1089.
7. Cao H, Wang MW, Jia JH, Wang QG, Cheng MS. Comparison of the effects of pantoprazole enantimers on gastric mucosal lesions and gastric epithelial cells in rats. J Health Sci. 2004; 50(1):1–8.
8. Rao ChV, Ojha SK, Radhakrishnan K, Govindarajan R, Rastogi S, Mehrotra S, Pushpangadan P. Antiulcer activity of Utleria salicifolia rhizome extract. J Ethnopharmacol. 2004; 91(2-3):243–249. PMID: 15120446.

9. Kim YR, Lee MR, Kim YH, Jang BJ, Park SC, Han SH, Kim BH, Ryoo ZY, Kim KS. Effect of Opuntiahumifusa extract on indomethacin-induced gastric ulcer in Sprague Dawley rat. Lab Anim Res. 2005; 21(4):375–578.
10. Raffin RP, Colomé LM, Schapoval EE, Jornada DS, Pohlmann AR, Guterres SS. Gastro-resistant microparticles containing sodium pantoprazole: stability and in vivo anti-ulcer activity. Open Drug Deliv J. 2007; 1:28–35.
11. Dias PC, Foglio MA, Possenti A, de Carvalho JE. Antiulcerogenic activity of crude hydroalcoholic extract of Rosmarinus officinalis L. J Ethnopharmacol. 2000; 69(1):57–62. PMID: 10661884.
12. Cantarella G, Martinez G, Cutuli VM, Loreto C, D'Alcamo M, Prato A, Amico-Roxas M, Bernardini R, Clementi G. Adrenomedullin modulates COX-2 and HGF expression in reserpine-injuried gastric mucosa in the rat. Eur J Pharmacol. 2005; 518(2-3):221–226. PMID: 16081063.

13. Cantarella G, Martinez G, Di Benedetto G, Loreto C, Musumeci G, Prato A, Lempereur L, Matera M, Amico-Roxas M, Bernardini R, Clementi G. Protective effects of amylin on reserpine-induced gastric damage in the rat. Pharmacol Res. 2007; 56(1):27–34. PMID: 17412609.

14. Işbil Büyükcoşkun N, Güleç G, Ozlük K. Protective effect of centrally-injected glucagon-like peptide-1 on reserpine-induced gastric mucosal lesions in rat: possible mechanisms. Turk J Gastroenterol. 2006; 17(1):1–6. PMID: 16830270.
15. Pope AJ, Toseland CD, Rushant B, Richardson S, McVey M, Hills J. Effect of potent urease inhibitor, fluorofamide, on Helicobacter sp. in vivo and in vitro. Dig Dis Sci. 1998; 43(1):109–119. PMID: 9508511.
16. Hahm KB, Kim DH, Lee KM, Lee JS, Surh YJ, Kim YB, Yoo BM, Kim JH, Joo HJ, Cho YK, Nam KT, Cho SW. Effect of longterm administration of rebamipide on Helicobacter pylori infection in mice. Aliment Pharmacol Ther. 2003; 18(Suppl 1):24–38. PMID: 12925138.

17. Aristoteli LP, O'Rourke JL, Danon S, Larsson H, Mellgard B, Mitchell H, Lee A. Urea, fluorofamide, and omeprazole treatments alter helicobacter colonization in the mouse gastric mucosa. Helicobacter. 2006; 11(5):460–468. PMID: 16961809.

18. Coghlan JG, Gilligan D, Humphries H, McKenna D, Dooley C, Sweeney E, Keane C, O'Morain C. Campylobacter pylori and recurrence of duodenal ulcers--a 12-month follow-up study. Lancet. 1987; 2(8568):1109–1111. PMID: 2890019.
19. Graham DY, Evans DG, Evans DJ Jr. Campylobacter pylori. The organism and its clinical relevance. J Clin Gastroenterol. 1989; 11(Suppl 1):S43–S48. PMID: 2809138.
20. Wotherspoon AC, Ortiz-Hidalgo C, Falzon MR, Isaacson PG. Helicobacter pylori-associated gastritis and primary B-cell gastric lymphoma. Lancet. 1991; 338(8776):1175–1176. PMID: 1682595.
21. Cover TL, Blaser MJ. Helicobacter pylori and gastroduodenal disease. Annu Rev Med. 1992; 43:135–145. PMID: 1580578.

22. Lee A, Fox J, Hazell S. Pathogenicity of Helicobacter pylori: a perspective. Infect Immun. 1993; 61(5):1601–1610. PMID: 8478048.

23. Marshall BJ. Helicobacter pylori in peptic ulcer: have Koch's postulates been fulfilled? Ann Med. 1995; 27(5):565–568. PMID: 8541033.
24. Zhang Z, Liu ZQ, Zheng PY, Tang FA, Yang PC. Influence of efflux pump inhibitors on the multidrug resistance of Helicobacter pylori. World J Gastroenterol. 2010; 16(10):1279–1284. PMID: 20222174.
25. Feldman SC, Reynaldi S, Stortz CA, Cerezo AS, Damont EB. Antiviral properties of fucoidan fractions from Leathesia difformis. Phytomedicine. 1999; 6(5):335–340. PMID: 11962540.

26. Wang J, Zhang Q, Zhang Z, Song H, Li P. Potential antioxidant and anticoagulant capacity of low molecular weight fucoidan fractions extracted from Laminaria japonica. Int J Biol Macromol. 2010; 46(1):6–12. PMID: 19883681.

27. Bojakowski K, Abramczyk P, Bojakowska M, Zwoliñska A, Przybylski J, Gaciong Z. Fucoidan improves the renal blood flow in the early stage of renal ischemia/reperfusion injury in the rat. J Physiol Pharmacol. 2001; 52(1):137–143. PMID: 11321507.
28. Li N, Zhang Q, Song J. Toxicological evaluation of fucoidan extracted from Laminaria japonica in Wistar rats. Food Chem Toxicol. 2005; 43(3):421–426. PMID: 15680677.

29. Shibata H, Iimuro M, Uchiya N, Kawamori T, Nagaoka M, Ueyama S, Hashimoto S, Yokokura T, Sugimura T, Wakabayashi K. Preventive effects of Cladosiphon fucoidan against Helicobacter pylori infection in Mongolian gerbils. Helicobacter. 2003; 8(1):59–65. PMID: 12603617.

30. Shibata H, KimuraTakagi I, Nagaoka M, Hashimoto S, Sawada H, Ueyama S, Yokokura T. Inhibitory effect of Cladosiphon fucoidan on the adhesion of Helicobacter pylori to human gastric cells. J Nutr Sci Vitaminol. 1999; 45(3):325–336. PMID: 10524351.
31. Funatogawa K, Hayashi S, Shimomura H, Yoshida T, Hatano T, Ito H, Hirai Y. Antibacterial activity of hydrolyzable tannins derived from medicinal plants against Helicobacter pylori. Microbiol Immunol. 2004; 48(4):251–261. PMID: 15107535.
32. Kamiya S, Osaki T, Yamaguci H, Shimada T, Okada T, Takahashi Y. Effect of evening primrose extract on growth, adhesion and colonization of Helicobacter pylori. Bact Adherence Bofilm. 2003; 17:16–19.
33. Cai J, Kim TS, Jang JY, Kim J, Shin K, Lee SP, Choi EK, Kim SH, Park M, Kim JB, Kim YB. In vitro and in vivo anti-Helicobacter pylori activities of FEMY-R7 composed of fucoidan and evening primrose extract. Lab Anim Res. 2014; 30(1):28–34. PMID: 24707302.
34. Kim TS, Choi EK, Kim J, Shin K, Lee SP, Choi Y, Jeon JH, Kim YB. Anti-Helicobacter pylori activities of FEMY-R7 composed of fucoidan and evening primrose extract in mice and humans. Lab Anim Res. 2014; 30(3):131–135. PMID: 25324874.
35. Yang YH, Park D, Yang G, Lee SH, Bae DK, Kyung J, Kim D, Choi EK, Son JC, Hwang SY, Kim YB. Anti-Helicobacter pylori effects of IgY from egg york of immunized hens. Lab Anim Res. 2012; 28(1):55–60. PMID: 22474475.
36. Reagan-Shaw S, Nihal M, Ahmad N. Dose translation from animal to human studies revisited. FASEB J. 2008; 22(3):659–661. PMID: 17942826.
37. Daw MA, Deegan P, Leen E, O'Moráin C. Short report: the effect of omeprazole on Helicobacter pylori and associated gastritis. Aliment Pharmacol Ther. 1991; 5(4):435–439. PMID: 1777552.

Figure 1
Dose-dependent H. pylori-eliminating activity of FEMY-R7 in mouse and human patients. H. pylori was detected with CLO kits from mouse stomach (◌), mouse feces (•) or human feces (▪).




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download