Abstract
Purpose
There have been conflicting reports concerning the relationship between breast-feeding and the development of atopic dermatitis (AD) in early childhood. The objective of this study was to investigate the associations between breast-feeding and the risk of AD in early childhood in Korea.
Methods
We combined the fourth and fifth Korea National Health and Nutrition Examination Survey data collected from 2007 to 2012 and analyzed 2,015 children at 1 to 3 years old. Regression analysis was used to determine the association of the following variables: AD, feeding types, duration of breast-feeding, and others.
Results
The annual prevalence of exclusive breast-feeding and AD decreased. Parents with allergic diseases preferred breast-feeding and extended duration of feeding compared with those without. In multiple logistic regression analyses, exclusive breast-feeding in feeding type I (P=0.070; adjusted odds ratio [OR]=1.990), exclusive breast-feeding in feeding type II (P=0.095; adjusted OR=1.495) and breast-feeding duration (P=0.430; adjusted OR=1.013) were not significantly related to AD.
Conclusions
Breast-feeding was not found to be associated with an occurrence of AD in young children. Rather, parents with histories of allergic diseases tended to prefer breast-feeding and extend its duration. To clarify the role of breast-feeding in the development of AD, a nation-wide prospective study is needed.
Atopic dermatitis (AD) begins in early childhood, and 60% of the cases develop in children before 2 years of age.1 It has distinctive chronicity and is the gateway of atopic march.2 To reduce potential public health implications, intervention for the prevention of AD has been considered.2
Breast-feeding is commonly known as a preventive factor against the development of allergic diseases including AD.3 However, recent studies demonstrated that breast-feeding does not have a protective effect against AD but actually increases the risk of AD.45 In Korean studies, there were also conflicting results, and a recent report in 2014 indicated that breast-feeding was associated with the risk of AD in children less than 5 years old.6 Many studies have shown that the protective effect of breast-feeding against AD is controversial. It could be a result of differences in study design (including sample size and region).7
This study investigated the association between breast-feeding and AD in young Korean children from data based on the fourth and fifth Korea National Health and Nutrition Examination Survey (KNHANES IV and V) collected from 2007 to 2012.
The present study is based on the data of the KNHANES IV and V from 2007 to 2012. The KNHANES was an annual cross-sectional representative survey in the non-institutionalized Korean population. The survey included a health interview, a nutrition survey, and a physical examination. Specially trained interviewers or examiners who were not provided with any prior information about participants conducted the survey. The KNHANES used a rolling sample design with complex, stratified, and multistage probability sampling to extract the representative households in Korea.89
The KNHANES was approved by the Institutional Review Board of Korea Centers for Disease Control and Prevention (2007-02CON-04-P, 2008-04EXP-01-C, 2009-01CON-03-2C, 2010-02CON-21-C, 2011-02CON-06-C, 2012-01EXP-01-2C)9. All participants in the survey signed an informed consent form. From 2007 to 2012, 50,404 individuals participated in the KNHANES (detailed information about KNHANES: http://khanes.cdc.go.kr/). Among the participants, 2,015 at 1 to 3 years old were selected (196 in 2007, 393 in 2008, 415 in 2009, 363 in 2010, 351 in 2011, and 297 in 2012, respectively).
This study was exempt from IRB review by the Institutional Review Boards of Kyung Hee University Hospital at Gangdong (KHNMC 2014-11-024).
Participants were determined as having AD when they answered the survey question “AD diagnosed by a doctor” affirmatively. Exclusive breast-feeding is a feeding type by breast milk only without other liquids or solids except for drops or syrups consisting of vitamins, mineral supplements, or medications.10 Participants were classified as “exclusive breast-feeding” when they answered “yes” to the survey question “whether breast-feeding or not” but “no” to the survey question “whether formula-feeding or not.”11 Participants were categorized as “exclusive formula-feeding” when they answered “no” to the survey question “whether breast-feeding or not” but “yes” to the survey question “whether formula-feeding or not.”11 The “mixed feeding” group was made up of participants who answered “yes” to the survey questions “whether breast-feeding or not” and “whether formula-feeding or not.”11 Participants were classified as “formula-feeding” when they answered “yes” to the survey question “whether formula-feeding or not” regardless of breast-feeding.11 To analyze the effects of feeding types, we performed 2-type analyses for 2 feeding types. In analysis of feeding type I, feeding formulas were classified into exclusive breast-feeding, exclusive formula-feeding, and mixed feeding.11 In the analysis of feeding type II, feedings were defined as exclusive breast-feeding and formula-feeding.11 Positive history of parental allergic diseases was determined when one parent answered “yes” to one of the following survey questions: “asthma diagnosed by a doctor,” “allergic rhinitis diagnosed by a doctor,” or “AD diagnosed by a doctor.”
The age, sex, body mass index (BMI), residence, family size, familial income quartile, birth weight, current wheezing, onset-time of weaning, and breast-feeding duration of participants were also surveyed.
All statistical analyses were performed using IBM SPSS ver. 21.0 (IBM Co., Armonk, NY, USA) to evaluate the stratified cluster sampling design survey. All results are presented as weighted values.9
Study weight=(weight of 2007 year/11)+(weight of 2008 year/5.5)+(weight of 2009 year/5.5)+(weight of 2010 year/5.5) (weight of 2011 year/5.5)+(weight of 2012 year /5.5)
Categorical variables are presented as proportions (percentages), and continuous variables are presented as means (±standard error [SE]).
The χ2 test and t test were used to make a comparison between children with AD and those without and to examine proportions of feeding patterns and duration of feeding in relation to history of parental allergic diseases.
To evaluate the association between the types of feeding and AD prevalence, we utilized multiple logistic regression analysis. Adjustments of AD were achieved for feeding type I, an analysis of exclusive breast-feeding and mixed-feeding, by using exclusive formula-feeding as the reference group. Adjustments were also made for feeding type II, an analysis of exclusive breast-feeding made by using formula-feeding as the reference group. Multiple logistic regression analysis was also adjusted by feeding duration with other variables including age, sex, residence, members of household, familial income quartile, birth weight, history of parental allergic diseases, current wheezing, and start time of weaning.
The Characteristics of the participants are shown in Table 1. The age (mean±SE) was 1.98±0.02 years, and 51.6% of the participants were male. Five hundred sixty-five (29.1%) participants were exclusively breast-fed, 202 (11.3%) were exclusively formula-fed, and 1,134 (59.7%) had mixed feeding patterns; feeding duration (mean±SE) was 9.87±0.21 months. The rates of positive parental allergic history (P<0.001) and exclusive breast-feeding (P=0.037, 0.036, respectively) were greater in children with AD than in those without. Onset time of weaning, duration of breast-feeding, and current wheezing were not significantly different between the 2 groups.
Data from surveys collected from 2007 to 2012 demonstrate that the prevalence of AD decreased from 18.2% in 2008 and reached the lowest rate of 8.8% in 2011 but slightly increased to 10.7% in 2012 (Figure). Since 2009, the percentage of exclusive breast-feeding has steadily decreased from 35.6% to 23.1% (Figure). The proportion of breast-feeding, including mixed feeding, has not been significantly altered so far.
Feeding types and breast-feeding duration were analyzed in relation to the history of parental allergic diseases (Table 2). Parents with allergic diseases favored breast-feeding in the analysis of feeding type II. In addition, parents with allergic diseases also preferred breast-feeding for an extended duration in comparison with those without (11.06±0.50 months vs 9.93±0.27 months) (Table 2). The relation between feeding types and AD was analyzed according to parental allergic history (Supplementary Table). Regardless of parental allergic history, all feeding-patterns did not significantly differ between the prevalence rate of AD and non-AD.
Exclusive breast-feeding was a significant risk factor for AD in feeding type I (P=0.043; crude odds ratio [OR], 1.882; 95% confidence interval [CI], 1.020-3.475) by univariate logistic regression. In a multiple logistic regression analyses, however, exclusive breast-feeding in feeding type I (P=0.070; adjusted OR, 1.990; 95% CI, 0.946-4.187), exclusive breast-feeding in feeding type II (P=0.095; adjusted OR, 1.495; 95% CI, 0.932-2.398), and breast-feeding duration (P=0.430; adjusted OR, 1.013; 95% CI, 0.981-1.047) were not significantly related to AD (Table 3).
This study used a sample from the KNHANES from 2007 to 2012, regarding it as being representative of Korean children. This is the first study that investigated the relationship between breast-feeding and the prevalence rates of AD using the KNHANES, Korean national representative data, to our knowledge.
In crude logistic regression analysis, exclusive breast-feeding was not associated with the development of AD in early childhood, and multiple regression analysis showed the definite disconnection between breast-feeding and the prevalence of AD. Furthermore, parents with histories of allergic diseases were significantly more likely to exclusively breast-feed and to prolong breast-feeding than parents without allergic diseases. This shows that breast-feeding and prolonged duration of breast-feeding did not prevent AD in young Korean children from 1 to 3 years of age.
Breast-feeding has long been believed to be an effective method in the prevention of allergic diseases including AD.312 The European Academy of Allergy and Clinical Immunology recommended exclusive breast-feeding during 4-6 months and the American Academy of Pediatrics also announced that exclusive breast-feeding for 3 to 4 months had a protective effect against allergic disease.313 For example, the incidence of clinical asthma was reduced by 27% in a low-risk population, and the risk of AD was lowered by as much as 42% in infants with a positive family history of the conditions in their policy statement.314 A study of a birth cohort with 4,089 children concluded that breast-feeding longer than 4 months reduces the development of eczema and allergy march for children up to 4 years-of-age.12 A meta-analysis reported that exclusive breast-feeding during the first 3 months of life could significantly reduce incidence rates of AD in children with a family history of atopy (OR=0.58; 95% CI, 0.41–0.92).15 These findings can explain why parents with allergic diseases prefer breast milk to formula as indicated in our research.
Breast milk has an immunomodulatory effect that enhances the immune system and defends infants from infection and the development of atopy.15 Glycans (complex carbohydrates) modulate mucosal immunity, and transforming growth factor (TGF)-β and interleukin (IL)-6 in human milk are considered to be more involved in immunoglobulin A (IgA) synthesis than those in formula milk.1617 Infants with breast-feeding exclusively for 4 months and partially after that time were reduced risks of infections in gastrointestinal tract infection, and the upper and lower respiratory tract infections.318 Breast-feeding could protect the development of AD from possible factors such as infection.151920 Consequently, the World Health Organization encourages mothers to breast-feed exclusively for 6 months.21
Recently, many researchers expressed doubts about protective effects of breast-feeding against AD.45222324 Cochrane review concluded that exclusive breast-feeding beyond 3 to 4 months does not reduce the risk of atopic eczema, asthma, or other atopic outcomes in studies from Finland, Australia, and Belarus, nor does it seem to lead to any additional reductions in the incidence of atopic eczema.25 As a result, the policy statement by the American Academy of Pediatrics on the protective effect of exclusive breast-feeding against AD was viewed as being based on poor evidence.26 According to a cohort study from Sweden in 2005, exclusive breast-feeding did not relate to the risk of AD within 1 year of life regardless of familial history of atopic diseases.22 Jelding-Dannemand et al.27 reported that exclusive breast-feeding had no protective effect against the development of AD at 7 years of age in a cohort study, even if adjusting for reverse causation.
Furthermore, there are several reports claiming that breast-feeding is a risk factor of AD.452324 A birth cohort study of high-risk infants concluded that the risk of eczema increased in infants with long breast-feeding duration (relative risk, 2.09; 95% CI, 1.15–3.80).4 A nationwide Japanese birth cohort study reported that exclusively breast-fed children had a higher incidence of AD up to the age of 42 months compared to those who were formula-fed (OR, 1.26; 95% CI, 1.12-1.41), and breast-feeding duration was strongly associated with the incidence of AD (P for trend <0.001).5 Prolonged breast-feeding longer than 9 months was associated with AD in a 20-year follow-up cohort.24 The case control study showed that after adjustment for parental atopy, breast-feeding increased the risk of AD.23 From an immunologic perspective, there were differences in cytokines in breast milk between allergic mothers and mothers without allergies. The TGF-β levels were lower in allergic mothers than in non-allergic mothers with mature breast milk.2829 TGF-β is one of the immune-modulating cytokines, play an important role in the immune response in growing infants.30 Additionally, environmental pollution chemicals in breast milk may influence development of allergic disease.3132 Persistent organic pollutants (POPs), such as dioxins and polychlorinated biphenyls (PCBs), can influence infants' health such as growth as well as endocrine, neurodevelopmental, and immunologic outcomes.31 A cohort study in the Faroe Islands from 1999-2001 found that serum total immunoglobulin E (IgE) in children 7 years old was correlated with the PCB concentration in serum and the breast-feeding duration.33 Another Japanese study found maternal fish intake to be associated with AD.5 Because fish contains PCBs that can be transferred to breast milk and disturb normal immune functioning, breast-feeding may transmit PCB to the infant.5 Those recent studies are in agreement with the authors' results that exclusive breast-feeding is connected to the development of AD in young children.
This study is a cross-sectional study and has some limitations. First, it may be inappropriate to establish a casual relationship between breast-feeding and the prevention of AD in spite of the fact that the KNHANES collected data year-round to overcome the limitations of a cross-sectional study. Secondly, reverse causation also affected our result because we could not exclude children who developed AD during exclusive breast-feeding from the KNHANES data. However, since our results on prevalence is similar to those of another study conducted to determine the prevalence of AD in 2 years olds,34 the KNHANES seems to be a valid survey. In our results, the information was based on the interview and not-self-reported questionnaire administered by personnel trained for the KNHANES. Taking these factors into consideration, it is an appropriate study to analyze the association between breast-feeding and the prevalence of AD in young children from the Korean national representative data.
In conclusion, breast-feeding is not associated with the occurrence of AD in children up to 3 years old in Korea regardless of familial allergy history as found using the KNHANES IV, V (2007–2012). National prospective studies are needed to clarify the role of breast-feeding and the mechanism behind breast milk's effects in the development of AD.
ACKNOWLEDGMENTS
We are thankful to the Korea Center for Disease Control and Prevention (KCDC) as the research data were based on the “Korea National Health and Nutrition Examination Survey” (KNHANES) by the KCDC (Statistics Korea's confirmation number: 11758). Because data from the KNHANES were publicly accessible, we did not require the permission of the KCDC for research and publishing purposes. The study was presented by poster in the 2015 American Academy of Allergy, Asthma, and Immunology (AAAAI) annual meeting (Journal of Allergy and Clinical Immunology, Vol. 135, Issue 2, AB263).
References
1. Bieber T. Atopic dermatitis 2.0: from the clinical phenotype to the molecular taxonomy and stratified medicine. Allergy. 2012; 67:1475–1482. PMID: 23106343.

2. Dharmage SC, Lowe AJ, Matheson MC, Burgess JA, Allen KJ, Abramson MJ. Atopic dermatitis and the atopic march revisited. Allergy. 2014; 69:17–27. PMID: 24117677.

3. Section on Breastfeeding. Breastfeeding and the use of human milk. Pediatrics. 2012; 129:e827–e841. PMID: 22371471.
4. Giwercman C, Halkjaer LB, Jensen SM, Bønnelykke K, Lauritzen L, Bisgaard H. Increased risk of eczema but reduced risk of early wheezy disorder from exclusive breast-feeding in high-risk infants. J Allergy Clin Immunol. 2010; 125:866–871. PMID: 20236698.

5. Ito J, Fujiwara T. Breastfeeding and risk of atopic dermatitis up to the age 42 months: a birth cohort study in Japan. Ann Epidemiol. 2014; 24:267–272. PMID: 24342028.

6. Hong S, Choi WJ, Kwon HJ, Cho YH, Yum HY, Son DK. Effect of prolonged breast-feeding on risk of atopic dermatitis in early childhood. Allergy Asthma Proc. 2014; 35:66–70. PMID: 24433599.

7. Yang YW, Tsai CL, Lu CY. Exclusive breastfeeding and incident atopic dermatitis in childhood: a systematic review and meta-analysis of prospective cohort studies. Br J Dermatol. 2009; 161:373–383. PMID: 19239469.

8. Kim HJ, Kim Y, Cho Y, Jun B, Oh KW. Trends in the prevalence of major cardiovascular disease risk factors among Korean adults: results from the Korea National Health and Nutrition Examination Survey, 1998-2012. Int J Cardiol. 2014; 174:64–72. PMID: 24742812.

9. Ministry of Health and Welfare, Korea Centers for Disease Control and Prevention. Korea National Health and Nutrition Examination Survey [Internet]. Sejong: Korea Centers for Disease Control and Prevention;2016. 2016 May 29. Available from: https://knhanes.cdc.go.kr/knhanes/index.do.
10. Kim MJ, Kim YM, Yoo JH. Factors affecting exclusive breast-feeding during the first 6 months in Korea. Pediatr Int. 2013; 55:177–180. PMID: 23110585.

11. Lee KS, Choi SH, Choi YS, Oh IH, Rha YH. Relationship between breast-feeding and wheeze risk in early childhood in Korean children: based on the fifth Korea National Health and Nutrition Examination Survey 2010-2012. Allergy Asthma Respir Dis. 2014; 2:103–107.

12. Kull I, Böhme M, Wahlgren CF, Nordvall L, Pershagen G, Wickman M. Breast-feeding reduces the risk for childhood eczema. J Allergy Clin Immunol. 2005; 116:657–661. PMID: 16159639.

13. Muraro A, Halken S, Arshad SH, Beyer K, Dubois AE, Du Toit G, et al. EAACI food allergy and anaphylaxis guidelines. Primary prevention of food allergy. Allergy. 2014; 69:590–601. PMID: 24697491.

14. Ip S, Chung M, Raman G, Chew P, Magula N, DeVine D, et al. Breastfeeding and maternal and infant health outcomes in developed countries. Evid Rep Technol Assess (Full Rep). 2007; 1–186.
15. Gdalevich M, Mimouni D, David M, Mimouni M. Breast-feeding and the onset of atopic dermatitis in childhood: a systematic review and meta-analysis of prospective studies. J Am Acad Dermatol. 2001; 45:520–527. PMID: 11568741.

16. Iyengar SR, Walker WA. Immune factors in breast milk and the development of atopic disease. J Pediatr Gastroenterol Nutr. 2012; 55:641–647. PMID: 22684347.

17. Newburg DS, Walker WA. Protection of the neonate by the innate immune system of developing gut and of human milk. Pediatr Res. 2007; 61:2–8. PMID: 17211132.

18. Duijts L, Jaddoe VW, Hofman A, Moll HA. Prolonged and exclusive breastfeeding reduces the risk of infectious diseases in infancy. Pediatrics. 2010; 126:e18–e25. PMID: 20566605.

19. Frick OL, German DF, Mills J. Development of allergy in children. I. Association with virus infections. J Allergy Clin Immunol. 1979; 63:228–241. PMID: 85648.
20. Penders J, Thijs C, van den Brandt PA, Kummeling I, Snijders B, Stelma F, et al. Gut microbiota composition and development of atopic manifestations in infancy: the KOALA Birth Cohort Study. Gut. 2007; 56:661–667. PMID: 17047098.

21. World Health Organization. Breastfeeding [Internet]. Geneva: World Health Organization;2016. 2016 May 29. Available from: http://www.who.Int/topics/breastfeeding/en/.
22. Ludvigsson JF, Mostrom M, Ludvigsson J, Duchen K. Exclusive breastfeeding and risk of atopic dermatitis in some 8300 infants. Pediatr Allergy Immunol. 2005; 16:201–208. PMID: 15853948.

23. Purvis DJ, Thompson JM, Clark PM, Robinson E, Black PN, Wild CJ, et al. Risk factors for atopic dermatitis in New Zealand children at 3.5 years of age. Br J Dermatol. 2005; 152:742–749. PMID: 15840107.

24. Pesonen M, Kallio MJ, Ranki A, Siimes MA. Prolonged exclusive breastfeeding is associated with increased atopic dermatitis: a prospective follow-up study of unselected healthy newborns from birth to age 20 years. Clin Exp Allergy. 2006; 36:1011–1018. PMID: 16911357.

25. Kramer MS, Kakuma R. Optimal duration of exclusive breastfeeding. Cochrane Database Syst Rev. 2012; CD003517. PMID: 22895934.

27. Jelding-Dannemand E, Malby Schoos AM, Bisgaard H. Breast-feeding does not protect against allergic sensitization in early childhood and allergy-associated disease at age 7 years. J Allergy Clin Immunol. 2015; 136:1302–1308.e1-13. PMID: 25843315.

28. Rigotti E, Piacentini GL, Ress M, Pigozzi R, Boner AL, Peroni DG. Transforming growth factor-beta and interleukin-10 in breast milk and development of atopic diseases in infants. Clin Exp Allergy. 2006; 36:614–618. PMID: 16650046.
29. Böttcher MF, Jenmalm MC, Björkstén B, Garofalo RP. Chemoattractant factors in breast milk from allergic and nonallergic mothers. Pediatr Res. 2000; 47:592–597. PMID: 10813582.

30. Penttila IA. Milk-derived transforming growth factor-beta and the infant immune response. J Pediatr. 2010; 156:S21–S25. PMID: 20105660.
31. Nickerson K. Environmental contaminants in breast milk. J Midwifery Womens Health. 2006; 51:26–34. PMID: 16399607.

32. Nagayama J, Tsuji H, Iida T, Nakagawa R, Matsueda T, Hirakawa H, et al. Immunologic effects of perinatal exposure to dioxins, PCBs and organochlorine pesticides in Japanese infants. Chemosphere. 2007; 67:S393–S398. PMID: 17222440.

33. Grandjean P, Poulsen LK, Heilmann C, Steuerwald U, Weihe P. Allergy and sensitization during childhood associated with prenatal and lactational exposure to marine pollutants. Environ Health Perspect. 2010; 118:1429–1433. PMID: 20562055.

34. Smidesang I, Saunes M, Storrø O, Øien T, Holmen TL, Johnsen R, et al. Atopic dermatitis among 2-year olds; high prevalence, but predominantly mild disease--the PACT study, Norway. Pediatr Dermatol. 2008; 25:13–18. PMID: 18304146.

SUPPLEMENTARY MATERIAL
Supplementary Table
Cross-table analysis between feeding types and AD according to parental allergic history
Figure
Changes in the proportion of AD and exclusive breast-feeding in children at 1 to 3 years of age (KNHANES-IV and V, 2007-2012). This survey was conducted by Korea Centers for Disease Control and Prevention to evaluate Korean health and nutrition (KNHANES-IV: from 2007 to 2009, KNHANES-V: from 2010 to 2012). AD, atopic dermatitis; KNHANES-IV and V, The fourth and fifth Korea National Health and Nutrition Examination Survey.
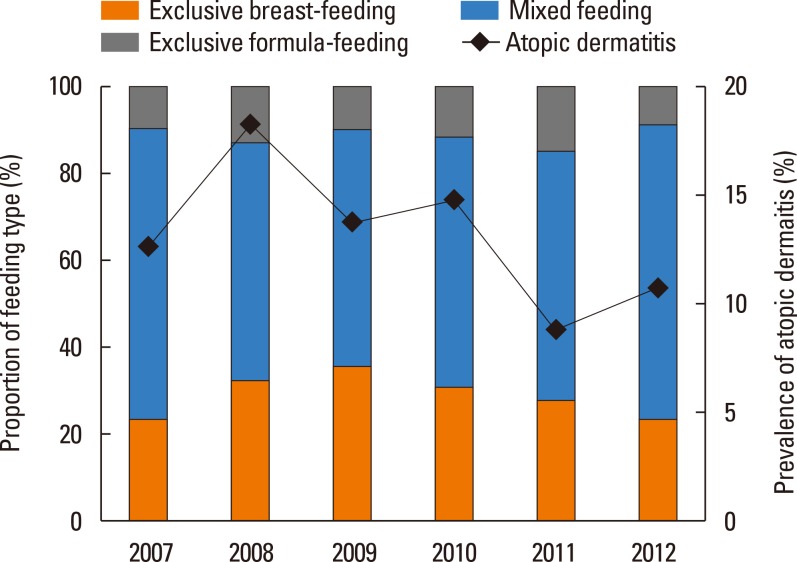
Table 1
Characteristics of the subjects at 1 to 3 years of age (KNHANES-IV and V, 2007–2012)
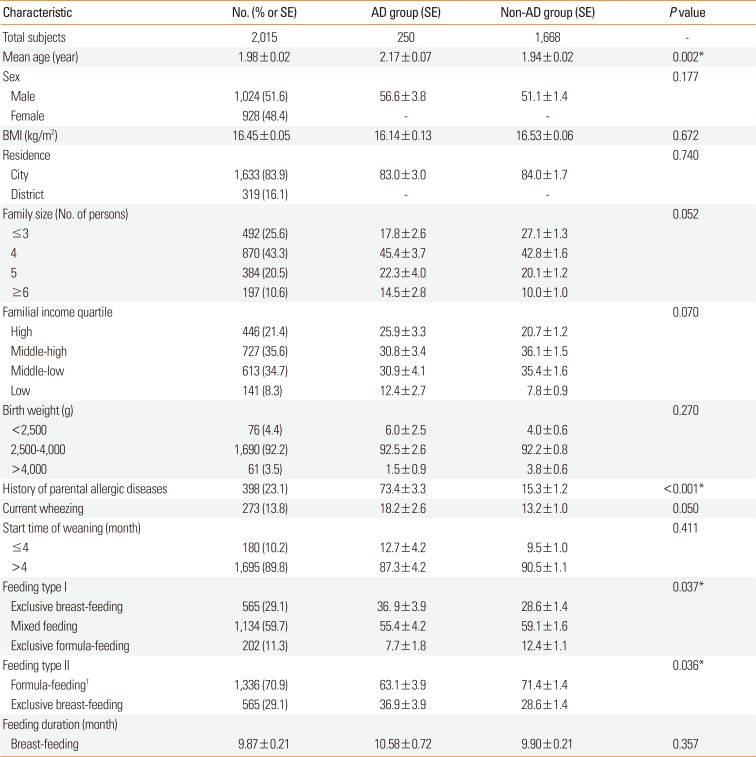
Table 2
Differences in the type and duration of feeding via history of parental allergic diseases
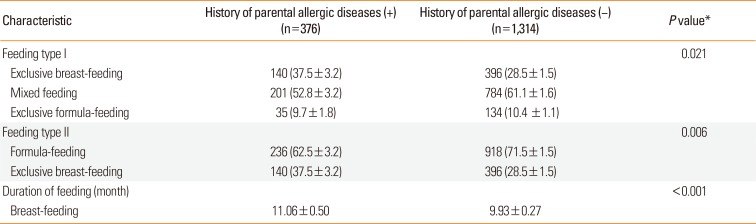
Table 3
Crude and adjusted ORs of AD (at 1 to 3 years of age, KNHANES-IV and V, 2007-2012)
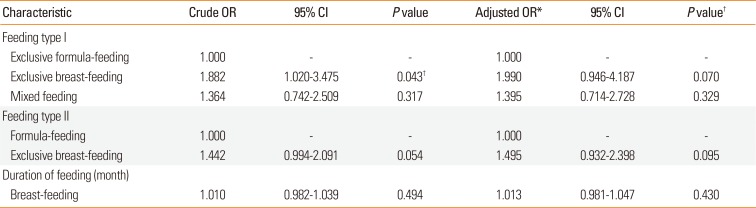
AD, atopic dermatitis; OR, odds ratio; CI, confidence interval; KNHANES-VI and V, The fourth and fifth Korea National Health and Nutrition Examination Survey.
*Adjusted by age, sex, residence, family size, familial income quartile, birth weight, current wheezing, start time of weaning, and history of parental allergic diseases; †P<0.050.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download