Abstract
Purpose
This study aimed to evaluate the safety and efficacy to induce clinical desensitization to cow's milk (CM) of an oral immunotherapy (OIT) protocol in a pediatric population with cow's milk allergy (CMA). In addition, the immune responses against β-casein, of peripheral blood mononuclear cells (PBMCs) from CMA patients, before and after the protocol were evaluated and compared to a nonallergic population.
Methods
A group of 20 children with IgE-mediated CMA and 15 nonallergic children were recruited. Allergic subjects underwent an OIT protocol based on weekly doses of commercial semi-skimmed ultra-high temperature treated (UHT) CM, followed by a maintenance phase. Immune profiles and changes in all subjects were investigated by measuring Th1, Th2, and Treg cytokines, transcription factors, and specific IgE and IgG4 levels.
Results
The CM-OIT protocol enabled to desensitize 70% of the allergic patients. Successful OIT was accompanied by significant increases in casein-specific IgG4 levels, together with a reduction in the concentration of antigen-specific IgE and in IL-5, IL-13, and IL-10 production by β-casein-stimulated PBMCs. Baseline significant differences observed between allergic and nonallergic children in IL-13 and IL-5 levels were no longer found once the protocol had finished.
Cow's milk allergy (CMA) is the most common food allergy among infants in Europe, with prevalence rates estimated in the range of 2% and 3%.1 Although previous reports stated a good prognosis with a high rate of spontaneous resolution,23 recent studies suggest varying results (13%-37%) to the rate of resolution during childhood.14
The accepted management of CMA is the total avoidance of milk to prevent adverse reactions, which can be life-threatening.56 Nevertheless, milk exclusion involves a wide dietary restriction, which leads to negative nutritional, social, psychological, and economic consequences.7 Moreover, because of cow's milk (CM) ubiquity, avoidance cannot be always guaranteed, and accidental reactions may occur.8 For this reason, CM oral immunotherapy (OIT) appears as a promising approach for CMA treatment.9 As in any other food OIT protocol, CM-OIT starts with administration of milk at very low doses, which are increased up to the usual intake (around 200 mL). Thereafter, it is given daily in a maintenance dosage.10 The main goal of CM-OIT is to increase the threshold dose which triggers symptoms, protecting patients against reactions on accidental exposure. In addition, it allows the inclusion of milk in the patient's diet, with the subsequent benefit in nutrition and quality of life.
Previous studies on CM-OIT have shown desensitization rates of 36%-92% after a wide array of protocols.11 However, there is still a lack of sufficient evidence regarding long-term efficacy, safety, impact on quality of life, and cost-effectiveness of these procedures. Thus, CM-OIT is considered nowadays an experimental treatment not ready yet for clinical practice.1213
Currently, there is little knowledge regarding immunological changes and mechanisms subjacent to CM-OIT. So far, the different studies performed have highlighted an increase in the levels of allergen-specific IgG4 after successful CM-desensitization.14151617 Nevertheless, in cases of the allergen-specific IgE response, the results are somehow controversial.17181920 Although these observations clearly indicate immune-deviation, to the best of our knowledge, there is only 1 report available characterizing the T-cell response of milk allergic patients before and after a CM-OIT protocol.21
The objective of this study was to evaluate the safety and efficacy to induce clinical desensitization to CM of an OIT protocol in a pediatric population with CMA. In addition, with the aim of adding some insights into the immunological mechanisms subjacent to CM-OIT, the immune responses against β-casein, one of the main milk allergens, of Peripheral Blood Mononuclear Cells (PBMCs) from CMA patients before and after the protocol were evaluated. For that purpose, a panel of cytokines covering Th1, Th2, and Treg responses, together with allergen-specific IgE and IgG4 levels were assessed. For comparison, a population of nonallergic donors from the same age-range was included in the study.
All human samples/procedures were obtained/performed with written consent from the next of kin, caretakers, or guardians on behalf of the minors/children involved in the study. The Bioethics Committees from Consejo Superior de Investigaciones Científicas and Hospital Universitario La Paz (Madrid, Spain) approved all experiments.
Subjects were recruited from the Allergology Service at Infanta Sofia Hospital (Madrid, Spain). All the children enrolled in the CMA group were patients diagnosed through a compatible clinical history, positive skin prick test (≥3 mm of negative control) and positive CM-, casein- (CN), α-lactalbumin (α-La)-, and/or β-lactoglobulin (β-Lg)-specific IgE. In addition, all the subjects had experienced a positive reaction during a single blind food challenge (SBFC) with commercial semi-skimmed ultra-high temperature-treated (UHT) pasteurized CM (3.3% protein) the month before the beginning of the study. A group of nonallergic children, with no detectable IgE against a broad panel of the most common allergens, was also included in the study.
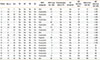
The protocol was carried out at the Allergology Day Unit of the Infanta Sofía Hospital, under the direct supervision of the medical and nursing staff, and with all the equipment and material required for the treatment of possible allergic reactions that could occur during the procedure. The CM-OIT protocol was performed with commercial semi-skimmed UHT CM, as described in Table 1. The starting dose of the protocol was the previous one to the highest tolerated dose during the SBFC. Once the patients were able to tolerate 4 mL of undiluted CM without symptoms, an open challenge with baked goods containing milk was performed. Similarly, after tolerating 10 mL, patients were challenged with milk-containing cold meat, with milk chocolate after 15 mL, liquid fermented milk (Actimel®) after 60 mL, yogurt after 100 mL, cow's cream cheese after 120 mL, and finally with goat and ewe's milk cheeses after 200-240 mL. Between visits, patients were advised to daily ingest at home the maximum dose tolerated during their last visit to the unit. When needed, premedication with oral antihistamines was given to patients who developed adverse reactions during the protocol, in order to control the symptoms. Reaction severity was assessed according to Clark and Ewan.22 In cases of moderate reactions, these were pharmacologically treated and the protocol was restarted in the following week at the previously tolerated dose. Hence, the length of the protocol was increased stepwise depending on the severity of the reactions experienced by each patient. In cases of repeated severe reactions (anaphylaxis), the desensitization protocol was interrupted. Patients were considered to have successfully completed the protocol if they were able to tolerate a minimum of 200 mL of CM in less than 24 months.
Once the patients completed the OIT protocol, they maintained, during 1 year, a daily ingestion of 200 mL of commercial semi-skimmed UHT CM. If after 1 year the clinical desensitization was sustained, the patients were authorized to have a non-restricted diet.
Blood samples were withdrawn from the control subjects included in the study and from the allergic patients before and after the OIT protocol was finished, and sera were analyzed for specific-IgE to CM, CN, α-La, and β-Lg, and CN-specific IgG4 using the Phadia ImmunoCAP-System FEIA (Thermo Fisher Scientific, Barcelona, Spain).
PBMCs were isolated by density-gradient separation (Ficoll-Paque PLUS; GE Healthcare, Barcelona, Spain) from heparinized venous blood. PBMCs (2×106 cells/mL) were cultured in vitro for 7 days at 37℃ in 5% CO2 with medium alone (AIM-V, Biowest, Nuaillé, France), as negative control, or 200 µg/mL of β-casein (Sigma, St. Louis, MO, USA), with a lipopolysaccharide (LPS) level <0.4 ng/mg, as quantified by the Pierce LAL Chromogenic Endotoxin Quantitation Kit (Thermo Scientific, Waltham, MA, USA). Phytohemagglutinin (PHA) (4 µg/mL; Sigma) was used as positive control.
After 7 days of culture, levels of IL-5, IL-13, IL-10, IFN-γ, and TNF-α in supernatants were analyzed by a multiplex bead assay (BD cytometric bead array; BD Biosciences, San Diego, CA, USA), according to the manufacturer's instructions. Cytokine secretion was correlated to the standard of each of the human cytokines (0-2,500 pg/mL). The Gallios™ flow cytometer (Beckman Coulter, Barcelona, Spain) was used to acquire data, which were analyzed by Beckman Coulter Kaluza and FCAP Array v3 (BD Biosciences) Software. Results are expressed as the amount of each cytokine detected after the stimulation with β-casein minus the amount detected after stimulation with the negative control.
Total RNA from the PBMCs cultured for 7 days was extracted using the Total RNA Isolation NucleoSpin® RNA II Kit according to the manufacturer's instructions (Macherey-Nagel, Duren, Germany). The RNA template was qualitatively assessed and quantified using an Agilent 2100 Bioanalyzer (Agilent Technologies, Palo Alto, CA, USA) and a NanoDrop ND1000 instrument (Thermo Fisher Scientific), respectively. Reverse transcription reactions were performed following the manufacturer's instructions with the Transcriptor First Strand cDNA Synthesis Kit (Roche, Manheim, Germany). RT-qPCR was performed in a ViiA™ 7 Real-Time PCR System (Applied Biosytems, Foster City, CA, USA) using a total of 6 ng of transcribed cDNA and TaqMan® Gene Expression Assay for the transcription factors: GATA3 (Human Assay ID Hs00231122m1), T-bet (ID Hs 00203436m1), and FoxP3 (ID Hs01085834m1), according to the manufacturer's recommendations. The hypoxanthine guanine phosphoribosyl transferase (HPRT) ID Hs02800695m1 was used as a reference gene. The amplification program used was: 1 cycle of 10 minutes at 95℃, 40 cycles of 15 seconds at 95℃, and finally 1 cycle of 1 minutes at 60℃. All reactions were performed in triplicate. The mean value of the replicates for each sample was expressed as the quantification cycle (Ct). The relative gene expression values (RQ) were calculated using the delta delta CT method. RQ of more than 2 or less than 0.5 was established to be considered relevant.
Statistical analyses were performed using the GraphPad Prism 5 software (San Diego, CA, USA). The nonparametric Mann-Whitney test was used to compare between the groups, and the Wilcoxon t test was used to analyze differences between variables during OIT protocol. Results are presented as mean±standard error of the mean (SEM) unless indicated. Differences were considered significant at the 95% confidence level.
Twenty allergic children (7 females and 13 males) aged between 1.5 and 11 years (mean 4.3 years) and 15 nonallergic children (8 females and 7 males) aged between 5 and 14 years (mean 8.7 years) were enrolled in the study (Table 2). There were not statistically significant differences regarding sex or age between any of the groups. Fifty-five percent of the CMA patients were allergic to other foods. Also, 45% of them had a past or current history of atopic dermatitis, 40% of asthma, and 30% of allergic rhinitis (Table 2). The baseline average specific IgE levels of the allergic group were 27.38 kU/L [0.4-100 kU/L] for CM, 26.45 kU/L [0.1-100 kU/L] for CN, 20.53 kU/L [0.1-94.1 kU/L] for α-La, and 14.18 kU/L [0.5-82.3 kU/L] for β-Lg.
During the SBFC, the median threshold dose resulting in an allergic reaction was 4.0 mL (0.1-120 mL), with 60% of the patients developing anaphylaxis and 30% skin-related reactions (Table 2).
Among the 20 patients included in the study, 14 (patients 1 to 14 in Table 2) tolerated more than 200 mL of CM, as well as goat's and ewe's milk cheeses, in an average period of 18.9 months (interval: 6-24 months), with 27.8 visits to the clinic of (interval 10-46 times). Fifty-seven percent of them experienced mild dermatologic reactions during the desensitization protocol, with the most common symptoms being mouth itching and perioral erythema. Immunological changes associated with the OIT protocol were only assessed in these patients.
Four patients (patients 15 to 18 in Table 2) tolerated between 35 and 80 mL of CM after 24 months of treatment and 40 visits (interval 32-48 times) to the clinic, on average. At the end of the 24 months period, established as a time limit, this group was able to consume bakery, cold meat, and milk chocolate without developing adverse reactions. The reactions during desensitization of this particular group of patients were more severe, reporting strong abdominal pain and anaphylactic reactions. Two patients (patients 19 and 20) discontinued the study due to parental decision.
As depicted in Fig. 1A, in patients that successfully completed the CM-OIT protocol (n=14) a significant (at least 4-fold), drop in their CM, α-La, β-Lg, and CN-specific IgE levels was detected once the protocol was finished. Moreover, a significant increase from baseline was reached in the serum casein-specific IgG4 concentration after the CM-OIT treatment (Fig. 1B).
Regarding the cellular response, a marked decrease in IL-13, IL-5 and IL-10 (statistically significant for IL-13 and IL-10) production by PBMCs upon β-CN stimulation was observed when comparing initial and post-OIT levels (Fig. 2). Th1 cytokines, IFN-γ, and TNF-α were not detected. Interestingly, the baseline significant differences observed between allergic and nonallergic children in IL-13 and IL-5 levels were no longer found once the protocol had finished (Fig. 2A and B). IL-10 production by β-CN-primed PBMCs from nonallergic donors was significantly higher (P<0.01) than that from CMA patients at the end of the protocol (Fig. 2C).
Analysis of the expression levels of the transcription factors Foxp3, GATA3, and T-bet in the successful patients (n=14), before and after the CM-OIT protocol, did not show any changes, with RQ values of 1.25 for FoxP3, 1.48 for GATA3, and 1.92 for T-bet.
In the present study, CM-desensitization (corresponding to tolerance to at least 200 mL of CM) was achieved by 70% of the children with IgE-mediated CM allergy initially included in the CM-OIT protocol. The desensitization rate was in the range of previous reports by González-Jiménez et al.,23 Vázquez-Ortiz et al.24, and Meglio et al.,25 where 72%, 71.6%, and 71.4%, respectively, of the children enrolled were desensitized to CM. A distinct feature of the reported protocol is the progressive introduction of milk-containing foods into patients, diet: this allowed food diversification and helped improve their quality of life while reducing the withdrawals from the therapy as they felt confident with the results of the intervention. It should be mentioned that children seemed to be not only desensitized to CM, but also to goat's and ewe's milk proteins. Several case reports on allergy to goat and sheep milk proteins in individuals previously desensitized to CM can be found in the literature.2627 In fact, Rodríguez del Río et al.28 found, in patients who tolerated CM after CM-OIT, that 26% of them were still allergic to goat's milk and ewe's milk, with 47% of the positive oral food challenges graded as anaphylactic reactions.
Adverse reactions were usually controllable with a rate of occurrences lower than those reported in other CM-OIT protocols.293031 In any case, the side effects encountered during the treatment considerably lengthened the duration of the protocol, compared to what was originally planned, highlighting the importance of adapting the dosing regimen to the patient's response to the therapy. Similar results have recently been observed in the course of an egg-OIT protocol, which had to be increased in approximately 9 months in relation to the original desensitization schedule.32 It is worthwhile to mention that some studies have documented that prolonged OIT treatments enhance the desensitization effect, suggesting that longer treatment courses are more effective and possibly safer.313334
Due to the length of the protocol and the strong familiar commitment required for CM-OIT, the study was open-label and uncontrolled. However, the high baseline specific-IgE levels, as well as the adverse reactions observed during the therapy, suggested that spontaneous CMA resolution was very unlikely in the population under study.353637 The absence of a placebo group is justified by the results obtained in the placebo-controlled trials performed by Skripak et al.17 and Longo et al.,18 in which none of the children included in the placebo group achieved even partial tolerance once the study had ended. In cases where the treatment applied had altered the natural course of CM-oral tolerance achievement, the authors would have either anticipated it or increased the threshold dose for patients that did not successfully complete the therapy.3138 While the current protocol setting cannot confirm whether patients were tolerant as CM was not withdrawn for ethical reasons, it should be noted that all the patients considered successfully desensitized were on a free diet 1 year after the OIT protocol had ended.
Baseline specific-IgG4 levels increased after the therapy, as previously observed by a number of authors in other CM-OIT protocols,11141517 as well as in patients who spontaneously recovered from CMA,1639 confirming the important role of this immunoglobulin in oral tolerance establishment. Concomitant with the increase in specific-IgG4, significantly reduced antigen-specific-IgE production was found. Although a decrease in allergen-specific IgE production is commonly reported in most of the CM-OIT protocols described,1924303840 other studies have reported no changes,172025 which according to the authors, might be explained due to the shorter duration of their treatments.
In accordance with previous publications,4142 β-CN-primed PBMCs from CM allergic patients presented a significant Th2-biased phenotype when compared to nonallergic individuals. In fact, enumeration of CN-specific IL-4- and IL-13-secreting T cells has been proposed as a promising tool to improve diagnosis of CMA.43 β-CN (27% of the total milk proteins) was chosen for PBMC stimulation as it represents a serious health risk in patients with CMA, since 75% of sera from patients with IgE-mediated CMA against whole bovine CN have IgE directed against it.44 Furthermore, it is known that PBMCs from clinically reactive IgE-mediated CMA patients proliferate in response to LPS-free αS-, β-, and κ-CN, but not β-Lg.45 Importantly, significant differences in baseline IL-5 and IL-13 levels between CMA and nonallergic children were no longer found once the treatment had finished, demonstrating a transition toward a nonallergic phenotype in the patients able to ingest ≥200 mL of milk without developing symptoms. To the best of our knowledge, there is only 1 other publication dealing with changes in the cytokine response in milk allergic individuals subjected to CM-OIT. Bedoret et al.21 found a shift from IL-4 and IL13 to IFN-production in patients desensitized to milk. However, in our protocol, detectable levels of β-casein-specific IFN- were not found.
In contrast to other OIT protocols toward egg3246 or peanut,47 IL-10 production by β-CN-stimulated PBMCs decreased, suggesting not only Th2- and Treg cell impairment, as IL-10 production is considered one of the main effectors responsible for the suppressive effect of Treg.48 Interestingly, Bedoret et al.21 ruled out a role of allergen-specific FoxP3+ regulatory T cells in oral desensitization to CMA, suggesting that even when high doses of antigen are administered, the mechanism lies in anergy or deletion, rather than suppression, of allergen-specific T cells. However, according to Shreffler et al.,49 allergen-specific and functionally suppressive Treg cells play a role in the resolution of milk allergy and could be important targets for immune monitoring. The authors reported that introduction of milk into the diet causes a decline in the frequency of Treg present in the peripheral blood, in parallel with an increase in the IgG4/IgE ratio and a reduced basophile response, which is attributed to Treg cells being recruited to the gastrointestinal tract by allergen ingestion.49 Similarly, Varsheny et al.50 claimed that decreased Th2-cytokine and increased IgG4/Treg cell productions are the main immunologic changes that accompany the clinical efficacy of peanut OIT, even if they do not detect significant changes in blood IL-10, which raises the hypothesis that blood cytokine levels do not reflect mucosal production of Treg or that mucosal and periphery Treg exert different functions. A further possibility is that induction of Treg is transient. Thus, Jones et al.47 found, in the course of peanut OIT, early generation of Treg and associated increased production of IL-10 by PBMCs eventually decreased after 12 months. In this respect, it should be noted that in our study, a long period of time required for a successful outcome of the treatment (average 18.9 months) might have masked certain immunological events. On the other hand, in accordance with our results, Tiemessen et al.42 reported that CM-specific IL-10 production was significantly higher in T-cell clones derived from children with persistent CMA than from nonallergic children.
The lack of treatment-related changes in the expression of Treg (Foxp3), Th1 (Tbet), or Th2 (GATA3) transcription factors, despite the existence of measurable variations in cytokine production, was already reported by Jones et al.47 and Perezábad et al.32 in their studies with peanut and egg OIT, respectively.
In conclusion, this report presents an efficient and safe milk-OIT protocol characterized by the progressive introduction of milk-containing foods that may substantially improve the patient's quality of life along the treatment course. Successful OIT was accompanied by an immune alteration characterized by a significant increase in antigen-specific IgG4 levels, a significant reduction in antigen-specific IgE concentration, and IL-5, and decreased IL-13 production by β-CN-stimulated PBMCs toward a nonallergic phenotype. More research needs to be done in order to understand the role of IL-10 in CM-OIT.
Figures and Tables
Fig. 1
Antibody response in CM-allergic patients. Serum-specific (A) IgE (kU/L) and (B) IgG4 (µg/L) to CM, α-La, β-Lg, and CN before (Orange blocks) and after (Blue blocks) the OIT protocol in the CM-allergic patients who tolerated at least 200 mL of cow's milk (n=14). Bars represent mean±SEM. ***P<0.001; **P<0.01.

Fig. 2
Cytokine production by β-CN-stimulated PBMCs. Levels of (A) IL-13, (B) IL-5, and (C) IL-10 (pg/mL) before (Orange blocks) and after (Blue blocks) the OIT protocol in the CM-allergic patients who tolerated at least 200 mL of CM (n=14). Gray blocks represent baseline cytokine production by β-CN-stimulated PBMCs in nonallergic children (n=15). Bars represent mean±SEM. *P<0.05; **P<0.01; ***P<0.001.

Table 1
Cow's milk oral immunotherapy protocol (CM-OIT)

Table 2
Demographics, anamnesis, and response to cow's milk-OIT in cow's milk-allergic patients
ACKNOWLEDGMENTS
All the authors declare that they have no competing financial interests. Authors would like to acknowledge Dr. Pedro J. Martín-Alvárez for his fruitful discussions with statistical analysis. Ms. Perezábad, Dr. López-Fandiño and Dr. Molina are members of the COST action ImpARAS FA1402. Ms. Perezábad is in receipt of a Formación de Personal Universitario Ph.D. Grant from the Ministerio de Educación, Cultura y Deporte (Spain).
References
1. Skripak JM, Matsui EC, Mudd K, Wood RA. The natural history of IgE-mediated cow's milk allergy. J Allergy Clin Immunol. 2007; 120:1172–1177.
2. Vanto T, Helppilä S, Juntunen-Backman K, Kalimo K, Klemola T, Korpela R, et al. Prediction of the development of tolerance to milk in children with cow's milk hypersensitivity. J Pediatr. 2004; 144:218–222.
3. Høst A, Halken S, Jacobsen HP, Christensen AE, Herskind AM, Plesner K. Clinical course of cow's milk protein allergy/intolerance and atopic diseases in childhood. Pediatr Allergy Immunol. 2002; 13:Suppl 15. 23–28.
4. Santos A, Dias A, Pinheiro JA. Predictive factors for the persistence of cow's milk allergy. Pediatr Allergy Immunol. 2010; 21:1127–1134.
5. Bock SA, Muñoz-Furlong A, Sampson HA. Fatalities due to anaphylactic reactions to foods. J Allergy Clin Immunol. 2001; 107:191–193.
6. Bock SA, Muñoz-Furlong A, Sampson HA. Further fatalities caused by anaphylactic reactions to food, 2001-2006. J Allergy Clin Immunol. 2007; 119:1016–1018.
7. Lieberman JA, Sicherer SH. Quality of life in food allergy. Curr Opin Allergy Clin Immunol. 2011; 11:236–242.
8. Wood RA. Food-specific immunotherapy: past, present, and future. J Allergy Clin Immunol. 2008; 121:336–337.
9. Martorell Calatayud C, Muriel García A, Martorell Aragonés A, De La Hoz Caballer B. Safety and efficacy profile and immunological changes associated with oral immunotherapy for IgE-mediated cow's milk allergy in children: systematic review and meta-analysis. J Investig Allergol Clin Immunol. 2014; 24:298–307.
10. Brożek JL, Terracciano L, Hsu J, Kreis J, Compalati E, Santesso N, et al. Oral immunotherapy for IgE-mediated cow's milk allergy: a systematic review and meta-analysis. Clin Exp Allergy. 2012; 42:363–374.
11. Pajno GB. Oral desensitization for milk allergy in children: state of the art. Curr Opin Allergy Clin Immunol. 2011; 11:560–564.
12. Sopo SM, Onesimo R, Giorgio V, Fundarò C. Specific oral tolerance induction (SOTI) in pediatric age: clinical research or just routine practice? Pediatr Allergy Immunol. 2010; 21:e446–e449.
13. Keet CA, Seopaul S, Knorr S, Narisety S, Skripak J, Wood RA. Long-term follow-up of oral immunotherapy for cow's milk allergy. J Allergy Clin Immunol. 2013; 132:737–739.e6.
14. Savilahti EM, Kuitunen M, Savilahti E, Mäkelä MJ. Specific antibodies in oral immunotherapy for cow's milk allergy: kinetics and prediction of clinical outcome. Int Arch Allergy Immunol. 2014; 164:32–39.
15. Pajno GB, Caminiti L, Salzano G, Crisafulli G, Aversa T, Messina MF, et al. Comparison between two maintenance feeding regimens after successful cow's milk oral desensitization. Pediatr Allergy Immunol. 2013; 24:376–381.
16. Lee JH, Kim WS, Kim H, Hahn YS. Increased cow's milk protein-specific IgG4 levels after oral desensitization in 7- to 12-month-old infants. Ann Allergy Asthma Immunol. 2013; 111:523–528.
17. Skripak JM, Nash SD, Rowley H, Brereton NH, Oh S, Hamilton RG, et al. A randomized, double-blind, placebo-controlled study of milk oral immunotherapy for cow's milk allergy. J Allergy Clin Immunol. 2008; 122:1154–1160.
18. Longo G, Barbi E, Berti I, Meneghetti R, Pittalis A, Ronfani L, et al. Specific oral tolerance induction in children with very severe cow's milk-induced reactions. J Allergy Clin Immunol. 2008; 121:343–347.
19. García-Ara C, Pedrosa M, Belver MT, Martín-Muñoz MF, Quirce S, Boyano-Martínez T. Efficacy and safety of oral desensitization in children with cow's milk allergy according to their serum specific IgE level. Ann Allergy Asthma Immunol. 2013; 110:290–294.
20. Pajno GB, Caminiti L, Ruggeri P, De Luca R, Vita D, La Rosa M, et al. Oral immunotherapy for cow's milk allergy with a weekly up-dosing regimen: a randomized single-blind controlled study. Ann Allergy Asthma Immunol. 2010; 105:376–381.
21. Bedoret D, Singh AK, Shaw V, Hoyte EG, Hamilton R, DeKruyff RH, et al. Changes in antigen-specific T-cell number and function during oral desensitization in cow's milk allergy enabled with omalizumab. Mucosal Immunol. 2012; 5:267–276.
22. Clark AT, Ewan PW. Food allergy in childhood. Arch Dis Child. 2003; 88:79–81.
23. González Jiménez D, Larrea Tamayo E, Díaz Martin JJ, Molinos Norniella C, Pérez Solis D, Menéndez Arias C, et al. Eficacia y seguridad de una pauta rush de inducción de tolerancia oral en pacientes con alergia a proteínas de leche de vaca: evolución clínica e inmunológica). An Pediatr (Barc). 2013; 79:346–351.
24. Vázquez-Ortiz M, Alvaro-Lozano M, Alsina L, Garcia-Paba MB, Piquer-Gibert M, Giner-Muñoz MT, et al. Safety and predictors of adverse events during oral immunotherapy for milk allergy: severity of reaction at oral challenge, specific IgE and prick test. Clin Exp Allergy. 2013; 43:92–102.
25. Meglio P, Bartone E, Plantamura M, Arabito E, Giampietro PG. A protocol for oral desensitization in children with IgE-mediated cow's milk allergy. Allergy. 2004; 59:980–987.
26. Alonso-Lebrero E, Fuentes V, Zapatero L, Pérez-Bustamante S, Pineda F, Martinez-Molero MI. Goat's milk allergies in children following specific oral tolerance induction to cow's milk. Allergol Immunopathol (Madr). 2008; 36:180–181.
27. Tripodi S, Comberiati P, Di Rienzo Businco A, Bianchi A, Bondanini F, Sargentini V, et al. Severe anaphylaxis to sheep's milk cheese in a child desensitized to cow's milk through specific oral tolerance induction. Eur Ann Allergy Clin Immunol. 2013; 45:56–60.
28. Rodríguez del Río P, Sánchez-García S, Escudero C, Pastor-Vargas C, Sánchez Hernández JJ, Pérez-Rangel I, et al. Allergy to goat's and sheep's milk in a population of cow's milk-allergic children treated with oral immunotherapy. Pediatr Allergy Immunol. 2012; 23:128–132.
29. Sánchez-García S, Rodríguez del Río P, Escudero C, García-Fernández C, Ramirez A, Ibáñez MD. Efficacy of oral immunotherapy protocol for specific oral tolerance induction in children with cow's milk allergy. Isr Med Assoc J. 2012; 14:43–47.
30. Zapatero L, Alonso E, Fuentes V, Martínez MI. Oral desensitization in children with cow's milk allergy. J Investig Allergol Clin Immunol. 2008; 18:389–396.
31. Staden U, Rolinck-Werninghaus C, Brewe F, Wahn U, Niggemann B, Beyer K. Specific oral tolerance induction in food allergy in children: efficacy and clinical patterns of reaction. Allergy. 2007; 62:1261–1269.
32. Perezábad L, Reche M, Valbuena T, López-Fandiño R, Molina E, López-Expósito I. Clinical efficacy and immunological changes subjacent to egg oral immunotherapy. Ann Allergy Asthma Immunol. 2015; 114:504–509.
33. Meglio P, Giampietro PG, Carello R, Gabriele I, Avitabile S, Galli E. Oral food desensitization in children with IgE-mediated hen's egg allergy: a new protocol with raw hen's egg. Pediatr Allergy Immunol. 2013; 24:75–83.
34. Narisety SD, Skripak JM, Steele P, Hamilton RG, Matsui EC, Burks AW, et al. Open-label maintenance after milk oral immunotherapy for IgE-mediated cow's milk allergy. J Allergy Clin Immunol. 2009; 124:610–612.
35. Wood RA, Sicherer SH, Vickery BP, Jones SM, Liu AH, Fleischer DM, et al. The natural history of milk allergy in an observational cohort. J Allergy Clin Immunol. 2013; 131:805–812.
36. Elizur A, Rajuan N, Goldberg MR, Leshno M, Cohen A, Katz Y. Natural course and risk factors for persistence of IgE-mediated cow's milk allergy. J Pediatr. 2012; 161:482–487.e1.
37. Fiocchi A, Terracciano L, Bouygue GR, Veglia F, Sarratud T, Martelli A, et al. Incremental prognostic factors associated with cow's milk allergy outcomes in infant and child referrals: the Milan Cow's Milk Allergy Cohort study. Ann Allergy Asthma Immunol. 2008; 101:166–173.
38. Meglio P, Giampietro PG, Gianni S, Galli E. Oral desensitization in children with immunoglobulin E-mediated cow's milk allergy--follow-up at 4 yr and 8 months. Pediatr Allergy Immunol. 2008; 19:412–419.
39. Savilahti EM, Rantanen V, Lin JS, Karinen S, Saarinen KM, Goldis M, et al. Early recovery from cow's milk allergy is associated with decreasing IgE and increasing IgG4 binding to cow's milk epitopes. J Allergy Clin Immunol. 2010; 125:1315–1321.e9.
40. Alvaro M, Giner MT, Vázquez M, Lozano J, Domínguez O, Piquer M, et al. Specific oral desensitization in children with IgE-mediated cow's milk allergy. Evolution in one year. Eur J Pediatr. 2012; 171:1389–1395.
41. Tsuge I, Kondo Y, Tokuda R, Kakami M, Kawamura M, Nakajima Y, et al. Allergen-specific helper T cell response in patients with cow's milk allergy: simultaneous analysis of proliferation and cytokine production by carboxyfluorescein succinimidyl ester dilution assay. Clin Exp Allergy. 2006; 36:1538–1545.
42. Tiemessen MM, Van Ieperen-Van Dijk AG, Bruijnzeel-Koomen CA, Garssen J, Knol EF, Van Hoffen E. Cow's milk-specific T-cell reactivity of children with and without persistent cow's milk allergy: key role for IL-10. J Allergy Clin Immunol. 2004; 113:932–939.
43. Michaud B, Aroulandom J, Baiz N, Amat F, Gouvis-Echraghi R, Candon S, et al. Casein-specific IL-4- and IL-13-secreting T cells: a tool to implement diagnosis of cow's milk allergy. Allergy. 2014; 69:1473–1480.
44. Shek LP, Bardina L, Castro R, Sampson HA, Beyer K. Humoral and cellular responses to cow milk proteins in patients with milk-induced IgE-mediated and non-IgE-mediated disorders. Allergy. 2005; 60:912–919.
45. Sletten GB, Halvorsen R, Egaas E, Halstensen TS. Memory T cell proliferation in cow's milk allergy after CD25+ regulatory T cell removal suggests a role for casein-specific cellular immunity in IgE-mediated but not in non-IgE-mediated cow's milk allergy. Int Arch Allergy Immunol. 2007; 142:190–198.
46. Vickery BP, Pons L, Kulis M, Steele P, Jones SM, Burks AW. Individualized IgE-based dosing of egg oral immunotherapy and the development of tolerance. Ann Allergy Asthma Immunol. 2010; 105:444–450.
47. Jones SM, Pons L, Roberts JL, Scurlock AM, Perry TT, Kulis M, et al. Clinical efficacy and immune regulation with peanut oral immunotherapy. J Allergy Clin Immunol. 2009; 124:292–300.
48. Akdis CA, Blesken T, Akdis M, Wüthrich B, Blaser K. Role of interleukin 10 in specific immunotherapy. J Clin Invest. 1998; 102:98–106.
49. Shreffler WG, Wanich N, Moloney M, Nowak-Wegrzyn A, Sampson HA. Association of allergen-specific regulatory T cells with the onset of clinical tolerance to milk protein. J Allergy Clin Immunol. 2009; 123:43–52.e7.
50. Varshney P, Jones SM, Scurlock AM, Perry TT, Kemper A, Steele P, et al. A randomized controlled study of peanut oral immunotherapy: clinical desensitization and modulation of the allergic response. J Allergy Clin Immunol. 2011; 127:654–660.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download